Abstract
Purpose
The aim of the present study was to develop a new strategy for combined thermo-chemotherapy of cancer. For this purpose, we used ultrasound waves [1 MHz; 1 W/cm2; 10 min] in combination with a sonosensitizing nanoplatform, named ACA, made of alginate co-loaded with cisplatin and gold nanoparticles (AuNPs).
Methods
Various combinatorial treatment regimens consisting of ultrasound, AuNPs, cisplatin, and ACA nanoplatform were studied in vivo. The CT26 colon adenocarcinoma cell line was used for tumor induction in BALB/c mice. During the ultrasound exposure, we monitored the temperature variations in each treatment group using infrared thermal imaging. Furthermore, tumor metabolism was assessed by [18F]FDG (2-deoxy-2-[18F]fluoro-d-glucose)-positron emission tomography (PET) imaging.
Results
The combination of ultrasound with nanoplatform showed an improved therapeutic efficacy than free cisplatin or ultrasound alone. It was revealed that the examined thermo-chemotherapy protocol has the potential to intensively decrease the metabolic activity of CT26 tumors.
Conclusions
The data obtained in this study confirmed a potent anti-tumor efficacy caused by the ACA nanoplatform and ultrasound combination. It may provide a beneficial cancer therapy strategy in which the thermal and mechanical effects of ultrasound can intensify the therapeutic ratio of conventional chemotherapy methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductions
Chemotherapy, as one of the main cancer therapy modalities, usually induces some serious side effects in cancer patients. Common chemotherapy techniques, due to the lack of specific distribution of drug in tumor tissues, are not capable of destroying cancer cells specifically and affect healthy tissues as well. Nausea and vomiting, peripheral neurological disorders in both acute and chronic forms, myeloid leukemia, high toxicity, and low efficacy are the examples of current chemotherapy method limitations. Therefore, a successful chemotherapy method needs to provide an appropriate way to deliver medications to the cancer cells with less interaction with healthy tissues. In recent years, nanoparticles have been extensively used as drug carriers to promote the efficacy of conventional chemotherapy techniques. Good stability, high biological half-life, reduced complications due to nonspecific drug distribution in healthy tissues, and the availability of drug administration in a variety of ways are the main advantages of using nanoparticles as drug carriers [1,2,3,4].
On the other hand, hyperthermia has been recently used with chemotherapy to sensitize cancer cells to anti-cancer drugs. Hyperthermia has been recently suggested as an additional treatment modality which can be used with other acceptable cancer therapy methods [5,6,7,8,9,10]. In hyperthermia, the malignant tissues are exposed to high temperatures causing them to be destroyed intensively. Hyperthermia also reduces the amount of hypoxia in cancer tissues and acts as an auxiliary treatment modality to increase the sensitivity of cancer cells to chemotherapy [11]. In conventional hyperthermia methods, there is no way to selectively make a difference between the heating of target tissue and the collateral healthy tissues. Therefore, during the hyperthermia procedure, the temperature of healthy tissues increases causing damage. Recently, nanotechnology-based hyperthermia has been introduced as a substitute for the conventional hyperthermia techniques [5, 9, 12]. Nanoparticles can absorb the energy of external sources and locally increase the therapeutic effects. In this modern type of hyperthermia, nanoparticles act as the internal sources of energy inside the tumor and damage cancer tissues more specifically. Different external sources of energy such as lasers, microwaves, and ultrasound waves are currently used in hyperthermia procedures [5]. Ultrasound, as one of the sources of energy in hyperthermia procedures, has an acceptable superiority over the other energy sources because of having good penetration into the body tissues and it can be focused at any depth of the body. Therefore, tumor temperature can be locally increased and the healthy tissues remain intact without any lethal damages [12].
Due to the unique properties of gold nanoparticle (AuNP) as a drug carrier and its great ability to intensify the mechanical and thermal effects of ultrasound waves [8, 9, 12, 13], we designed this study to investigate the combinatorial effects of chemotherapy and ultrasound hyperthermia in the presence of an AuNP-based nanoplatform. For this purpose, we firstly fabricated a nanoplatform, named ACA, made of alginate co-loaded with cisplatin (as the chemotherapy drug) and AuNPs (as the sonosensitizer). Then, we investigated the combinatorial effects of this nanoplatform in the presence of ultrasound in a CT26 tumor model induced in BALB/c mice. Figure 1 illustrates the main procedures applied in the present study at a glance.
Materials and methods
Materials
The ACA nanoplatform (NB-NC-100) was prepared in the R&D department of Nanobon Company (Tehran, Iran), using the protocol reported previously [13]. Then, we characterized the fabricated ACA nanoplatform using transmission electron microscopy (TEM; LEO906-ZEISS) and Malvern Zetasizer Nano ZS-90 instrument.
CT26 colon adenocarcinoma cell line and male BALB/c mice (5–8 weeks old and weighing 20–25 g) were obtained from Pasteur Institute of Iran. Fetal bovine serum (FBS) was purchased from Gibco® (USA). Roswell Park Memorial Institute (RPMI) 1640 cell culture medium, trypan blue powder, penicillin–streptomycin, trypsin–ethylene diamine tetraacetic acid (EDTA), and phosphate buffer saline were purchased from Sigma-Aldrich Company (USA).
Tumor induction
The above-mentioned materials were used for cell culture protocols, as reported elsewhere [6]. CT26 cells were cultured in RPMI 1640 medium with 10% FBS, 100 units/ml penicillin, and 100 µg/ml streptomycin at 37 °C in 5% CO2. The CT26 cells (2 × 106 cells suspended in 200 µl RPMI 1640) were subcutaneously injected to the right flank of BALB/c mice. All the animal experiments were conducted in accordance with guidelines established by the Institutional Animal Care Committee considering NIH guidelines (Principles of laboratory animal care, NIH publication No. 85-23, revised 1985).
In vivo studies
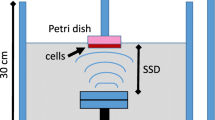
When the average CT26 tumor volume was approximately 150 mm3, we started our in vivo anti-tumor studies. The tumor-bearing mice were randomly divided into eight groups (n = 5) and received various treatments as described in Table 1. The mice were injected intraperitoneally and 6 h post-injection they were irradiated by ultrasound using a Phyaction 190i generator (Phyaction, Germany). To monitor the hyperthermia process in each group that received ultrasound, the transient temperature variations of the tumor were measured using an infrared (IR) thermal camera (Testo 875–1i, Germany).
The tumor volume was measured every 3 days to assess the anti-tumor effect of each treatment modality. The tumor volume was calculated as: \(\frac{\pi }{6}\) × length × (width)2. As a final point, the tumor growth profile of the various treatments was plotted during 21 days of the study span.
PET scan studies
To compare the combinatorial effects of ultrasound hyperthermia and ACA nanoplatform-based chemotherapy, we performed [18F]FDG (2-deoxy-2-[18F]fluoro-d-glucose)-positron emission tomography (PET) imaging using a micro-PET scanner (Xtrim PET). This part of the present study was performed on the 21st day of the study period only for three groups (# 4, 5 and 8 of Table 1). The mice were injected with 200 μCi of [18F]FDG via the tail vein. After 15 min, the animals were anesthetized via an i.p. injection of 100 mg/kg ketamine and 10 mg/kg xylazine. The whole-body PET image acquisition was performed for 20 min in three-dimensional (3D) list mode.
Statistical analysis
One-way ANOVA test was used for statistical analysis and we used the Tukey test at 95% confidence level as a post-test. Statistical analysis was performed using SPSS software (version11). A value of p < 0.05 was considered statistically significant.
Results
Figure 2a shows the typical TEM micrographs of the prepared ACA nanoplatform. The results suggest that the nanoparticles are well dispersed and appear to be spherical in shape. The hydrodynamic size and zeta potential of the nanoparticles were measured using DLS and zeta potential analyzer, respectively. It was determined that the hydrodynamic size of the nanoparticles was 44 nm (Fig. 2b). Zeta potential of the synthesized nanoplatform was − 35.1 mV demonstrating a good particle stability in the colloidal dispersion.

(Reprinted with permission from Ref. [13]. Copyright © 2019 Elsevier)
a TEM images of the ACA nanoplatform shows that AuNPs are coated by alginate hydrogel (arrows indicate alginate coating). b DLS profile shows the effective hydrodynamic size of the nanocomplex to be 44 nm (PDI: 0.38)
After preparation and characterization of the ACA nanoplatform, we started the in vivo experiments. To investigate the anti-tumor effects of different treatment modalities listed in Table 1, the tumor volume changes of the mice in each group were monitored during the study span (Fig. 3). We did not see any significant tumor growth delay for the mice treated with AuNPs alone in comparison to the control group (p value = 0.92). The mice treated with cisplatin alone or ultrasound alone or the combination of these two treatments (ultrasound + cisplatin) showed a significant tumor growth inhibition compared to the control (p < 0.05). Also, we observed that the combination of ultrasound and AuNPs with/without alginate coating induced greater anti-tumor effects in comparison to ultrasound alone (p < 0.05). On day 21, the tumor growth was significantly inhibited by {ultrasound + alginate-coated AuNPs} treatment regimen and the average tumor volume in this group was found to be ~ 6500 mm3, which was smaller than the average tumor volume in the ultrasound group (~ 12000 mm3). There was a black scar on the tumors treated with {ultrasound + alginate-coated AuNPs} regimen, giving an evidence for necrosis of the surface tissue following ultrasound hyperthermia (see Fig. 5). However, the mice in the eighth group (ultrasound + ACA nanoplatform) had the smallest tumor size (~ 2300 mm3), suggesting a better anti-tumor efficacy of AuNPs in combination with cisplatin and ultrasound hyperthermia.
Figure 4 shows the temperature variations in the different treatment groups that received ultrasound irradiation. As seen in Fig. 4, AuNPs caused significant increase in tumor temperate if ultrasound irradiation was received, while cisplatin did not induce any increase in temperature. Interestingly, we observed that ACA nanoplatform highly enhanced the variations of temperature, but there was no significant difference between the presence and the absence of cisplatin inside the ACA nanoplatform.
In addition to macroscopic investigations, we studied the anti-tumor effects of the treatment modalities at a microscopic level using [18F]FDG-PET imaging. Figure 5 shows three representative photographs and the axial [18F]FDG-PET images of the mice receiving various treatments on the last day of the study span (on the 21th day). As seen in Fig. 5, the concentration of [18F]FDG which reflects the metabolic activity of viable tumor cells was significantly lower in the mouse treated by {ultrasound + ACA nanoplatform}, compared to other treatment groups. This shows that the combination of ACA nanoplatform and ultrasound irradiation can significantly decrease the viability of tumor cells.
Discussion
The goal of this study was to develop a new combinatorial cancer treatment strategy taking advantages of sonosensitizing nanoplatforms. To this end, we fabricated an ACA nanoplatform and used ultrasound waves as the external source of energy for the hyperthermia procedure.
In the area of nanotechnology-assisted hyperthermia, laser (as a source of energy) is commonly utilized, but it has some serious limitations. In this area, the main concern relates to the limited penetration depth of light-based treatments which hampers the translation of these modalities in the clinics. The use of nanoparticles in association with ultrasound is an attractive area of research that may provide a safe and advantageous strategy to treat deep-seated tumors. The sonosensitizing properties of nanoparticles, like AuNPs, originate from two separate pathways by which nanoparticles may enhance the thermal and mechanical interactions of ultrasound with tissue [8]. We have discussed these two types of interactions in more detail elsewhere [12]. In fact, the presence of nanoparticles inside the tissues can intensify both types of thermal and mechanical interactions [14]. Nanoparticle type, concentration, size, and ultrasound frequency, intensity, and exposure time are effective in the strength of hyperthermia effects. Wen et al. [15] recently used spherical AuNPs with various sizes ranging from 10 to 300 nm at different concentrations of 11.1, 33.3, 75.0, and 150.0 μmol/L. Then, they applied 60 kHz ultrasound to the samples and monitored the induced temperature variations. They concluded that the larger nanoparticles and the higher concentrations of nanoparticles led to greater temperature increase. They also found that the longer time of ultrasound exposure caused higher temperature. In another study, Dabek et al. [16] studied the effects of magnetic nanoparticles on the temperature profile of a nanoparticles-containing medium exposed to ultrasound. They concluded that iron oxide magnetic nanoparticles, as the sonosensitizers, can receive the ultrasound energy and induce higher temperature in the medium. Recently, we also reported the sonosensitizing effects of nano-graphene oxide (NGO), iron oxide (IONP), and AuNPs. Different conditions of ultrasound irradiation and various concentrations of nanoparticles were tested and finally we concluded that AuNPs have better sonosensitizing efficacy [8, 9]. Accordingly, in the present study, we selected AuNPs to make the ACA nanoplatform a drug containing nanoparticle and sonosensitizer agent.
On the other hand, in the present study, we used nanoparticles-assisted hyperthermia to increase the sensitivity of cancer cells to chemotherapy. Mehtala et al. [17] also confirmed that the combination of mild hyperthermia and AuNPs conjugated to cisplatin can elevate the cell death level in chemotherapy-resistant SKOV3 cell line. There are many similar reports in the literature confirming the same effects when investigators used different chemotherapeutics, nanoparticles, and hyperthermia sources [18, 19].
As we reported in Fig. 4, ultrasound in the presence of AuNPs or alginate-coated AuNPs or ACA nanoplatform can increase the temperature of a tumor > 7 °C. Such an increase in temperature may be attributed to the enhanced ultrasonic attenuation. Also, it has been confirmed that the enhanced ultrasonic attenuation is because of differences between several parameters related to the nanoparticles and their neighboring medium including density, thermal properties, and acoustic impedance [16]. Such outstanding discrepancies result in the enhanced acoustic energy dissipation, leading to localized heat generation and significant thermal damage to the tumor cells as the final consequence. Additionally, the presence of highly thermal conductive nanoparticles, such as AuNPs, inside the tumor increases the thermal diffusion rate of the tumor upon ultrasound irradiation. This would assist heat redistribution within the tumor volume [20]. Taken together, the preferential insertion of the sonosensitizing nanoparticles into a tumor and subsequent ultrasound irradiation would selectively heat up the tumor, while the neighboring normal tissues are kept safe from undesirable thermal destruction. Also, using such a nanotechnology-based hyperthermia approach, cancer cells can be discriminately sensitized to the anti-tumor drugs. These mechanisms sound to be the main reasons of the obtained results in our PET scan studies (reported in Fig. 5).
Conclusion
The aim of present study was to develop a new nanotechnology-based strategy for combined thermo-chemotherapy of cancer. For this purpose, we used 1 MHz ultrasound waves in combination with a nanoplatform made of alginate co-loaded with cisplatin (as the anti-tumor drug) and AuNPs (as a sonosensitizing agent). A considerable tumor growth suppression and significant decrease in metabolic activity of tumor cells (obtained from the PET imaging studies) confirmed a potent anti-tumor efficacy caused by the ACA nanoplatform and ultrasound combination. Accordingly, the treatment protocol suggested and examined in the present study may provide a perceptive cancer therapy strategy in which the thermal and mechanical effects of ultrasound can intensify the therapeutic ratio of current conventional chemotherapy methods.
References
Cho K, Wang X, Nie S, Shin DM (2008) Therapeutic nanoparticles for drug delivery in cancer. Clin Cancer Res 14(5):1310–1316
de Solorzano IO, Alejo T, Abad M, Bueno-Alejo C, Mendoza G, Andreu V, Irusta S, Sebastian V, Arruebo M (2019) Cleavable and thermo-responsive hybrid nanoparticles for on-demand drug delivery. J Colloid Interface Sci 533:171–181
Hashemian A, Eshghi H, Mansoori G, Shakeri-Zadeh A, Mehdizadeh A (2009) Folate-conjugated gold nanoparticles (synthesis, characterization and design for cancer cells nanotechnology-based targeting). Int J Nanosci Nanotechnol 5(1):25–34
Shakeri-Zadeh A, Eshghi H, Mansoori G, Hashemian A (2009) Gold nanoparticles conjugated with folic acid using mercaptohexanol as the linker. J Nanotechnol Progress Int 1:13–23
Beik J, Khademi S, Attaran N, Sarkar S, Shakeri-Zadeh A, Ghaznavi H, Ghadiri H (2017) A nanotechnology based strategy to increase the efficiency of cancer diagnosis and therapy: folate conjugated gold nanoparticles. Curr Med Chem 24(39):4399–4416
Mirrahimi M, Hosseini V, Kamrava SK, Attaran N, Beik J, Kooranifar S, Ghaznavi H, Shakeri-Zadeh A (2018) Selective heat generation in cancer cells using a combination of 808 nm laser irradiation and the folate-conjugated Fe2O3@ Au nanocomplex. Artif Cells Nanomed Biotechnol 46:241–253
Shakeri-Zadeh A, Kamrava SK, Farhadi M, Hajikarimi Z, Maleki S, Ahmadi A (2014) A scientific paradigm for targeted nanophotothermolysis; the potential for nanosurgery of cancer. Lasers Med Sci 29(2):847–853
Beik J, Abed Z, Shakeri-Zadeh A, Nourbakhsh M, Shiran MB (2016) Evaluation of the sonosensitizing properties of nano-graphene oxide in comparison with iron oxide and gold nanoparticles. Phys E 81:308–314
Beik J, Abed Z, Ghadimi-Daresajini A, Nourbakhsh M, Shakeri-Zadeh A, Ghasemi MS, Shiran MB (2016) Measurements of nanoparticle-enhanced heating from 1 MHz ultrasound in solution and in mice bearing CT26 colon tumors. J Therm Biol 62:84–89
Ghaznavi H, Hosseini-Nami S, Kamrava SK, Irajirad R, Maleki S, Shakeri-Zadeh A, Montazerabadi A (2018) Folic acid conjugated PEG coated gold–iron oxide core–shell nanocomplex as a potential agent for targeted photothermal therapy of cancer. Artif Cells Nanomed Biotechnol 46(8):1594–1604
Hauck TS, Jennings TL, Yatsenko T, Kumaradas JC, Chan WC (2008) Enhancing the toxicity of cancer chemotherapeutics with gold nanorod hyperthermia. Adv Mater 20(20):3832–3838
Beik J, Shiran MB, Abed Z, Shiri I, Ghadimi-Daresajini A, Farkhondeh F, Ghaznavi H, Shakeri-Zadeh A (2018) Gold nanoparticle-induced sonosensitization enhances the antitumor activity of ultrasound in colon tumor-bearing mice. Med Phys 45(9):4306–4314
Mirrahimi M, Abed Z, Beik J, Shiri I, Dezfuli AS, Mahabadi VP, Kamrava SK, Ghaznavi H, Shakeri-Zadeh A (2019) A thermo-responsive alginate nanogel platform co-loaded with gold nanoparticles and cisplatin for combined cancer chemo-photothermal therapy. Pharmacol Res 143:178–185
Sviridov A, Andreev V, Ivanova E, Osminkina L, Tamarov K, Timoshenko VY (2013) Porous silicon nanoparticles as sensitizers for ultrasonic hyperthermia. Appl Phys Lett 103(19):193110
Wen D (2013) Nanoparticle-related heat transfer phenomenon and its application in biomedical fields. Heat Transfer Eng 34(14):1171–1179
Dąbek L, Hornowski T, Józefczak A, Skumiel A (2013) Ultrasonic properties of magnetic nanoparticles with an additional biocompatible dextran layer. Arch Acoust 38(1):93–98
Mehtala JG, Torregrosa-Allen S, Elzey BD, Jeon M, Kim C, Wei A (2014) Synergistic effects of cisplatin chemotherapy and gold nanorod-mediated hyperthermia on ovarian cancer cells and tumors. Nanomedicine 9(13):1939–1955
Raoof M, Corr SJ, Zhu C, Cisneros BT, Kaluarachchi WD, Phounsavath S, Wilson LJ, Curley SA (2014) Gold nanoparticles and radiofrequency in experimental models for hepatocellular carcinoma. Nanomed Nanotechnol Biol Med 10(6):1121–1130
Xu Y, Karmakar A, Heberlein WE, Mustafa T, Biris AR, Biris AS (2012) Multifunctional magnetic nanoparticles for synergistic enhancement of cancer treatment by combinatorial radio frequency thermolysis and drug delivery. Adv Healthcare Mater 1(4):493–501
Chol S, Estman J (1995) Enhancing thermal conductivity of fluids with nanoparticles. ASME Publ Fed 231:99–106
Funding
All financial supports received from Iran University of Medical Sciences (Grant no. 29865) and Zahedan University of Medical Sciences (Grant no. 7970) are acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in this study were in accordance with the ethical standards of Iran University of Medical Sciences (IUMS ethics committee, Permit number: IR.IUMS.REC 1395.95-03-30-27720).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Irajirad, R., Ahmadi, A., Najafabad, B.K. et al. Combined thermo-chemotherapy of cancer using 1 MHz ultrasound waves and a cisplatin-loaded sonosensitizing nanoplatform: an in vivo study. Cancer Chemother Pharmacol 84, 1315–1321 (2019). https://doi.org/10.1007/s00280-019-03961-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-019-03961-9