Abstract
Sub-inhibitory concentrations of antibiotics are always generated as a consequence of antimicrobial therapy and the effects of such residual products in bacterial morphology are well documented, especially the filamentation generated by beta-lactams. The aim of this study was to investigate some morphological and pathological aspects (virulence factors) of Escherichia coli cultivated under half-minimum inhibitory concentration (1.0 µg/mL) of piperacillin–tazobactam (PTZ sub-MIC). PTZ sub-MIC promoted noticeable changes in the bacterial cells which reach the peak of morphological alterations (filamentation) and complexity at 16 h of antimicrobial exposure. Thereafter the filamentous cells and a control one, not treated with PTZ, were comparatively tested for growth curve; biochemical profile; oxidative stress tolerance; biofilm production and cell hydrophobicity; motility and pathogenicity in vivo. PTZ sub-MIC attenuated the E. coli growth rate, but without changes in carbohydrate fermentation or in traditional biochemical tests. Overall, the treatment of E. coli with sub-MIC of PTZ generated filamentous forms which were accompanied by the inhibition of virulence factors such as the oxidative stress response, biofilm formation, cell surface hydrophobicity, and motility. These results are consistent with the reduced pathogenicity observed for the filamentous E. coli in the murine model of intra-abdominal infection. In other words, the treatment of E. coli with sub-MIC of PTZ suggests a decrease in their virulence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The therapeutic concentrations of antimicrobial agents used in vivo are always followed by sub-inhibitory concentrations (sub-MIC; MIC: minimal inhibitory concentration). Once antimicrobials are used in various sectors of human activity, such as farming, ranching, fish farming, and the food industry, as a result, environmental microorganisms are exposed to a range of antimicrobials at sub-MIC. The effects of sub-MIC of antimicrobial agents have been the subject of many studies over time [1–7].
Antimicrobial agents at sub-MIC have been implicated in numerous changes in bacterial character, including morphology [8] and cell wall components [9, 10]. Accumulating evidence associates filamentation with an intended response to specific environmental cues such as innate immunity, predator sensing, quorum sensing, and antimicrobial pressure [11].
Virulence factors are also affected by sub-MIC; researchers have demonstrated alterations in enzyme and toxin production [12], changes in adhesive properties and cell surface hydrophobicity [5, 13, 14], alterations in biofilm formation [5, 15, 16], decreased motility [5], and increased susceptibility to phagocytes [17].
The effect of piperacillin, a potent broad-spectrum ureidopenicillin, on bacterial morphology was first reported in 1978 by Iida et al. that showed that growing E. coli at sub-MIC resulted in filamentation [1]. Today, piperacillin is combined with the beta-lactamase inhibitor tazobactam, expanding their activity against beta-lactamase-producing Gram-negative, Gram-positive, and anaerobic organisms. However, there are limited studies regarding the effect of sub-MIC of piperacillin–tazobactam (PTZ) and no studies concerning the effect of PTZ sub-MIC on E. coli virulence. Thus, in the present study, we examined the effect of PTZ sub-MIC on E. coli morphology and physiology. E. coli has been frequently used as a model organism in structural and functional studies aimed at understanding bacterial physiology and gene expression. The focus on E. coli is because it represents one of the most important pathogenic bacteria for both humans and animals.
Materials and Methods
E. coli Strain and Antibiotics
E. coli ATCC 25922 was used in this study. A commercial piperacillin–tazobactam preparation (Tazocin) was purchased (Lederle Piperacillin) and the antibiotic solutions were prepared according to the manufacturer’s instructions. The sub-inhibitory concentration used in all assays was 1.0 µg/mL, equivalent to half PTZ MIC (0.5 × MIC) for E. coli.
Kinetics of Morphological Changes and Preparation of Inocula
Based on a previous study in our group that showed morphological changes in E. coli treated with sub-MIC of PTZ (no published data), it was proposed to determine the progression of this change over time. Therefore, flow cytometric analysis was applied to determine the time at which 0.5 × MIC PTZ affects the majority of the bacterial population. The experiment is briefly described: Mueller–Hinton agar plates (Difco) containing 0.5 × MIC of PTZ (1 µg/mL) were inoculated with an overnight culture of E. coli adjusted to 0.5 McFarland (1.5 × 108 CFU/mL) and incubated at 37 °C. At 2, 4, 8, 12, 16, 20, 24, and 48 h post-inoculation, the cells were harvested by washing the plates with sterile phosphate buffered saline (PBS) that was then collected for centrifugation (4000 rpm, 10 min, 4 °C). After 3 rounds of centrifugation, a bacterial suspension was subjected to flow cytometry (FACScan—Becton–Dickinson). For size and complexity determination, cells were collected on the forward scatter (FSC) and side scatter (SSC), respectively, with logarithmic amplifiers for 100,000 events. A 24 h bacterial growth in Mueller–Hinton agar without antibiotic was used as a control. The percentage difference between treated groups and the control was assessed by the software WinMDI, version 2.8.
The cultures grown with and without PTZ were subjected to Gram staining for visualization of cell morphology. In parallel, to assess persistent morphological changes, filamentous cells were grown on Mueller–Hinton agar without antibiotic for 20 h and were also visualized by Gram staining.
The bacterial inocula used in the following assays were prepared by growing E. coli with 0.5 × MIC of PTZ until the majority of the bacterial population is altered morphologically. Two cultures were generated: one with filamentous cells (EcF: E. coli filamentous) and a control untreated with PTZ (EcN: E. coli normal).
Growth Curve
Growth curves were carried out according to methods from Santos [18]. Aliquots of EcN and EcF obtained as previously described were inoculated in flasks with 90 mL of Tryptic Soy Broth (TSB) with and without 0.5 × MIC PTZ until reaching an optical density (OD) of approximately 0.01 at 550 nm (Shimadzu UV 160A). Flasks were incubated at 37 °C and monitored for 12 h. At 20 min intervals, aliquots of 2 mL were aseptically withdrawn from each flask to determine the OD. Fresh TSB was used as a blank. Three to four consecutive stable points after log phase were related to the stationary phase of the bacterial growth.
Biochemical Profile
Suspensions of EcN and EcF were adjusted to 0.5 McFarland and subjected to the following biochemical tests: indole, citrate, H2S, urease, lysine decarboxylase, tryptophan deaminase, malonate, glucose utilization with production of acid and gas, esculin hydrolysis, catalase, oxidase, and sugar fermentation. Tests of malonate, esculin hydrolysis, and sugar fermentation were performed with and without 0.5 × MIC of PTZ. All tubes (except catalase and oxidase) were incubated at 37 °C for 24 h [19].
Tolerance to Oxidative Stress
Tolerance to oxidative stress was determined according to methods from Santos [20]. Suspensions of EcN and EcF were adjusted to 0.5 McFarland and spread onto Tryptic Soy Agar (TSA) plates with and without 0.5 × MIC of PTZ. Sterile paper disk filters (7 mm diameter) infused with 10 µL of 30 % H2O2 were placed on the center of the plates. After incubation for 24 h at 37 °C, the diameter of the area of growth inhibition was measured. These assays were performed in triplicate and repeated on five different days.
Biofilm Assay
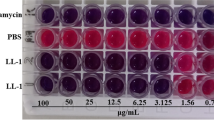
The effect of 0.5 × MIC of PTZ on E. coli biofilm formation was performed according to O’Toole et al. [21]. Suspensions of EcN and EcF were adjusted to 0.5 McFarland in brain heart infusion (BHI) broth with and without 0.5 × MIC of PTZ. Aliquots (200 µL) of these bacterial suspensions were added to wells of a 96-well microplate. After incubation for 24 h at 37 °C, adhered cells were stained with a violet crystal solution (0.1 %). The microplates were then washed three times with distilled water to remove excess dye. The remaining dye was finally solubilized by an ethanol-acetone solution (8:2) and the absorption was read on a microplate reader (Thermo Scientific—Multiskan Spectrum) at 590 nm. Each assay was performed in triplicate and repeated in five different days.
Cell Hydrophobicity
The effect of 0.5 × MIC of PTZ on the cell hydrophobicity was performed according to Fonseca et al. by microbial adhesion to hydrocarbon (MATH) assay [5]. Suspensions of EcN and EcF were adjusted to 0.5 McFarland in PBS and aliquots of 2 mL were inoculated into two different sterile tubes, one of which contained 500 µL of n-hexadecane (JT Baker). After vortexing (Daigger Vortex Genie 2) for 1 min, two phases were allowed to separate (30 min) and 1 mL of the lower aqueous phase of each tube was collected. The OD600 (Spectrum série SP—2000 UV) of aqueous extractions was read. The results were expressed as the percentage decrease in the OD of the lower aqueous phase (ODfinal) compared with the OD of the initial cell suspension (ODinitial): [1 − (ODfinal/ODinitial)] × 100. Each assay was performed in triplicate and repeated on five different days.
Motility Assay
Suspensions of EcN and EcF were adjusted to 3 McFarland (9 × 108CFU/mL) and aliquots of 5 µL (106–107 cells) were spotted on the surface of semi-solid medium to test motility (1 % Tryptone, 0.5 % NaCl, 0.3 % Bacto Agar, pH 7.1–7.3). Test were performed in media with and without 0.5 × MIC of PTZ and incubated for 6 h at 37 °C. After this time the diameter of the growth area was measured [4, 22]. This assay was performed in triplicate and repeated on five different days.
Pathogenicity in Vivo
After approval by the Ethic Committee on Animal Experimentation of the Federal University Of Minas Gerais (CETEA/UFMG—nº 107/09), female Swiss mice (7–8 weeks of age) were distributed into seven groups of six animals and intraperitoneally infected with 0.1 mL of a bacterial suspension (EcN and EcF) in PBS containing approximately 107 CFU/mL.
Animals were distributed into seven groups as follows: Group EcN1H: infection with EcN and sampling at 1 h post-inoculation; Group EcF1H, infection with EcF and sampling at 1 h post-inoculation; Group EcN3H, infection with EcN and sampling at 3 h post-inoculation; Group EcF3H, infection with EcF and sampling at 3 h post-inoculation; Group EcN6H, infection with EcN and sampling at 6 h post-inoculation; Group EcF6H, infection with EcF and sampling at 6 h post-inoculation; Group CTRL, control group inoculated with sterile PBS.
After infection, samples of blood, spleen, liver, lung, and peritoneal fluid were taken at 1, 3, or 6 h. Sampling in control animals was performed in an interval between 1 to 6 h. Blood was collected from animals anesthetised intraperitoneally (Ketamine-Xilazine) in the axillary plexus. After sacrifice of the animals by cervical dislocation, the other materials were collected. Aliquots of blood and peritoneal fluid were diluted and plated on McConkey agar. Pieces of spleen, liver, and lung were weighed, macerated, diluted, and plated on McConkey agar. Viable colonies were counted after 24 h of incubation at 37 °C.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism 5. The following statistical methods were applied when necessary. Analysis of variance (One-way ANOVA) using the Kruskal–Wallis test for nonparametric variables (P < 0.05). The Paired t test was used for mean comparison (P < 0.05).
Results and Discussion
The growth of E. coli in 0.5 × MIC of PTZ promoted noticeable changes in the bacterial cells. There was a switch from rod to filamentous shape, as first demonstrated by Iida et al. in [1] (Fig. 1). The filamentation of Gram-negative bacteria induced by beta-lactam antibiotics has been extensively reported in several studies [4–8]. It is well known that PTZ targets penicillin-binding protein 3 (PBP-3), which is responsible for cell septation during division. Thus, as reported [3, 23, 24], the bacteria continue dividing when in contact with PTZ at sub-MIC but no septation occurs due the PBP-3 inhibition, leading to generation of filamentous cells. Beta-lactamase inhibitors such as sulbactam also cause filament formation in different species of Enterobacteriaceae, due likely to your primary affinity for the PBP-1a and PBP-3 [25]. However, in E. coli, the binding affinity of tazobactam (formerly YTR 830) is mainly for the PBP-2 leading to spheroplast formation at MIC. However, tazobactam had much lower intrinsic activity (MIC 256.0 µg/ml) than clavulanic acid or sulbactam (MIC 32.0 µg/ml) against strains of the family Enterobacteriaceae [26].Thus, it is assumed that the filamentation observed in E. coli was due to the piperacillin instead tazobactam. When the bacterial population in the filamentous state was grown without antibiotic, the cells returned to their typical rod shape, indicating that the morphological change is a transient state [27]. A number of evidences associate filamentation with a mechanism of innate immunity subversion by pathogenic bacteria such as uropathogenic E. coli, predator sensing, quorum sensing, antimicrobial, and oxidative pressure response [6, 11, 28]. As stated by Lorian et al., the presence of morphologically altered bacteria may indicate sub-MIC at the site of infection and this effect on the host–microbial interaction deserves more investigation. So, to better understand the effect of such morphological changes, the kinetics of cellular alteration was first assessed using flow cytometry technology [2].
E. coli growing in the presence of 0.5 × MIC of PTZ reaches the peak of cells alterations at 16 h, with 82 % of the cells altered in morphology (FSC) and complexity (SSC) at that time (Fig. 2). Flow cytometry has been applied for the detection of morphological changes in E. coli and P. aeruginosa treated with various antimicrobial agents [29]. Likewise, Wickens et al. observed filamentous forms in 79 % of an E. coli population exposed to ciprofloxacin [30].The increase in cellular complexity can be explained by the increased amount of nucleic acid in filamentous cells due to multiple chromosomal copies from continuous replication without bacterial division [3, 29, 31]. A greater amount of cytoplasmic granules and increased roughness of the membrane can also be responsible for the increase in the SSC parameter. Thereafter, the bacterial inoculum used in the following assays was prepared from the growth of E. coli in 0.5 × MIC of PTZ for 16 h, generating two cultures: one with filamentous cells (EcF) and a control one not treated with PTZ (EcN).
Kinetics of cellular alterations of E. coli treated with 0.5 × MIC of PTZ. a Dot plot graphs of cells untreated and treated during a 48 h period. b Highlighted 16 h growth culture in which the maximum percentage (82 %) of cells with morphological alterations was observed. c Curve of cellular alteration showing the percentage of abnormal cells in relation to a 24 h growth control without PTZ. R1 area of cells with normal morphology from a growth control (without drug), R2 area of modified cells relative to the growth control, CTL control, ATB antibiotic, FSC forward scatter, and SSC side scatter
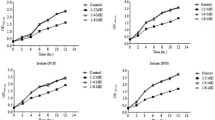
The growth curves of EcN and EcF with and without 0.5 × MIC of PTZ were constructed (pre-inoculum obtained as described) and the data showed that such treatment attenuated the bacterial growth rate, leading to a delay of 4 h in log phase of EcF and a lower cell density of EcN, both of which were treated with sub-MIC of PTZ and were compared to the control. When comparing EcN and EcF treated with PTZ, the filamentous culture (EcF) showed a delay of 5 h in log phase, although an increase in cell density, likely due to the filamentation (Fig. 3). These findings are in accordance with several authors [32–35], and Veloso et al. also reported a delay of 15 h in the log phase of an anaerobic, Gram-negative bacillus (Bacteroides fragilis) that had been exposed to sub-MIC of PTZ [36]. These authors maintained the hypothesis that the lower bacterial growth rate detected in the culture treated with 0.5 × MIC of PTZ was due to the decrease in abundance of enzymes related to energy metabolism. However, no changes in carbohydrate fermentation tests or in traditional biochemical tests have been detected in the current study. As already discussed by our group [37], these delays in bacterial growth may be a consequence of the cost that antimicrobial pressure imposes on bacterial fitness. Moreover, because the PBP-3 is an essential component for bacterial growth and PTZ inhibits this enzyme, changes in the levels of these proteins due to lower expression or inactivation could also lead to a delay in bacterial growth, which is in agreement with the work of Fang et al. [34]. Another interpretation proposed by Veloso et al. suggests that during E. coli—targeted antimicrobial therapy, a sub-MIC of PTZ could suppress bacterial growth in a phenomenon known as the post-antibiotic effect [36]. This effect may encompass all the propositions listed above.
Effect of PTZ Sub-MIC on the Oxidative Stress Tolerance
The tolerance to oxidative stress of the normal shape E. coli (EcN) was statistically higher (P < 0.05) than those filamentous one (EcF) (Fig. 4a). Furthermore, the presence of 0.5 × MIC of PTZ decreased the tolerance to oxidative stress in all conditions, thus making EcF more vulnerable than EcN (Fig. 4a). Fonseca et al. also observed a similar effect in P. aeruginosa treated with sub-MIC of PTZ [5]. It is believed that bacteria subjected to antibiotics decrease the production of enzymes such as peroxidases and catalase, which protect the cell from damage caused by reactive oxygen species. Therefore, it is expected that in these conditions the bacteria will be more vulnerable to the oxidative burst during phagocytosis, which is in agreement with the results of others authors [4, 14, 17].
Graphical representation of physiological features of E. coli in the typical rod shape (EcN), the filamentous form (EcF) and in the same strains treated with 0.5 × MIC of PTZ (EcNA and EcFA). a Sensitivity to oxidative stress represented by zones of growth inhibition by H2O2. b Biofilm formation in a 96-well polypropylene microplate. c Cell surface hydrophobicity. d Motility represented by zones of growth (migration) in semi-solid agar. The graphs represent mean and standard error. Numbers 1, 2, and 3 represent significant differences (P < 0.05): 1 EcN compared to EcF and/or EcNA, 2 EcFA in relation to ECF, 3 EcNA in relation to EcFA
Effect of PTZ Sub-MIC on Biofilm Formation
The level of biofilm formation by filamentous E. coli (EcF) was lower (P < 0.05) than that of the typical rod-shaped bacteria (EcN). Furthermore, PTZ sub-MIC markedly inhibited the biofilm formation by both EcN and EcF cultures, with the filamentous bacteria being less capable of forming biofilm (Fig. 4b). Similar results were found by Fonseca et al., who observed lower biofilm formation in P. aeruginosa exposed to sub-MIC of PTZ and more pronounced inhibition when the bacteria were presented in the filamentous form [5]. The onset of biofilm formation in E. coli is dependent on motility and adhesion capabilities [35]. In addition to the influence of adhesion, PTZ sub-MIC may affect other factors required for biofilm formation, such as the quorum-sensing system [15, 38]. This system is key for the communication between cells and is essential for the proper formation and maintenance of biofilms. Salmonella enterica serovar Typhimurium treated with sub-MIC of antibiotics also exhibited reduced biofilm formation, in addition to reduced production of exopolysaccharides [16]. Moreover, Bagge et al. observed differential gene expression in biofilms formed by P. aeruginosa treated with sub-MIC of imipenem [39]. Thus, sub-MIC of PTZ may be influencing gene expression in E. coli, resulting in the inhibition of essential factors for the formation, maturation, and maintenance of the biofilm. More recently, de Souza-Filho et al. showed significant reduction in the biofilm formation by Fusobacterium nucleatum exposed to sub-MIC of ampicillin, ampicillin-sulbactam, and PTZ that, as stated by the authors, probably caused a decrease in the concentration of adhesins on the bacterial surface [6].
Effect of PTZ sub-MIC on cell hydrophobicity
EcF showed a significant (P < 0.05) decrease in cell surface hydrophobicity (Fig. 4c), which was expressed as a decrease in the percentage of cells adhering to n-hexadecane. Fonseca et al. and Fonseca and Sousa also observed a decrease in hydrophobicity in P. aeruginosa that were morphologically altered by 0.5 × MIC of PTZ and correlated the lower hydrophobicity with changes in the bacterial surface structures, in particular fimbriae, which greatly contribute to P. aeruginosa hydrophobicity [5, 8]. Various beta-lactams antibiotics such as penicillin, ampicillin, and ceftazidime in sublethal concentrations markedly impair adhesion of E. coli to epithelial human cells due to lost fimbrial expression and the adhesive properties, suggesting a link between the functional inactivation of the carboxypeptidase and the absence of fimbriae on the bacterial surface [40]. Changes in cell surface structures due to sub-MIC of antibiotics have been reported by other authors who observed decreased expression of pili in Neisseria gonorrhoeae treated with sub-MICs of azithromycin [9] and changes in surface antigens of Pasteurella multocida treated with penicillin G, tetracycline, trimethoprim, and sulfametoxazol [10]. Braga et al. and Dal Sasso et al. reported a decrease in E. coli hydrophobicity, possibly due to a smaller amount of fimbriae on the surface [4, 14]. In the case that the cell surface hydrophobicity correlates with the adhesiveness, one would assume that the EcF also has a lower adhesion, consistent with the reduced ability to form biofilm found in the present study.
Effect of PTZ Sub-MIC on E. coli Motility
The filamentous form of E. coli (EcF) also showed decreased motility in the presence of the antimicrobial in relation to the normal rod-shaped bacteria (EcN) (P < 0.05) (Fig. 4d). Furthermore, the presence of 0.5 × MIC of PTZ decreased the motility of both EcN and EcF, with the filamentous form again being more affected by the PTZ than the normal one (EcN) (Fig. 4d). Similar results were found in studies with P. aeruginosa treated with PTZ [5, 8] and in E. coli treated with sub-MIC of gemifloxacin and cefodizime, showing that drug concentration is directly proportional to the effects [4, 14]. Chen et al. also reported decreased motility of filamentous form of B. pseudomallei induced by ceftazidime, ofloxacin, and trimethoprim and reported the restoration of the motility after growing the cells without antibiotic [27]. A decreased motility due to bacterial treatment with sub-MIC of antibiotics may hinder the spread of bacteria in the in vivo situation, as proposed by Buijs et al. that reported less dispersion of E. coli in animal models of infection under treatment with sub-MICs of antibiotics [23]. This hypothesis is also consistent with Braga et al. and Dal Sasso et al. [4, 14]. It is possible that the decrease in motility observed in our experiments is related to a lower proportion of flagella given the increased size acquired by filamentous cells, thus preventing the standard motility of these cells. Another possibility is that less energy is available for the filamentous cells to effectively use the flagella for movement [27]. Lower motility may also imply a decrease in biofilm formation [41], supporting the data found.
Effect of PTZ Sub-MIC on E. coli Pathogenicity in Vivo
In the murine model of intra-abdominal infection, EcF showed lower pathogenicity than the typically shaped E. coli (EcN). EcN was detected in the spleen, liver, lung, and peritoneal fluid, while filamentous E. coli (EcF) was only detected in the peritoneal cavity, 1 h post-inoculation (Fig. 5). This finding corroborates the decreased virulence parameters observed for morphologically altered E. coli. Furthermore, it is believed that these morphologically abnormal cells are more sensitive to killing by phagocytes, which is in agreement with previously published works with E. coli and cefodizime sub-MIC [4], E. coli and Staphylococcus aureus with gemifloxacin sub-MIC [14], and P. aeruginosa treated with sub-MIC of imipenem and ceftazidime [17]. Moreover, the presence of bacteria in sites outside the peritoneal cavity such as in the lung, which is anatomically isolated from the peritoneal cavity, indicates bacterial migration, though no organism was detected in the blood. However, it is important to highlight the limitations of these analysis, which was based only on the detection of microorganisms in different anatomical sites. Thus, it is mandatory in future studies, the reassessment of these in vitro findings in model of infection and antimicrobial therapy that best approximates the actual situation in vivo.
Bacterial counts in the spleen, liver, lungs, and peritoneal lavage from mice challenged with E. coli with typical morphology (N) and E. coli with altered morphology (F). The mice were sacrificed after 1 h (N 1h, F 1h), 3 h (N 3hs, F 3hs) and 6 h (N 6hs, F 6hs) post-inoculation. CTL control group inoculated with the vehicle of the bacterial suspension. The graphs represent mean and standard error values. *statistically significant difference (P < 0.05) between N1h and F1h
In summary, the treatment of E. coli with sub-MIC of PTZ generates filamentous forms which are accompanied by the inhibition of virulence factors such as the oxidative stress response, biofilm formation, cell surface hydrophobicity, and motility (Table 1). These results are consistent with the reduced pathogenicity observed for the filamentous E. coli in the murine model of intra-abdominal infection, although more detailed analysis of host–pathogen interaction in the presence of PTZ sub-MIC is still needed. In other words, the treatment of E. coli with sub-MIC of PTZ suggests a decrease in their virulence.
References
Iida K, Hirata S, Nakamuta S, Koike M (1978) Inhibition of cell division of Escherichia coli by a new synthetic penicillin, piperacillin. Antimicrob Agents Chemother 14:257–266
Lorian V, Waluschka A, Kim Y (1982) Abnormal morphology of bacteria in the sputa of patients treated with antibiotics. J Clin Microbiol 16:382–386
Lorian VGC (1991) Effect of low antibiotic concentrations on bacteria effects on ultrastructure, virulence, and susceptibility to immune defenses. Antibiotics in Laboratory Medicine. Williams & Wilkins Co, Baltimore, pp 493–549
Braga PC, Sasso MD, Sala MT (2000) Sub-MIC concentrations of cefodizime interfere with various factors affecting bacterial virulence. J Antimicrob Chemother 45:15–25
Fonseca AP, Extremina C, Fonseca AF, Sousa JC (2004) Effect of subinhibitory concentration of piperacillin/tazobactam on Pseudomonas aeruginosa. J Med Microbiol 53:903–910
De Souza Filho JA, Diniz CG, Barbosa NB et al (2012) Morphological, biochemical, physiological and molecular aspects of the response of Fusobacterium nucleatum exposed to subinhibitory concentrations of antimicrobials. Anaerobe 18:566–575
Freitas MCR, Silva VL, Gameiro J et al (2015) Bacteroides fragilis response to subinhibitory concentrations of antimicrobials includes different morphological, physiological and virulence patterns after in vitro selection. Microb Pathog 78:103–113
Fonseca AP, Sousa JC (2007) Effect of antibiotic-induced morphological changes on surface properties, motility and adhesion of nosocomial Pseudomonas aeruginosa strains under different physiological states. J Appl Microbiol 103:1828–1837
Gorby GL, McGee ZA (1990) Antimicrobial interference with bacterial mechanisms of pathogenicity: effect of sub-MIC azithromycin on gonococcal piliation and attachment to human epithelial cells. Antimicrob Agents Chemother 34:2445–2448
Lebrun A, Caya M, Jacques M (1992) Effects of sub-MICs of antibiotics on cell surface characteristics and virulence of Pasteurella multocida. Antimicrob Agents Chemother 36:2093–2098
Justice SS, Hunstad DA, Cegelski L, Hultgren SJ (2008) Morphological plasticity as a bacterial survival strategy. Nat Rev Microbiol 6:162–168
Mohsin M, Haque A, Ali A et al (2010) Effects of ampicillin, gentamicin, and cefotaxime on the release of Shiga toxins from Shiga toxin-producing Escherichia coli isolated during a diarrhea episode in Faisalabad, Pakistan. Foodborne Pathog Dis 7:85–90
Braga PC, Piatti G (1993) Favourable effects of sub-MIC rufloxacin concentrations in decreasing the pathogen-host cell adhesion. Pharmacol Res 28:11–19
Dal Sasso M, Culici M, Bovio C, Braga PC (2003) Gemifloxacin: effects of sub-inhibitory concentrations on various factors affecting bacterial virulence. Int J Antimicrob Agents 21:325–333
Tateda K, Ishii Y, Kimura S et al (2007) Suppression of Pseudomonas aeruginosa quorum-sensing systems by macrolides: a promising strategy or an oriental mystery? J Infect Chemother 13:357–367
Majtán J, Majtánová L, Xu M, Majtán V (2008) In vitro effect of subinhibitory concentrations of antibiotics on biofilm formation by clinical strains of Salmonella enterica serovar Typhimurium isolated in Slovakia. J Appl Microbiol 104:1294–1301
Sasahara T, Satoh Y, Sekiguchi T et al (2003) Pretreatment of Pseudomonas aeruginosa with a sub-MIC of imipenem enhances bactericidal activity of neutrophils. J Infect Chemother 9:297–303
Dos Santos KV, Nicoli JR, Martins WA et al (2007) Comparative activity of ertapenem and piperacillin tazobactam in a murine systemic infection model with Bacteroides fragilis and Escherichia coli. J Med Microbiol 56:1576–1579
Holt JG, Krieg NR, Sneath PHS, Staley JTWS (1994) Bergey´s manual of determinative bacteriology, 9th edn. Williams & Wilkins, Baltimore
Dos Santos SG, Diniz CG, da Silva VL et al (2007) The influence of molecular oxygen exposure on the biology of Prevotella intermedia, with emphasis on its antibiotic susceptibility. J Appl Microbiol 103:882–891
O’Toole GA, Pratt LA, Watnick PI et al (1999) Genetic approaches to study of biofilms. Methods Enzymol 310:91–109
Wolfe AJ, Berg HC (1989) Migration of bacteria in semisolid agar. Proc Natl Acad Sci USA 86:6973–6977
Buijs J, Dofferhoff ASM, Mouton JW, van der Meer JWM (2006) Pathophysiology of in vitro induced filaments, spheroplasts and rod-shaped bacteria in neutropenic mice. Clin Microbiol Infect 12:1105–1111
Buijs J, Dofferhoff ASM, Mouton JW, van der Meer JWM (2007) Continuous administration of PBP-2- and PBP-3-specific beta-lactams causes higher cytokine responses in murine Pseudomonas aeruginosa and Escherichia coli sepsis. J Antimicrob Chemother 59:926–933
Kazmierczak A, Pechinot A, Siebor E et al (1989) Sulbactam: secondary mechanisms of action. Diagn Microbiol Infect Dis 12:139S–146S
Moosdeen F, Williams JD, Yamabe S (1988) Antibacterial characteristics of YTR 830, a sulfone β-lactamase inhibitor, compared with those of clavulanic acid and sulbactam. Antimicrob Agents Chemother 32:925–927
Chen K, Sun GW, Chua KL, Gan Y-H (2005) Modified virulence of antibiotic-induced Burkholderia pseudomallei filaments. Antimicrob Agents Chemother 49:1002–1009
Justice SS, Hung C, Theriot JA et al (2004) Differentiation and developmental pathways of uropathogenic Escherichia coli in urinary tract pathogenesis. Proc Natl Acad Sci USA 101:1333–1338
Gottfredsson M, Erlendsdóttir H, Sigfússon A, Gudmundsson S (1998) Characteristics and dynamics of bacterial populations during postantibiotic effect determined by flow cytometry. Antimicrob Agents Chemother 42:1005–1011
Wickens HJ, Pinney RJ, Mason DJ, Gant VA (2000) Flow cytometric investigation of filamentation, membrane patency, and membrane potential in Escherichia coli following ciprofloxacin exposure. Antimicrob Agents Chemother 44:682–687
Rothfield L, Justice S, García-Lara J (1999) Bacterial cell division. Annu Rev Genet 33:423–448
Diarra MS, Malouin F, Jacques M (1999) Postantibiotic and physiological effects of tilmicosin, tylosin, and apramycin at subminimal and suprainhibitory concentrations on some swine and bovine respiratory tract pathogens. Int J Antimicrob Agents 12:229–237
Diarra MS, Petitclerc D, Lacasse P (2002) Effect of lactoferrin in combination with penicillin on the morphology and the physiology of Staphylococcus aureus isolated from bovine mastitis. J Dairy Sci 85:1141–1149
Fang H, Edlund C, Hultenby K, Hedberg M (2002) Effects of cefoxitin on the growth and morphology of Bacteroides thetaiotaomicron strains with different cefoxitin susceptibility. Anaerobe 8:55–61
Silvestro EM, Nakano V, Arana-Chavez VE et al (2006) Effects of subinhibitory concentrations of clindamycin on the morphological, biochemical and genetic characteristics of Bacteroides fragilis. FEMS Microbiol Lett 257:189–194
Veloso Lde C, dos Santos KV, de Andrade HM et al (2013) Proteomic changes in Bacteroides fragilis exposed to subinhibitory concentration of piperacillin/tazobactam. Anaerobe 22:69–76
Valéria dos Santos K, Diniz CG, de Castro Veloso L et al (2010) Proteomic analysis of Escherichia coli with experimentally induced resistance to piperacillin/tazobactam. Res Microbiol 161:268–275
Kai T, Tateda K, Kimura S et al (2009) A low concentration of azithromycin inhibits the mRNA expression of N-acyl homoserine lactone synthesis enzymes, upstream of lasI or rhlI, in Pseudomonas aeruginosa. Pulm Pharmacol Ther 22:483–486
Bagge N, Schuster M, Hentzer M et al (2004) Pseudomonas aeruginosa biofilms exposed to imipenem exhibit changes in global gene expression and beta-lactamase and alginate production. Antimicrob Agents Chemother 48:1175–1187
Schifferli DM, Beachey EH (1988) Bacterial adhesion: modulation by antibiotics with primary targets other than protein synthesis. Antimicrob Agents Chemother 32:1609–1613
Pratt LA, Kolter R (1998) Genetic analysis of Escherichia coli biofilm formation: roles of flagella, motility, chemotaxis and type I pili. Mol Microbiol 30:285–293
Acknowledgments
Sérgio, Luiza, Vivian, MOA, Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Pró-Reitorias de Pesquisa e Pós-Graduação (PRPPG) da Universidade Federal de Minas Gerais (UFMG) e da Universidade Federal do Espírito Santo (UFES).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Andrade, J.P.L., de Macêdo Farias, L., Ferreira, J.F.G. et al. Sub-Inhibitory Concentration of Piperacillin–Tazobactam May be Related to Virulence Properties of Filamentous Escherichia coli . Curr Microbiol 72, 19–28 (2016). https://doi.org/10.1007/s00284-015-0912-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-015-0912-9