Abstract
Salmonellaenterica serotype Newport is an important cause of non-typhoidal salmonellosis, a clinically less severe infection than typhoid fever caused by S. enterica serotype Typhi. In this investigation, the virulence genotypes of S. enterica Newport isolated from a backwater environment were compared with Salmonella Typhi from clinical cases in the same region where salmonellosis is endemic. Genotyping was done by PCR screening for virulence markers associated with Salmonella pathogenicity islands (SPIs) and plasmids. The virulence genes associated with SPIs I–VI were detected in 95–100% of all the isolates, while the viaB locus representing SPI-7 was detectable in 66 and 73% of the environmental and clinical isolates, respectively. A significant number of Salmonella Newport lacked virulence genes shdA and sopE compared to S. Typhi. All S. Typhi and S. Newport isolates lacked large plasmid-borne virulence genes spvR and pefA. Further investigations into the antimicrobial resistance of S. Newport revealed multiple drug resistance to ampicillin, amoxicillin/clavulanic acid, trimethorprim-sulfamethoxazole, chloramphenicol, tetracycline, cephalothin, and cephalexin. In comparison, S. Typhi were susceptible to all clinically relevant antimicrobials. The results of this study will help in understanding the spread of virulence genotypes and antibiotic resistance in S. Newport in the region of study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salmonellaenterica subspecies I comprises of more than 2,000 serotypes capable of causing a range of intestinal and extraintestinal infections in humans from life-threatening septicemic typhoid fever to mild self-limiting gastroenteritis [6, 26]. The diverse serotypes of Salmonella vary in their host adaptation and virulence [2]. Salmonella serotype Typhi is a highly host-adapted serotype responsible for lethal invasive typhoid fever in humans characterized by high morbidity and mortality. In contrast, non-typhoidal serotypes exemplified by Salmonella Typhimurium have a broad host range including birds, reptiles and mammals and cause mild gastroenteritis in humans. When antibiotic treatment is desired in severe cases of infections, the drugs of choice are usually ampicillin, third-generation cephalosporins (ceftriaxone) or fluoroquinolones (ciprofloxacin). Lately, emergence of S. enterica with decreased susceptibilities to both classes of the fluoroquinolones and the cephalosporins has complicated treatment of salmonellosis [15, 16].
Salmonella possesses a myriad of genetic factors contributing for its success as an intracellular human pathogen that participate at various stages of invasion, intracellular replication and survival within the host. The virulence genes are distributed on large genomic regions of 10–200 kb known as Salmonella pathogenicity islands (SPIs) [17, 22]. Some virulence genes not located on SPIs such as the chromosomally encoded stn (Salmonella enterotoxin gene), phoP/Q (two component global regulator) and iroB also play important roles in the virulence of Salmonella [3, 28]. Many Salmonella serotypes harbor large plasmids of varying sizes that carry genes responsible for virulence in mouse models [13, 14].
This study was designed to compare Salmonella isolates from a backwater environment with clinical isolates of S. Typhi with focus on virulence genotypes and antimicrobial resistance. Salmonellosis is endemic in the region, though the relative contribution of typhoidal and non-typhoidal S. enterica to the disease burden is unknown. The evolution of virulence and antimicrobial resistance capabilities of pathogenic bacteria takes place by horizontal acquisition of genes and the aquatic environment is arguably an ideal ecosystem for such interactions among various groups of bacteria. The isolates were screened for genes associated with seven known SPIs and plasmids that are known to contribute significantly to establishment of infections and consequently the success of Salmonella as an intracellular pathogen. Such a study will help to understand the infection potentials and the evolution of virulence and antimicrobial resistance in S. enterica introduced into the environment, and lead towards developing suitable preventive strategies to counter the spread of this enteric pathogen in the community surrounding this backwater ecosystem.
Materials and Methods
Isolation and Identification of Salmonella
Ninety isolates of Salmonella were used in this study, of which 60 were Salmonella serotype Newport isolated from Cochin backwaters. Thirty clinical isolates of Salmonella serotype Typhi were provided by a local general hospital and private clinical laboratories. Environmental Salmonella Newport were isolated from water, shrimp and crabs following the method described in Bacteriological Analytical Manual, U.S. Food and Drug Administration [11]. Colonies typical of Salmonella were sub-cultured onto tryptic soya agar (TSA) slants and subjected to a series of biochemical tests for identification of Salmonella spp. The isolates were archived at −80°C in LB broth containing 15% glycerol. Serotyping of the isolates was done at the National Salmonella and Escherichia Centre, Central Research Institute, Kasauli, India.
Virulence Genotyping of Isolates by PCR
The primers designed in this study for PCR detection of various virulence genes present on SPIs are listed in the Table 1. Pure genomic DNA from the isolates was extracted following the protocol of Ausubel et al. [1]. PCR amplifications of invA, pefA, shdA, hilA, iroB, agfA, sopE, stn, ttrC, spi4D, pipA, spvC and spvR were performed as described previously [27, 29, 35, 36]. In addition, primers were designed in this study for the amplification of mgtB, ttrC, viaB, pagN, pipA, spi4R, spi4D, spiC, fliC, pefC, spvC, spvR, shdA and sopB genes. The PCR cycling conditions consisted 30 cycles of 1 min denaturation at 94°C, 1 min annealing at 55°C and 1 min extension at 72°C. S. Typhimurium (ATCC14028) was used in invA, hilA, spvR, iroB, agfA, shdA and stn PCR assays, while S. Typhi (Presque Isle Cultures, Erie, PA) was used in pefA and sopE PCR as reference strains.
Antimicrobial Susceptibility Testing
The antimicrobial susceptibility of Salmonella isolates of this study was determined by standard agar disc diffusion technique in accordance with the Clinical and Laboratory Standards Institute (CLSI) guidelines [10] on Mueller Hinton agar using commercial discs (HiMedia, Mumbai, India). The antibiotics used were ampicillin (10 μg), amoxicillin (30 μg), bacitracin, cephalexin (30 μg), cephalothin (30 μg), chloramphenicol (30 μg), ciprofloxacin (5 μg), erythromycin (15 μg), gentamicin (10 μg), kanamycin (30 μg), nalidixic acid (30 μg), nitrofurantoin (100 μg), norfloxacin (10 μg), penicillin G (10 U), streptomycin (10 μg), sulfamethoxazole (300 μg), tetracycline (30 μg), tobramycin (30 μg) and trimethoprim (10 μg).
Plasmid Extraction
For extraction of large plasmids associated with Salmonella, a previously described protocol was used [37]. S. Typhimurium 14028 was used as the positive control. The plasmids preparations were separated on a 0.7% agarose gel and visualized by staining with ethidium bromide.
Results and Discussion
The facultative intracellular bacterium S. enterica is the most diverse of all the Gram negative pathogenic bacteria considering its host range and the genetics of virulence. The virulence determinants of S. enterica are clustered into characteristic genomic regions known as SPIs (Salmonella pathogenicity islands), while certain genes located on large plasmids are also known to be important in the virulence of this bacterium [17, 22]. Variations reportedly exist among serotypes with respect to the presence or absence of SPIs, a feature predicted to be responsible for host adaptation, expansion of host range and differences in severity of infections by different serotypes [7, 12, 31].
Isolation of Salmonella and PCR Genotyping
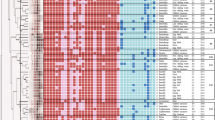
A total of 60 S. Newport were isolated, of which 36 were from shrimp, 15 were from backwater and 9 were from crabs. All S. Newport isolates and 30 clinical isolates of S. Typhi were subjected to PCR genotyping. The results are presented in Table 2. In our study, analysis of clinical isolates of S. Typhi for genes located on seven different SPIs, plasmid-borne and chromosomally-encoded virulence genes revealed that the clinical isolates, by far, are homogenous. The virulence genes invA, hilA located on SPI-1 and other virulence genes not present on SPIs such as stn, fliC, agfA and iroB were detectable in all the isolates in concurrence with previous studies suggesting universal presence of these genes in S. enterica subspecies I [25].
spiC is one of the genes in spiCAB structural component of a type III secretion system encoded on SPI-2 that contributes for intracellular survival and replication of Salmonella [9], while the genes responsible for Mg2+ uptake designated as mgt are present on SPI-3 [4]. All S. Typhi isolates of our study harbored spiC and mgtB as evidenced by PCR results. spi4R, sopB and pagN represent SPIs IV, V and VI, respectively. Except one (NIO-C5), all isolates yielded positive PCR amplicons for spi4R, sopB and pagN. In order to rule out the possibility of sequence variations leading to a negative PCR result or the isolate lacking a single gene within a pathogenicity island, we designed additional primers for spi4R, sopB and pagN (Table 1). We also tested this isolate for other genes associated with SPI-IV (spi4D) and SPI-V (pipA), and the isolate was found to be negative in all these PCR assays. Thus, the isolate (NIO-C5) appears to be deficient in genes of multiple SPIs and can make a good candidate for comparative studies involving genotyping and cells invasion assays. The target gene for SPI-7 was viaB, a component of cluster of genes encoding capsular polysaccharide. We targeted viaB because this locus is present in all Vi antigen-producing S. Typhi unlike the other genes such as viaA present in many serotypes of Salmonella and also in E. coli [32]. viaB was detectable in 22 (73.3%) of all the isolates tested using two sets of primers. SPI-7 is the largest of all the known SPIs and has been associated with serotypes causing systemic infections, though serotype Paratyphi lacks SPI-7 while still being able to cause systemic infection, thus casting doubt on the role of Vi antigen in typhoid fever [23].
The PCR results with environmental isolates, all belonging to Salmonella serotype Newport, was similar and comparable with clinical isolates except for shdA. As in clinical isolates, mgtB, stn, fliC, agfA, invA and hilA were detected in all of the 60 isolates. All isolates lacked plasmid-borne pefA, pefC, spvC and spvR genes. Human-adapted serotypes S. Typhi, Paratyphi A & B, and Salminella Sendai are known to lack virulence plasmids and consequently the spv operon [5]. Our results demonstrate that S. Newport lack spv and pef genes. We analyzed all the isolates of this study for the presence of large plasmids by extracting plasmids from them. While the control strain S. Typhimurium showed the presence of a large plasmid (~90 kb), none of the S. Newport or S. Typhi showed the presence of plasmids. Thus, the absence of spv and pef genes may be correlated with the absence of large plasmids in these isolates.
Among the SPI-associated genes, variations were observed in the incidence of viaB, sopE and shdA (Table 2). viaB and sopE were detected in 66% and 50% of the isolates respectively. These results clearly indicate that irrespective of the source and serotypes, the occurrence of sopE and viaB in Salmonella is variable. However, a clear difference was noticed in the occurrence of shdA between S. Typhi and S. Newport. shdA was detected in all isolates of S. Typhi, but only in 50% of S. Newport isolates. One isolate (BW8) was negative for spi4R, spi4D, sopB, pipA and pagN, apart from being negative for pefA, pefC, spvC and spvR. Two other isolates that showed variable genotypes were BW20 (iroB –, spiC –, ttrC –) and BW22 (spiC –, ttrC −) (data not shown). As in the case of S. Typhi, the absence of a particular gene was confirmed by using two separate primer pairs. In addition, the negative isolates were tested for additional genes of the respective pathogenicity island.
Eighteen isolates were positive for all virulence genes tested barring the plasmid-borne genes. In our study, the variations in genotypes were limited to, mainly, viaB, sopE, and shdA, all known to be highly unstable loci in the genome of Salmonella. Apart from these and the plasmid-borne genes, the isolates were positive for genes associated with PIs I-VI. shdA encodes a thin aggregative fimbrae required for prolonged fecal shedding of Salmonella [18, 19]. The ubiquitous presence of shdA in S. Typhi but not in S. Newport warrants further investigations on whether this gene contributes to any variation in the virulence between these two serotypes.
Antimicrobial Susceptibility
The clinical isolates of S. Typhi were sensitive to the commonly used drugs in the treatment of typhoid fever (data not shown). All clinical isolates were sensitive to tetracycline, quinolone and fluoroquinolone, β-lactam and the cephalosporin antibiotics. However, the antimicrobial resistance phenotypes of S. Newport were very different from S. Typhi (Table 3). The antibiotic susceptibility test revealed the presence of multi-drug resistant S. Newport in the backwater (Table 3). Fifteen isolates (25%) were resistant to ampicillin, 14 (23.3%) to tetracycline, 19 (31.6%) to trimethoprim/sulfamethoxazole, 9 (15%) to ciprofloxacin, 9 each (15%) to cephalothin and cephalexin, 14 (23.3%) to nalidixic acid and 9 (15%) were resistant to chloramphenicol. A study by the Centre for Disease Control and Prevention reported emergence of Newport-MDRAmpC strains resistant ampicillin, chloramphenicol, streptomycin, sulfamethoxazole, and tetracycline [8]. Seven isolates in our study were resistant to ampicillin, chloramphenicol, sulfamethoxazole and tetracycline, but not to streptomycin. Of these, one each was resistant to additional antibiotics kanamycin or norfloxacin. Interestingly, similar antibiotic resistance phenotype was not found among clinical S. Typhi that were resistant only to erythromycin and bacitracin.
Our study is limited to detecting few genes associated with a specific SPI and thus does not explore the possibility of variations within the SPIs. Such variations in SPIs caused by insertions or deletions of specific genes may be important determinants of virulence and host ranges of Salmonella serotypes. Our future study will focus on elucidating such variations within individual SPIs in S. Newport and S. Typhi. Put together, the results of our study show that S. Newport distributed in the environment have similar and comparable virulence genotypes to clinical S. Typhi. However, this observation is based on the distribution of virulence genes known to contribute to the pathogenicity of S. enterica. Comparison of whole genome sequences has identified 11% of the S. Typhimurium LT2 genes absent from the whole genome of S. Typhi [24]. In addition, more than 300 genes confined to the S. enterica subspecies I are predicted to have roles in the host specificity and pathogenicity of Salmonella [24]. Thus, the whole genome comparison using microarray technique is necessary to fully identify variations in gene contents, followed by animal studies to correlate these genetic variations with the virulence phenotype.
In developed countries where scientific monitoring and record keeping is followed, the morbidity due to emerging antibiotic resistant strains and the virulent types is well understood. According to one estimate, Newport MDR-AmpC strains were responsible for >2% of the 1 million cases of salmonellosis in 2001 in the U.S [15]. Studies from India have reported the isolation of multidrug-resistant S. Newport from water, animals, fish and vegetables [20, 33, 34]. Though epidemiological data on S. Newport infections in India are lacking, cases of neonatal meningitis and nursery outbreaks with S. Newport have been documented [21, 30]. The high prevalence of multiple drug resistant Salmonella in the environment as revealed by this study definitely represents significant disease burden in the region under study. Thus, future epidemiological studies in this region need to focus on the contribution of non-typhoidal Salmonella to the morbidity and mortality, sources of contamination and the transmission cycle to contain the endemicity of Salmonella infections.
References
Ausubel FM, Brent R, Kingsten RE, Moore DD, Seidman JG, Smith JA, Struhl K (1995) Short protocols in molecular biology, vol 3. Wiley, New York
Baumler AJ, Tsolis RM, Ficht TA, Adams LG (1998) Evolution of host adaptation in Salmonella enterica. Infect Immun 66:4579–4587
Bäumler AJ, Tsolis RM, van der Velden AW, Stojiljkovic I, Anic S, Heffron F (1996) Identification of a new iron regulated locus of Salmonella typhi. Gene 183:207–213
Blanc-Potard AB, Groisman EA (1997) The Salmonella selC locus contains a pathogenicity island mediating intramacrophage survival. EMBO J 16:5376–5385
Boyd EF, Hartl DL (1998) Salmonella virulence plasmid: Modular acquisition of the spv virulence region by an F-plasmid in Salmonella enterica subspecies I and insertion into the chromosome of subspecies II, IIIa, IV and VII isolates. Genetics 149:1183–1190
Brenner FW, McWhorter-Murlin AC (1998) Identification and serotyping of Salmonella. Centers for Disease Control and Prevention, Atlanta
Bueno SM, Santiviago CA, Murillo AA, Fuentes JA, Trombert AN, Rodas PI, Youderian P, Mora GC (2004) Precise excision of the large pathogenicity island, SPI7, in Salmonella enterica serovar typhi. J Bacteriol 186:3202–3213
Centers for Disease Control and Prevention (2000) National Antimicrobial Resistance Monitoring System: Enteric Bacteria, annual report. http://www.cdc.gov/narms/annual/2000/narms_2000_annual_a.htm
Cirillo DM, Valdivia RH, Monack DM, Falkow S (1998) Macrophage-dependent induction of the Salmonella pathogenicity island 2 type III secretion system and its role in intracellular survival. Mol Microbiol 30:175–188
Clinical and Laboratory Standards Institute (CLSI) (2006) Performance standards for antimicrobial susceptibility testing, 7th edn. CLSI document M7-A7, vol 26, no. 2. CLSI, Wayne
Andrews WH, Hammack T (2007) FDA bacteriological analytical manual. Salmonella, Chap. 5. U.S. Food and Drug Administration, Silver Spring
Ginocchio CC, Rahn K, Clarke RC, Galán JE (1997) Naturally occurring deletions in the centisome 63 pathogenicity island of environmental isolates of Salmonella spp. Infect Immun 65:1267–1272
Gulig PA (1990) Virulence plasmids of Salmonella typhimurium and other Salmonellae. Microb Pathog 8:3–11
Gulig PA, Danbara H, Guiney DG, Lax AJ, Norel F, Rhen M (1993) Molecular analysis of spv virulence genes of the Salmonella virulence plasmids. Mol Microbiol 7:825–830
Gupta A, Fontana J, Crowe C, Bolstorff B, Stout A, Van Duyne S, Hoekstra MP, Whichard JM, Barrett TJ, Angulo FJ, The National Antimicrobial Resistance Monitoring System PulseNet Working Group (2003) Emergence of multidrug-resistant Salmonella enterica serotype Newport infections resistant to expanded-spectrum cephalosporins in the United States. J Infect Dis 188:1707–1716
Harish BN, Menezes GA, Sarangapani K, Parija SC (2006) Fluoroquinolone resistance among Salmonella enterica serovar Paratyphi A in Pondicherry. Indian J Med Res 124:585–587
Hensel M (2004) Evolution of pathogenicity islands of Salmonella enterica. Int J Med Microbiol 294:95–102
Kingsley RA, Santos RL, Keestra AM, Adams LG, Bäumler AJ (2002) Salmonella enterica serotype typhimurium ShdA is an outer membrane fibronectin-binding protein that is expressed in the intestine. Mol Microbiol 43:895–905
Kingsley RA, van Amsterdam K, Kramer N, Bäumler AJ (2000) The shdA gene is restricted to serotypes of Salmonella enterica subspecies I and contributes to efficient and prolonged fecal shedding. Infect Immun 68:2720–2727
Kumar R, Surendran PK, Thampuran N (2009) Distribution and genotypic characterization of Salmonella serovars isolated from tropical seafood of Cochin, India. J Appl Microbiol 106:515–524
Kumari S, Gupta R, Bhargava SK (1980) A nursery outbreak with Salmonella Newport. Indian Pediatr 17:11–16
Marcus SL, Brumell JH, Pfeifer CG, Finlay BB (2000) Salmonella pathogenicity islands: big virulence in small packages. Microbes Infect 2:145–156
McClelland M, Sanderson KE, Clifton SW, Latreille P, Porwollik S, Sabo A, Meyer R, Bieri T, Ozersky P, McLellan M, Harkins CR, Wang C, Nguyen C, Berghoff A, Elliott G, Kohlberg S, Strong C, Du F, Carter J, Kremizki C, Layman D, Leonard S, Sun H, Fulton L, Nash W, Miner T, Minx P, Delehaunty K, Fronick C, Magrini V, Nhan M, Warren W, Florea L, Spieth J, Wilson RK (2004) Comparison of genome degradation in Paratyphi A and Typhi, human-restricted serovars of Salmonella enterica that cause typhoid. Nat Genet 36:1268–1274
McClelland M, Sanderson KE, Spieth J, Clifton SW, Latreille P, Courtney L, Porwollik S, Ali J, Dante M, Du F, Hou S, Layman D, Leonard S, Nguyen C, Scott K, Holmes A, Grewal N, Mulvaney E, Ryan E, Sun H, Florea L, Miller W, Stoneking T, Nhan M, Waterston R, Wilson RK (2001) Complete genome sequence of Salmonella enterica serovar typhimurium LT2. Nature 413:852–856
Ochman H, Groisman EA (1996) Distribution of pathogenicity islands in Salmonella spp. Infect Immun 64:5410–5412
Olsen SJ, Bishop R, Brenner FW, Roels TH, Bean N, Tauxe RV, Slutsker L (2001) The changing epidemiology of Salmonella: trends in serotypes isolated from humans in the United States, 1987–1997. J Infect Dis 183:753–761
Pasmans F, Martel A, Boyen F, Vandekerchove D, Wybo I, Immerseel FV, Heyndrickx M, Collard JM, Ducatelle R, Haesebrouck F (2005) Characterization of Salmonella isolates from captive lizards. Vet Microbiol 110:285–291
Prager R, Fruth A, Tschäpe H (1995) Salmonella enterotoxin (stn) gene is prevalent among strains of Salmonella enterica, but not among Salmonella bongori and other Enterobacteriaceae. FEMS Immunol Med Microbiol 12:47–50
Rahn K, De Grandis SA, Clarke RC, McEwen SA, Galan JE, Ginocchio C, Curtiss R 3rd, Gyles CL (1992) Amplification of an invA gene sequence of Salmonella typhimurium by polymerase chain reaction as a specific method of detection of Salmonella. Mol Cell Probes 6:271–279
Rao MR, Purkayastha SB, Khurana RC, Raghunath D (1991) Salmonella Newport neonatal septicemia. Med J Armed Forces India 47:147–148
Saroj SD, Shashidhar R, Karani M, Bandekar JR (2008) Distribution of Salmonella pathogenicity island (SPI)-8 and SPI-10 among different serotypes of Salmonella. J Med Microbiol 57:424–427
Seth-Smith HMB (2008) SPI-7: Salmonella’s Vi-encoding pathogenicity island. J Infect Dev Ctries 2:267–271
Singh BR, Jyoti J, Chandra M, Babu N, Sharma G (2009) Drug resistance patterns of Salmonella isolates of equine origin from India. J Infect Dev Ctries 3:141–147
Singh BR, Singh P, Verma A, Agrawal S, Babu N, Chandra M, Agarwal RK (2006) A study on prevalence of multi-drug-resistant (MDR) Salmonella in water sprinkled on fresh vegetables in Bareilly, Moradabad, and Kanpur (northern Indian cities). J Public Health 14:125–131
Smith KP, George J, Cadle KM, Kumar S, Aragon SJ, Hernandez RL, Jones SE, Floyd JL, Varela MF (2010) Elucidation of antimicrobial susceptibility profiles and genotyping of Salmonella enterica isolates from clinical cases of salmonellosis in New Mexico in 2008. World J Microbiol Biotechnol 26:1025–1031
Soto SM, Rodríguez I, Rodicio MR, Vila J, Mendoza MC (2006) Detection of virulence determinants in clinical strains of Salmonella enterica serovar Enteritidis and mapping on macrorestriction profiles. J Med Microbiol 55:365–373
Takahashi S, Nagano Y (1984) Rapid procedure for isolation of plasmid DNA and application to epidemiological analysis. J Clin Microbiol 20:608–613
Acknowledgements
The authors are grateful to the Director, NIO, Goa and the Scientist-in-charge, NIO (RC), Cochin for their support and advice. Financial support from suprainstitutional project SIP 1302 (CSIR, India) and GAP 2267 (DST, India) is gratefully acknowledged. We thank the National Salmonella and Escherichia Centre, Central Research Institute, Kasauli, India for serotyping the Salmonella isolates. This is NIO contribution no. 4742.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parvathi, A., Vijayan, J., Murali, G. et al. Comparative Virulence Genotyping and Antimicrobial Susceptibility Profiling of Environmental and Clinical Salmonella enterica from Cochin, India. Curr Microbiol 62, 21–26 (2011). https://doi.org/10.1007/s00284-010-9665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-010-9665-7