Abstract
The study provides phenotypic and molecular analyses of the antibiotic resistance in lactic acid bacteria (LAB) from fermented foods in Xi’an, China. LAB strains (n = 84) belonging to 16 species of Lactobacillus (n = 73), and Streptococcus thermophilus (n = 11) were isolated and identified by sequencing their 16S rRNA gene. All strains were susceptible to ampicillin, bacitracin, and cefsulodin, and intrinsically resistant to nalidixic acid, kanamycin, and vancomycin (except L. bulgaricus, L. acidophilus, and S. thermophilus, which were susceptible to vancomycin). Some strains had acquired resistance for penicillin (n = 2), erythromycin (n = 9), clindamycin (n = 5), and tetracycline (n = 14), while resistance to gentamycin, ciprofloxacin, streptomycin, and chloramphenicol was species dependant. Minimum inhibitory concentrations presented in this study will help to review microbiological breakpoints for some of the species of Lactobacillus. The erm(B) gene was detected from two strains of each of L. fermentum and L. vaginalis, and one strain of each of L. plantarum, L. salivarius, L. acidophilus, L. animalis, and S. thermophilus. The tet genes were identified from 12 strains of lactobacilli from traditional foods. This is the first time, the authors identified tet(S) gene from L. brevis and L. kefiri. The erm(B) gene from L. fermentum NWL24 and L. salivarius NWL33, and tet(M) gene from L. plantarum NWL22 and L. brevis NWL59 were successfully transferred to Enterococcus faecalis 181 by filter mating. It was concluded that acquired antibiotic resistance is well dispersed in fermented food products in Xi’an, China and its transferability to other genera should be monitored closely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lactic acid bacteria (LAB) have a long history of safe use as fermenting natural products and probiotics intended for health benefits and have acquired the “Generally recognized as safe” (GRAS) status [32]. Since the introduction of antibiotics more than 50 years ago, emergence of resistant microorganisms has become a major threat to public health [34]. Antibiotic resistance is well studied and documented for human pathogenic species [32]. However, since the last decade, researchers have also focused on characterizing antibiotic resistance in LAB [4]. LAB can serve as reservoir for antibiotic resistance genes and transfer it to other microorganisms including pathogens [23, 43]. This situation has become more hazardous by the overuse and misuse of antibiotics in feed, agriculture, and veterinary applications [2, 42]. European Food Safety Authority (EFSA) recommends that bacterial strains harboring transferable antibiotic resistance genes should not be used in animal feeds, fermented and probiotic foods for human [14].
Lactobacilli are dominant bacteria in several fermented foods such as meat and dairy products, which interact with gut microflora on ingestion [2]. Lactobacilli are generally intrinsically resistant for quinolones, trimethoprim, and sulphonamides, and susceptible to all protein synthesis inhibitors except aminoglycosides. Resistance of many species of lactobacilli except L. delbrueckii subsp. bulgaricus, L. acidophilus, L. johnsonii, and L. crispatus to glycopeptides is also considered intrinsic [8, 32]. Intrinsic resistance is not horizontally transferable as it is chromosomally encoded and related to the general physiology or anatomy of an organism. Acquired resistance is horizontally transferable, which emerges from genetic changes by mutations or acquisition of genetic elements (plasmids or transposons) most probably by conjugation [2, 4, 32]. Acquired antibiotic resistance in lactobacilli has been reported frequently in recent years from fermented milk products [10, 11, 29, 35, 41], pickles, and meat but there are no reports from China in this regard.
The objective of this study was a safety assessment of bacterial isolates from starter cultures and naturally fermented foods by phenotypic screening, polymerase chain reaction (PCR) and filter mating. This study provides data on the current resistance situation and insinuate for further monitoring and development of regulations for antibiotic resistance in food associated LAB in China.
Materials and Methods
Isolation of LAB and Growth Conditions
Bacterial strains were isolated from commercial and traditionally fermented food samples including Yogurt (n = 13), Whey or fermented milk (n = 10), Jiang shui (n = 3), and fermented vegetables (n = 15). Jiang shui is a traditional Chinese drink, made by fermenting a mixture of vegetables. Food samples obtained from local markets were homogenized and serial dilutions were plated on selective media and incubated at 37°C for 48 h. Lactobacilli were selected on MRS agar (Oxoid) plates incubated in anaerobic conditions (Anaerogen, Oxoid), while streptococci were isolated on M17 (Oxoid) agar plates in aerobic environment. After the incubation, distinguished colonies were selected, purified, and stored in MRS broth with 15% (w/v) glycerol at −20°C. Enterococcus faecalis ATCC 29212 and E. faecium ATCC 35667 were used as control strains in antibiotic sensitivity testing. Prior to all experiment bacterial isolates were subcultured at least twice.
Identification of LAB
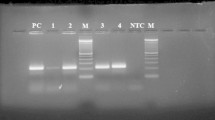
Preliminary identification of isolates was performed by gram staining and catalase test. DNA was extracted from bacterial isolates using a commercial kit (TianGen, Beijing, China) according to the manufacturer’s instructions. Lactobacillus genus was identified by PCR using genus specific primers XB5 and LbLMA1-R. For the identification of species, amplification of partial 16S rRNA gene was performed by universal primers (Table 1) in an automated thermocycler (ABI 2720 USA) using the following program: initial denaturation at 95°C for 5 min; followed by 35 cycles of 95°C for 45 s, 55°C for 45 s, 72°C for 1 min, and a final extension at 72°C for 7 min. Amplified products were resolved by 1.5% (w/v) agarose gel electrophoresis and visualized by ethidium bromide staining (0.5 μg/ml) under UV transillumination. PCR products (nearly 1,380 bp) were purified and sequenced directly by Beijing genomics institute (BGI) by using the same universal primers. LAB isolates were identified to the species level by comparing their sequences with those in the NCBI databases by BLAST. All sequences were submitted to GenBank and accession numbers were obtained.
Antibiotic Resistance
Minimum inhibitory concentrations (MICs) of 14 antibiotics were determined by broth microdilution method using LAB susceptibility test medium (LSM) [30], a mixed formulation containing Iso-Sensitest broth (90%) and MRS broth (10%). Penicillin G, ampicillin, erythromycin, clindamycin, tetracycline, cefsulodin, bacitracin, and ciprofloxacin were tested in concentration range of (0.032–64 mg/l) while, gentamicin, kanamycin, fusidic acid, streptomycin, chloramphenicol, nalidixic acid, and vancomycin in concentration range of (0.125–256 mg/l). In brief, 50 μl of antibiotics, doubly diluted in LSM broth were inoculated with 100 μl of test strain inoculum. Inoculum of the test strain was prepared by suspending colonies from LSM agar plates in 5 ml 0.85% NaCl solution to a turbidity of McFarland 1 standard and subsequently diluting them 1:1000 in LSM broth. Plates were incubated under anaerobic conditions at 37°C for 48 h. MICs were read as the lowest concentration of an antimicrobial agent at which visible growth was inhibited. Breakpoints were adopted from EFSA [15]. Breakpoints for antibiotic not covered by EFSA were adopted from Danielsen and Wind [10].
Amplification of Antibiotic Resistance Genes
Antibiotic resistance genes for β-lactam (bla), erythromycin [erm(A), erm(B), and mef(A)], tetracycline [tet(M), tet(O), tet(Q), tet(S), tet(W), tet(K), and tet(L)], gentamycin [aac(6′)-aph(2′′)], and chloramphenicol (cat) were amplified by PCR using primers given in Table 1. The reaction mixtures (50 μl) contained 25 pmol of each primer, 1.5, 2.0, 2.5, or 3.0 mM MgCl2 depending on experiment, 50–100 ng bacterial DNA, and 2.5 U of Taq DNA Polymerase. DNA fragments were amplified in a thermal cycler up to 40 cycles by using annealing temperatures given in Table 1. Positive and negative controls form our lab were used for all PCR reactions. PCR products were subjected to agarose gel electrophoresis in TAE buffer. Gels were stained with ethidium bromide (5 μg/ml) and visualized under UV transillumination.
Transfer of Antibiotic Resistance
Transfer of antibiotic resistance was analyzed by filter mating experiments as described by Gevers et al [24] with slight modifications. Enterococcus faecalis 181 and E. facium 258 were used as the recipient, which were sensitive to erythromycin and tetracycline, and resistant to rifampicin and fusidic acid. The tet(M), and erm(B) positive strains from the study were used as donors. Equal volumes (1 ml each) of donor and recipient strain, at exponential growth were mixed, filtered through a sterile 0.45 μm-pore-size nitrocellulose membrane filter (Millipore, USA), and placed on MRS agar plates. After incubation at 37°C for 24 h, cells were resuspended in phosphate buffer saline and serial dilutions were spread on selective medium. Following incubation for 48 h, transconjugants were selected and analyzed by antimicrobial susceptibility. The transfer of resistant gene tet(M) and erm(B) was confirmed in transconjugants by the detection of tet(M) and erm(B) by PCR. The number of transconjugants per recipient cell was given as conjugation frequencies.
The GenBank accession numbers of sequences reported in this article are mainly from HQ293024–HQ293117and HQ111074–HQ111078.
Results
Isolation and Identification of LAB
A total of 22 LAB, including, L. delbrueckii subsp. bulgaricus (n = 6), L. acidophilus (n = 6), L. rhamnosus (n = 1), L. kefiri (n = 1), and S. thermophilus (n = 8) were isolated from commercial Yogurts. 62 LAB strains belonging to species L. delbrueckii subsp. bulgaricus (n = 7), L. acidophilus (1), L. casei (n = 5), L. rhamnosus (3), L. fermentum (5), L. plantarum (7), L. brevis (6), L. salivarius (5), L. parabuchneri (12), L. alimentarius (2), L. anamalis (2), L. vaginalis (2), L. parabrevis (1), L. coryniformis (1), and S. thermophilus (n = 3) were isolated from traditional products of whey, yogurt, pickle, and Jiang shui. Species were identified by partially sequencing their 16S rRNA gene and all the sequences were submitted to GenBank. All the commercial products had the probiotic or starter strains of LAB as per label, except one yogurt sample that had L. kefiri instead of L. acidophilus as indicated on product label.
Phenotypic Profile of Antimicrobial Resistances
Table 2 indicates the number of strains that were subjected to antibiotic susceptibility, 90% MIC, range, and number of resistant strains for each species. All strains were susceptible to ampicillin, bacitracin, and cefsulodin and resistant to nalidixic acid and kanamycin. All the species except, L. bulgaricus and L. acidophilus and S. thermophilus were intrinsically resistant to vancomycin. Two strains, one each of L. salivarius and S. thermophilus species were resistant to penicillin G. High percentage of strains were resistant to gentamycin (65%) and ciprofloxacin (85%) while, a low percentage was resistant to streptomycin (7%) and chloramphenicol (12%) in species dependant manner. Moderately higher percentage of strains had acquired resistance for erythromycin (11%), clindamycin (6%), and tetracycline (17%). All erythromycin (n = 9) and tetracycline (n = 14) resistant strains originated from traditional products, except tetracycline resistant L. kefiri NWL78 and S. thermophilus NWL93, which were from two different commercially produced probiotic yogurts.
Antibiotic Resistance Genes
Antibiotic resistance genes were detected by PCR from resistant strains and results are presented in Table 3. Erythromycin resistance gene erm(B) was found from eight lactobacilli strains including L. fermentum NWL24 and NWL26, L. vaginalis NWL 35 and NWL43, L. plantarum NWL22, L. acidophilus NWL23, L. salivarius NWL33, and L. animalis NWL39. One strain of S. thermophilus (NWL02), isolated from a traditionally fermented yogurt also had erm(B) gene. All the strains with atypical MIC to erythromycin were positive for erm(B), while none of the susceptible strains were positive for erm(B). Other erythromycin resistant determinants [erm(A) and mef(A)] were not detected from any strain.
Out of 14 lactobacilli strains resistant to tetracycline, eight strains were positive for tet(M) gene only, two strains had tet(M) and tet(S) together, and two strains harbored only tet(S) gene. Two strains, resistant to tetracycline were negative for any of the tested tet resistance gene. None of the tet(W), tet(O), tet(Q), tet(K), and tet(L) genes were present in any strain. All tet gene positive strains were isolated from traditional sources except L. kefiri NWL78, which was isolated from a probiotic yogurt. One strain of each of L. plantarum (NWL16) and L. salivarius (NWL33) had erm(B) and tet(M) together. Penicillin, gentamycin, chloramphenicol, and streptomycin resistant strains were negative for any of the tested genes. Vancomycin resistance was intrinsic, and strains did not harbor acquired resistance gene van(B) (data not shown).
Transfer of Antibiotic Resistance Genes
LAB strains positive for erm(B) and tet(M) were used as donors, while E. faecalis 181 and E. facium258 were used as recipient strains in filter mating experiments. Results showed that erm(B) from L. fermentum NWL24 and L. salivarius NWL33 and tet(M) gene from L. plantarum NWL22 and L. brevis NWL59 were successfully transferred to E. faecalis. All transconjugants were resistant to erythromycin (MIC > 64) or tetracycline (MIC > 128) and positive for tet(M) or erm(B) genes. Transfer rate in filter mating experiments ranged from 2.9 × 10−6 to 1.39 × 10−5 for different combinations (Table 4).
Discussion
Since 1960s, the emergence of drug resistant pathogens and lack of newly developed antibiotics is a major concern for health professionals and researchers. Magnitude of problem increases significantly by the possibility of horizontal gene transfer, misuse, and overuse of antibiotics in human medicine, veterinary, agriculture, and food products. Food chain is considered as a major route of transmission of antibiotic resistant genes between animal and human populations [32]. LAB, a dominant part of microflora of fermented foods, can exchange genes to enhance their survival in antibiotic-containing environments and may transfer it to other commensal bacteria or pathogens in the intestine, on mucosal surfaces or in food [39, 43]. LAB with acquired resistance should be discouraged from entering into human food chain and a careful monitoring and regulation must be implied to check their antibiotic resistance profiles.
A wide spread susceptibility toward the inhibitors of cell wall synthesis, such as penicillin and ampicillin have been observed in many species of lactobacilli from different sources, such as cheese [4], probiotics or fermented foods [6], and human intestine [7, 11]. All of the lactobacilli from commercial or traditionally fermented foods in this study were sensitive to penicillin and ampicillin, except one strain of L. salivarius NWL31 (MIC > 64) from pickles that was resistant to penicillin. Resistance to penicillin has been reported in some species of lactobacilli from European probiotic products [41], from sausages [23] and cheese [19].
Susceptibility of all LAB strains to ampicillin, cefsulodin, and bacitracin, and intrinsic resistance to nalidixic acid, vancomycin, and kanamycin was in accordance with previous studies [10, 31, 32, 45]. Resistance of Lactobacillus species to vancomycin is considered as intrinsic [2], except for L. delbrueckii subsp. bulgaricus, L. acidophilus, L. johnsonii, and L. crispatus [4, 7].
Acquired resistance to erythromycin is generally because of erm(B) which has been reported previously in lactobacilli from different sources [2, 4, 5, 11, 18, 21, 25, 26, 31, 32]. Other resistant determinants [erm(A), erm(C), and erm(T)] are rarely detected from LAB, including lactobacilli and S. themophillus. Tetracycline resistance is also an acquired resistance in lactobacilli and S. thermophilus. Many tetracycline resistant determinants [tet(M), tet(O), tet(S), and tet(W) or the efflux proteins tet(K) and tet(L)] have been reported [26, 32]. The authors identified tet(M) in L. plantarum, L. salivarius, L. animalis, and L. brevis from different sources. The tet(M) has also been reported previously, in L. plantarum [17, 23] and L. salivarius from meat products [3]. The authors also identified, tet(S) gene in L. kefiri (NWL78) and L. brevis (NWL51 and 59). To the authors’ knowledge, the presence of tet(S) gene in L. kefiri or L. brevis has not been described previously; however, it has been detected in members of L. plantarum [27]. Other tetracycline resistant genes [tet(O), tet(Q), and tet(W)] have also been identified in lactobacilli such as tet(W) from a probiotic L. reuteri [29], but we did not find any of these genes in this study.
Although MIC can be considered as a “true” measure, however, it can have low reproducibility between labs. Recently, LAB susceptibility medium (LSM) [30] and microbiological breakpoints have been suggested by different researchers [10, 15, 16, 20, 31, 33]. Here, the authors propose tetracycline breakpoint for L.parabuchneri, isolated from fermented vegetables as 16 μg/ml. MIC of tetracycline for all the L. parabuchneri isolates (n = 12) from different sources, was from 16 to 32. Lactobacillus parabuchneri can be isolated frequently from fermented vegetables and pickles [9], from where resistances for different antibiotics have been described in other species of lactobacilli [36, 46]. MICs of bacitracin ranged from 0.063 to 16 in this study but none of the strain was resistant by the breakpoints given by Danielsen and Wind [10].
There are only few reports on conjugative transfer of naturally occurring antibiotic resistance determinants including erm(B) and tet(M) from lactobacilli to other bacteria in vitro [24, 35] or in gnotobiotic rats [28]. Feld et al. [18] successfully transferred an erythromycin resistant plasmid (pLFE1) in vitro and in vivo, from L. plantarum to a broad host-range including L. rhamnosus, L. lactis, E. faecalis, and L. monocytogenes. Hummel et al. [26] found erm(B) gene involved in erythromycin resistance from L. salivarius strain (BFE 7441), which was on genomic DNA. Recently, a transposons Tn916 containing tet(M) gene was transferred from L. paracasei to E. faecalis strain JH2-2 in mating experiments at low conjugation frequency [12]. Erythromycin resistance determinant Erm(B) from L. fermentum NWL24 and L. salivarius NWL33, and tet(M) gene from L. plantarum NWL22 and L. brevis NWL59 were successfully transferred to E. faecalis 181. Plasmid free recipient strains were characterized in the lab in another study. The authors also implied broth mating and filter separating techniques but conjugal transfer of erm(B) and tet(M) was not successful by these methods (data not shown), which further strengthen the notion that a close contact on a solid surface is required for better conjugal transfer in LAB [24].
The authors conclude that the prevalence of antibiotic resistant LAB in Chinese food chain is high and care should be taken whenever introducing any of these strains in functional foods intentionally. Although probiotic products and starter strains rarely had acquired antibiotic resistance, the presence of tet(S) gene in L. kefiri NWL78, isolated from a probiotic yogurt, draws the attention for a strict monitoring and regulation.
References
Aarestrup FM, Agerso Y, Gerner-Smidt P et al (2000) Comparison of antimicrobial resistance phenotypes and resistance genes in Enterococcus faecalis and Enterococcus faecium from humans in the community, broilers, and pigs in Denmark. Diagn Microbiol Infect Dis 37:127–137
Ammor MS, Florez AB, Mayo B (2007) Antibiotic resistance in non-enterococcal lactic acid bacteria and bifidobacteria. Food Microbiol 24:559–570
Aquilanti L, Garofalo C, Osimani A et al (2007) Isolation and molecular characterization of antibiotic-resistant lactic acid bacteria from poultry and swine meat products. J Food Prot 70:557–565
Belletti N, Gatti M, Bottari B et al (2009) Antibiotic resistance of lactobacilli isolated from two italian hard cheeses. J Food Prot 72:2162–2169
Cataloluk O, Gogebakan B (2004) Presence of drug resistance in intestinal lactobacilli of dairy and human origin in Turkey. FEMS Microbiol Lett 236:7–12
Charteris WP, Kelly PM, Morelli L et al (1998) Antibiotic susceptibility of potentially probiotic Bifidobacterium isolates from the human gastrointestinal tract. Lett Appl Microbiol 26:333–337
Charteris WP, Kelly PM, Morelli L et al (1998) Antibiotic susceptibility of potentially probiotic Lactobacillus species. J Food Prot 61:1636–1643
Charteris WP, Kelly PM, Morelli L et al (1998) Development and application of an in vitro methodology to determine the transit tolerance of potentially probiotic Lactobacillus and Bifidobacterium species in the upper human gastrointestinal tract. J Appl Microbiol 84:759–768
Coton M, Berthier F, Coton E (2008) Rapid identification of the three major species of dairy obligate heterofermenters Lactobacillus brevis, Lactobacillus fermentum and Lactobacillus parabuchneri by species-specific duplex PCR. FEMS Microbiol Lett 284:150–157
Danielsen M, Wind A (2003) Susceptibility of Lactobacillus spp. to antimicrobial agents. Int J Food Microbiol 82:1–11
Delgado S, Florez AB, Mayo B (2005) Antibiotic susceptibility of Lactobacillus and Bifidobacterium species from the human gastrointestinal tract. Curr Microbiol 50:202–207
Devirgiliis C, Coppola D, Barile S et al (2009) Characterization of the Tn916 conjugative transposon in a food-borne strain of Lactobacillus paracasei. Appl Environ Microbiol 75:3866–3871
Dubernet S, Desmasures N, Gueguen M (2002) A PCR-based method for identification of lactobacilli at the genus level. FEMS Microbiol Lett 214:271–275
EFSA (2007) Opinion of the scientific committee on a request from EFSA on the introduction of a qualified presumption of safety (QPS) approach for assessment of selected microorganisms referred to EFSA. The EFSA Journal 187:1–16
EFSA (2008) Technical guidance prepared by the panel on additives and products or substances used in animal feed (FEEDAP) on the update of the criteria used in the assessment of bacterial resistance to antibiotics of human or veterinary importance. The EFSA Journal 732:1–15
Egervarn M, Danielsen M, Roos S et al (2007) Antibiotic susceptibility profiles of Lactobacillus reuteri and Lactobacillus fermentum. J Food Prot 70:412–418
Egervarn M, Roos S, Lindmark H (2009) Identification and characterization of antibiotic resistance genes in Lactobacillus reuteri and Lactobacillus plantarum. J Appl Microbiol 107:1658–1668
Feld L, Bielak E, Hammer K et al (2009) Characterization of a small erythromycin resistance plasmid pLFE1 from the food-isolate Lactobacillus plantarum M345. Plasmid 61:159–170
Florez AB, Delgado S, Mayo B (2005) Antimicrobial susceptibility of lactic acid bacteria isolated from a cheese environment. Can J Microbiol 51:51–58
Florez AB, Egervarn M, Danielsen M et al (2006) Susceptibility of Lactobacillus plantarum strains to six antibiotics and definition of new susceptibility-resistance cutoff values. Microb Drug Resist 12:252–256
Fons M, Hege T, Ladire M et al (1997) Isolation and characterization of a plasmid from Lactobacillus fermentum conferring erythromycin resistance. Plasmid 37:199–203
Ge B, Jiang P, Han F et al (2007) Identification and antimicrobial susceptibility of lactic acid bacteria from retail fermented foods. J Food Prot 70:2606–2612
Gevers D, Danielsen M, Huys G et al (2003) Molecular characterization of tet(M) genes in Lactobacillus isolates from different types of fermented dry sausage. Appl Environ Microbiol 69:1270–1275
Gevers D, Huys G, Swings J (2003) In vitro conjugal transfer of tetracycline resistance from Lactobacillus isolates to other Gram-positive bacteria. FEMS Microbiol Lett 225:125–130
Gfeller KY, Roth M, Meile L et al (2003) Sequence and genetic organization of the 19.3-kb erythromycin- and dalfopristin-resistance plasmid pLME300 from Lactobacillus fermentum ROT1. Plasmid 50:190–201
Hummel AS, Hertel C, Holzapfel WH et al (2007) Antibiotic resistances of starter and probiotic strains of lactic acid bacteria. Appl Environ Microbiol 73:730–739
Huys G, D’Haene K, Swings J (2006) Genetic basis of tetracycline and minocycline resistance in potentially probiotic Lactobacillus plantarum strain CCUG 43738. Antimicrob Agents Chemother 50:1550–1551
Jacobsen L, Wilcks A, Hammer K et al (2007) Horizontal transfer of tet(M) and erm(B) resistance plasmids from food strains of Lactobacillus plantarum to Enterococcus faecalis JH2–2 in the gastrointestinal tract of gnotobiotic rats. FEMS Microbiol Ecol 59:158–166
Kastner S, Perreten V, Bleuler H et al (2006) Antibiotic susceptibility patterns and resistance genes of starter cultures and probiotic bacteria used in food. Syst Appl Microbiol 29:145–155
Klare I, Konstabel C, Muller-Bertling S et al (2005) Evaluation of new broth media for microdilution antibiotic susceptibility testing of Lactobacilli, Pediococci, Lactococci, and Bifidobacteria. Appl Environ Microbiol 71:8982–8986
Klare I, Konstabel C, Werner G et al (2007) Antimicrobial susceptibilities of Lactobacillus, Pediococcus and Lactococcus human isolates and cultures intended for probiotic or nutritional use. J Antimicrob Chemother 59:900–912
Mathur S, Singh R (2005) Antibiotic resistance in food lactic acid bacteria—a review. Int J Food Microbiol 105:281–295
Mayrhofer S, van Hoek AH, Mair C et al (2010) Antibiotic susceptibility of members of the Lactobacillus acidophilus group using broth microdilution and molecular identification of their resistance determinants. Int J Food Microbiol 144(1):81–87
Mazel D, Davies J (1999) Antibiotic resistance in microbes. Cell Mol Life Sci 56:742–754
Ouoba LI, Lei V, Jensen LB (2008) Resistance of potential probiotic lactic acid bacteria and bifidobacteria of African and European origin to antimicrobials: determination and transferability of the resistance genes to other bacteria. Int J Food Microbiol 121:217–224
Perez Pulido R, Omar NB, Lucas R et al (2005) Resistance to antimicrobial agents in lactobacilli isolated from caper fermentations. Antonie Van Leeuwenhoek 88:277–281
Relman DA, Loutit JS, Schmidt TM et al (1990) The agent of bacillary angiomatosis. An approach to the identification of uncultured pathogens. N Engl J Med 323:1573–1580
Rojo-Bezares B, Saenz Y, Poeta P et al (2006) Assessment of antibiotic susceptibility within lactic acid bacteria strains isolated from wine. Int J Food Microbiol 111:234–240
Salyers AA, Gupta A, Wang Y (2004) Human intestinal bacteria as reservoirs for antibiotic resistance genes. Trends Microbiol 12:412–416
Sutcliffe J, Grebe T, Tait-Kamradt A et al (1996) Detection of erythromycin-resistant determinants by PCR. Antimicrob Agents Chemother 40:2562–2566
Temmerman R, Pot B, Huys G et al (2003) Identification and antibiotic susceptibility of bacterial isolates from probiotic products. Int J Food Microbiol 81:1–10
Teuber M (2001) Veterinary use and antibiotic resistance. Curr Opin Microbiol 4:493–499
Teuber M, Meile L, Schwarz F (1999) Acquired antibiotic resistance in lactic acid bacteria from food. Antonie Van Leeuwenhoek 76:115–137
Xu J, Smyth CL, Buchanan JA et al (2004) Employment of 16 S rDNA gene sequencing techniques to identify culturable environmental eubacteria in a tertiary referral hospital. J Hosp Infect 57:52–58
Zhou JS, Pillidge CJ, Gopal PK et al (2005) Antibiotic susceptibility profiles of new probiotic Lactobacillus and Bifidobacterium strains. Int J Food Microbiol 98:211–217
Zonenschain D, Rebecchi A, Morelli L (2009) Erythromycin- and tetracycline-resistant lactobacilli in Italian fermented dry sausages. J Appl Microbiol 107:1559–1568
Acknowledgments
This study was supported by higher education commission (HEC) of Pakistan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nawaz, M., Wang, J., Zhou, A. et al. Characterization and Transfer of Antibiotic Resistance in Lactic Acid Bacteria from Fermented Food Products. Curr Microbiol 62, 1081–1089 (2011). https://doi.org/10.1007/s00284-010-9856-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-010-9856-2