Abstract
Purpose
Mercaptopurine plays a pivotal role in treatment of acute lymphoblastic leukemia (ALL) and autoimmune diseases, and inter-individual variability in mercaptopurine tolerance can influence treatment outcome. Thiopurine methyltransferase (TPMT) and multi-drug resistant Protein 4 (MRP4) have both been associated with mercaptopurine toxicity in clinical studies, but their relative contributions remain unclear.
Methods
We studied the metabolism of and tolerance to mercaptopurine in murine knockout models of Tpmt, Mrp4, and both genes simultaneously.
Results
Upon mercaptopurine treatment, Tpmt −/− Mrp4 −/− mice had the highest concentration of bone marrow thioguanine nucleotides (8.5 pmol/5 × 106 cells, P = 7.8 × 10−4 compared with 2.7 pmol/5 × 106 cells in wild-types), followed by those with Mrp4 or Tpmt deficiency alone (6.1 and 4.3 pmol/5 × 106 cells, respectively). Mrp4-deficient mice accumulated higher concentrations of methylmercaptopurine metabolites compared with wild-type (76.5 vs. 23.2 pmol/5 × 106 cells, P = 0.027). Mice exposed to a clinically relevant mercaptopurine dosing regimen displayed differences in toxicity and survival among the genotypes. The double knock-out of both genes experienced greater toxicity and shorter survival compared to the single knockout of either Tpmt (P = 1.7 × 10−6) or Mrp4 (P = 7.4 × 10−10).
Conclusions
We showed that both Tpmt and Mrp4 influence mercaptopurine disposition and toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mercaptopurine is widely used as an anticancer agent and immunosuppressant in the treatment of leukemia and autoimmune diseases. Dose-limiting toxicities of mercaptopurine, including hematopoietic, hepatic and gastrointestinal (GI) toxicities, were associated with treatment interruptions [1] and inferior outcomes in some studies [2,3,4,5]. Genetic variation in both TPMT and MRP4 have been shown to alter the metabolism and disposition of mercaptopurine. To investigate the impact of deficiency of these two genes on the disposition and toxicity of mercaptopurine in vivo, we developed murine models with combinations of Tpmt and Mrp4 deficiency.
The relationship between mercaptopurine toxicity and thiopurine methyltransferase (TPMT) has been extensively characterized [1, 6]. Erythrocyte TPMT activity is inversely related to the concentration of the active metabolites, thioguanine nucleotides (TGN), after mercaptopurine administration [7]. Heterozygotes who carry one copy of a non-functional TPMT allele have intermediate TPMT activity and moderate toxicity to thiopurines, and the rare homozygous deficient individuals may develop severe thiopurine-induced myelosuppression [6]. Therefore, TPMT-guided dosage individualization of thiopurines is recommended [6, 8].
We have previously established a Tpmt-deficient murine model that recapitulates clinical features of the human TPMT no-function variants [9]. Recently, using genome-wide approaches, we confirmed that TPMT activity is a monogenic trait determined by TPMT genetic polymorphisms [10]. Based on the clinical genotype of TPMT (presence or absence of *2, *3A and *3C variant alleles), we were able to predict TPMT activity with >90% sensitivity and specificity; however, the tolerability of mercaptopurine could not be fully predicted using TPMT genetic tests alone [10]. Other studies [11,12,13,14] also reported inter-individual variations in mercaptopurine toxicity that were not fully explained by TPMT phenotypes and genotypes.
MRP4 (Multi-resistant Protein 4), also designated ABCC4 (ATP-Binding Cassette, Sub-Family C, Member 4), is an efflux transporter of nucleoside monophosphate analogs, including all major thiopurine metabolites [15, 16]. Overexpression of MRP4 in cells conferred resistance to mercaptopurine and thioguanine [15, 17, 18]. A murine model with Mrp4 deficiency confirmed the protective effect of MRP4 against mercaptopurine hematopoietic toxicity by reducing intracellular TGN accumulation [19, 20]. Polymorphisms in MRP4 have been related to increased thiopurine toxicity in patients with ALL [21] and patients with inflammatory bowel disease (IBD) [22]. However, the magnitude of the effect of MRP4 deficiency (or heterozygosity) on thiopurine toxicity relative to TPMT deficiency is not well defined.
Methods
Animals
The generation of Tpmt knockout mice and Mrp4 knockout mice were previously described [9, 23]. Both strains were backcrossed into 129X1/SvJ for five generations. Wild-type, Tpmt −/− Mrp4 +/+ (Tpmt KO), Tpmt +/+ Mrp4 −/− (Mrp4KO), Tpmt −/− Mrp4 −/−(double knockout, DKO) and Tpmt +/− Mrp4 +/− (double heterozygotes, DHET) were used in this study. Mice of all genotypes are indistinguishable by appearance, reproductive capacity, and histology of heart, lungs, liver, kidney, adrenal glands, thymus, spleen, lymph nodes, stomach, small and large intestine, pancreas, adrenals, reproductive organs, brain and bone marrow. All animal experiments were approved by the Institutional Animal Care and Use Committee of St. Jude Children’s Research Hospital.
Chemicals
Mercaptopurine monohydrate was obtained from Acros Organics (Morris Plains, NJ, USA). Thioguanine nucleotides (TGN), mercaptopurine riboside, methylmercaptopurine, methylmercaptopurine riboside and tetracycline were purchased from Sigma (St. Louis, MO, USA). All chemicals and reagents were of high-performance liquid chromatography grade. A folic acid-deficient purified diet for mice was obtained from TestDiet (Richmond, IN, USA). Methotrexate and sulfamethoxazole/trimethoprim oral suspension were purchased from Alpharma (Fort Lee, NJ, USA).
Animal treatment and sample collection
Mice of both genders, aged 8–12 weeks, were used in the study. To mimic the antifolate therapy given to children with leukemia, mice were placed on a folate-deficient diet (containing less than 0.05 ppm residual folic acid). Tetracycline (1 g in 1 L drinking water, 7 days a week) and sulfamethoxazole/trimethoprim (600 mg sulfamethoxazole and 120 mg trimethoprim in 1 L drinking water, 3 days a week) were used to prevent infections.
To compare pharmacokinetics of mercaptopurine in different genotypes, 4 males and 4 females of each genotype were given a single intraperitoneal injection of mercaptopurine at 80 mg/kg. Four hours after administration, bone marrow cells were collected and the intracellular level of thiopurine nucleotides was measured by high-pressure liquid chromatography as previously described [24, 25].
To evaluate the chronic toxicity of mercaptopurine, 10 male and 10 female mice (or 5 males and 5 females as indicated) of each genotype were given mercaptopurine (10 mg/L or 2.5 mg/kg/day, given the estimated water intake) continuously in their drinking water for 6 months. Methotrexate was also administered i.p. at 1 mg/kg/week to mimic the exposure conditions of combination drug therapy [26]. Mice were sacrificed when they completed the 6-month treatment or became moribund. Blood was collected into tubes with anticoagulant, and all organs were dissected and fixed in 10% formalin, embedded in paraffin, sectioned (5 μm) and stained with hematoxylin and eosin (H&E) for screening of any pathologic changes associated with mercaptopurine treatment.
Statistical analysis
Differences in pharmacokinetic data between two genotypes were compared using the Wilcoxon rank-sum test. The Kaplan–Meier method and the log-rank test were used to compare the differences in survival. P < 0.05 was considered statistically significant.
Results
Mercaptopurine pharmacokinetics differed by genotypes
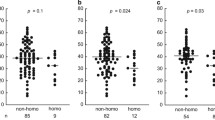
To assess TPMT and MRP4 impact on bone marrow accumulation of mercaptopurine derived nucleotides, mice received a single intraperitoneal injection of mercaptopurine (80 mg/kg), and metabolite levels were determined in bone marrow cells from Tpmt KO, Mrp4 KO and DKO mice. The median TGN levels in mice wild-type for both genes (2.7 pmol/5 × 106 cells) were lower than TpmtKO mice (4.3 pmol/5 × 106 cells, P = 0.021), Mrp4 KO (6.1 pmol/5 × 106 cells, P = 0.011) and DKO mice (8.5 pmol/5 × 106 cells, P = 7.8 × 10−4; (by an average of 37, 56 and 68%, respectively), Fig. 1a). As expected, the methylated metabolites were not detected in TpmtKO and DKO mice. Mrp4 KO mice had over threefold higher median MMPN levels (76.5 pmol/5 × 106 cells) than Mrp4 wild-type (23.2 pmol/5 × 106 cells, P = 0.027; Fig. 1b), indicating greater intracellular accumulation of methylated mercaptopurine metabolites in mice lacking Mrp4. Moreover, DKO, Mrp4 KO and DHET mice had higher intracellular concentrations of mercaptopurine (median = 12.5, 7.5 and 4.8 pmol/5 × 106 cells; Fig. 1c) compared with wild-type mice (median = 0.6 pmol/5 × 106 cells; P = 0.004, 0.047 and 0.048, respectively). The DHETs also tended to have slightly higher median TGN (3.3 pmol/5 × 106 cells) and MMPN levels (35.3 pmol/5 × 106 cells) than wild-types, although the differences were not statistically significant.
Effect of Tpmt and Mrp4 genotype on mercaptopurine nucleotide accumulation in bone marrow. Mice with wild-type (+/+), heterozygous (+/−) or homozygous (−/−) deficiency of Tpmt and/or Mrp4 genes (n = 8 for each genotype) were given a single administration of mercaptopurine (80 mg/kg). At 4 h after injection, bone marrow concentration of a TGN, b MMPN and c mercaptopurine (MP) were measured
Tpmt provided superior protection against chronic oral mercaptopurine toxicity than Mrp4
To mimic clinical regimens used to treat ALL, we next assessed the effect of chronic orally administered mercaptopurine, when combined with a single weekly dose of methotrexate. We provided wild-type, Tpmt KO, Mrp4 KO, DKO and DHET mice with mercaptopurine in their drinking water (equivalent to 2.5 mg/kg/d) and weekly methotrexate injections (1 mg/kg/wk i.p.). All of the wild-type and 80% of the DHET mice survived for the 6-month treatment (Fig. 2). The median duration of survival of the DKOs was only 17 days, followed by that of Tpmt KO (56 days; P = 7.4 × 10−10), which was shorter than that of Mrp4 KO mice (111 days; P = 1.7 × 10−6), suggesting a greater protective effect of Tpmt compared to Mrp4 against chronic orally administered mercaptopurine. In accordance with this, Tpmt KO mice had an average of 23% lower leukocyte counts (P = 0.009), 86% lower neutrophils (P = 4.1 × 10−4), 77% % lower platelets (P = 4.0 × 10−5) and 75% lower erythrocyte counts (P = 8.7 × 10−5) than Mrp4 KO at the end of treatment (Fig. 3). The survival did not differ by sex (Figure S1).
Effect of Tpmt and Mrp4 genotype on survival with chronic mercaptopurine treatment. Mice with wild-type (+/+), heterozygous (+/−) or homozygous (−/−) deficiency for Tpmt and/or Mrp4 received mercaptopurine from the drinking water (10 mg/L) and weekly methotrexate i.p. at 1 mg/kg. Numbers of mice of each genotype are shown. *Log-rank P < 0.01
Hematologic toxicity is impacted by Tpmt and Mrp4. Mice with wild-type (+/+), heterozygous (+/−) or homozygous (−/−) deficiency for Tpmt and Mrp4 genes were given mercaptopurine (10 mg/L) in the drinking water and weekly injections of methotrexate. Blood was collected at the end of 180-day treatment or at the time of sacrifice due to toxicity, and the median treatment duration (days) of each genotype are shown. Empty circles represent outliers, and asterisks (*) indicate significant difference (P < 0.05) compared with wild-types
After chronic mercaptopurine, we performed necropsies on all mice regardless of whether they succumbed to toxicity or completed the 6-month treatment. Severe bone marrow hypocellularity was observed in DKO mice after only 18 days of treatment (Fig. 4a), while the Tpmt KO or Mrp4 KO mice exhibited myelosuppression after 6 weeks and 9 weeks, respectively (Fig. 4b, c). Wild-type mice had only mild to moderate myelosuppression at the end of 6-months of treatment (Fig. 4d). Moreover, 4/4 (100%) DKO, 1/9 (11%) TpmtKO and 1/9 (11%) Mrp4 KO mice had spontaneous CNS hemorrhage (related to severe thrombocytopenia) (Figure S2).
Bone marrow suppression of mice with chronic exposure to mercaptopurine. H&E staining of a markedly hypocellular marrow from a DKO mouse at day 18; b severely hypocellular marrow from a Tpmt −/− mouse at week 6; c moderately hypocellular marrow from an Mrp4 −/− mouse at week 9; d mildly hypocellular marrow from a wild-type mouse. Magnification: 40×. Mice received mercaptopurine from drinking water (10 mg/L) and weekly methotrexate i.p. at 1 mg/kg
GI toxicity that resembled mercaptopurine-induced GI toxicity in patients was also observed (Figure S3). Gastric epithelial hyperplasia, hyperkeratosis and/or ulceration were found in 4 of 9 TpmtKO mice that received at least 30 days of treatment. This was not observed in either Mrp4 KO (n = 9) or wild-type mice (n = 7) that received more than 30 days of treatment. The short survival (<20 days) of DKO mice prevented the evaluation of GI toxicity; however, an exception was one DKO mouse that had a gastric submucosal hemorrhage after 18 days of treatment.
Renal tubular degeneration was observed in mice of all genotypes (12/30, 40%) at the time of sacrifice (Figure S4). Hepatocellular lipidosis was common in mice that received more than 2 months of treatment (Figure S5), including 3 of 9 (33%) Tpmt KO (average duration 77 days), 7 of 9 (78%) Mrp4 KO (average duration 100 days) and 3 of 7 (43%) wild-type mice (average duration 6 months).
Discussion
Mercaptopurine toxicity has been associated with genetic factors, including polymorphisms in TPMT and MRP4 [1, 22]. Deficiency in TPMT results in excessive intracellular accumulation of TGN and severe myelosuppression [7]. Approximately 10% of patients carry one non-functional TPMT allele, and those who inherit homozygous deficiency in TPMT universally experience severe hematopoietic toxicity with conventional mercaptopurine doses [1, 27]. In addition to TPMT, polymorphisms in MRP4 have also been associated with TGN accumulation and hematopoietic toxicity in patients [21, 22]. The frequency of damaging MRP4 variants G2269A, C912A and G559T is higher in the Japanese population compared to people of European ancestry, occurring in 19, 30 and 14%, respectively [19]. Given the high prevalence of variants in these two genes, it is important to know if TPMT and MRP4 act independently or cooperate in protecting against mercaptopurine toxicity.
In the current study, we established preclinical mouse models that investigated how combinations of Tpmt and Mrp4 deficiency impact the type and extent of mercaptopurine toxicity. As expected, both Tpmt and Mrp4 protect against mercaptopurine-induced toxicities. However, the accumulation of cytotoxic TGN shows that each gene acts independently, with the absence of both TPMT and MRP4 producing the greatest intracellular accumulation of TGN. Accordingly, mice lacking both Tpmt and Mrp4 had significantly shorter durations of survival and markedly lower blood counts, indicative of greater hematopoietic toxicity than mice lacking either Tpmt or Mrp4. Notably, mice that were compound heterozygotes of Tpmt and Mrp4 were more susceptible to mercaptopurine than wild-type mice, indicating one functional allele of each gene is not sufficient to fully protect from mercaptopurine toxicity, consistent with greater TGN accumulation in bone marrow cells of these mice.
A clinically relevant oral administration schedule of mercaptopurine revealed that mice with Tpmt deficiency were more susceptible to toxicity than mice that lacked Mrp4 (Figs. 2, 3, 4). This observation is consistent with clinical findings that a homozygous defect of TPMT has a more dramatic effect than that of MRP4 on the hematopoietic toxicity after chronic thiopurine treatment; patients who are homozygous for any TPMT damaging variants (*2, *3A or *3C) only tolerate ~10% of the conventional dose of mercaptopurine [27], while those who are homozygous for any MRP4 damaging variants (G2269A, C912A and G559T) tolerated about 75% of the conventional dose [21]. This was surprising given Mrp4 deficiency resulted in greater accumulation of both cytotoxic TGN and MMPN in bone marrow cells of mice receiving parenteral mercaptopurine (Fig. 1). One possible explanation is that mercaptopurine was administered orally and Mrp4 is known to facilitate the oral absorption of its substrates. For example, previous studies have shown that the Mrp4 substrate, dasatinib, exhibits poor oral absorption in the absence of Mrp4, due to its high expression in the stomach [28]. We postulate that decreased mercaptopurine absorption from the stomach of Mrp4 knockout mice could account for relatively greater tolerance in Mrp4 KO mice compared to TPMT KO mice.
Mercaptopurine is also commonly associated with GI toxicity which can be severe, preventing patients from normal food intake and may have an adverse impact on the therapy [26]. Studies have reported that polymorphisms in TPMT and reduced TPMT activity predisposed patients to thiopurine-induced GI toxicity [11, 29]. In the current study we observed GI toxicity in mice after at least 30 days of oral exposure to low-dose mercaptopurine, and GI toxicity was more severe in mice with Tpmt deficiency compared with Tpmt +/+ mice (Figure S3).
In summary, we showed that Tpmt and Mrp4 both contribute to protecting from mercaptopurine toxicity, with a greater protective effect from Tpmt than Mrp4 following the low-dose chronic oral exposure that is used in the clinic.
References
Relling MV, Hancock ML, Rivera GK, Sandlund JT, Ribeiro RC, Krynetski EY, Pui CH, Evans WE (1999) Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J Natl Cancer Inst 91:2001–2008
McLeod HL, Coulthard S, Thomas AE, Pritchard SC, King DJ, Richards SM, Eden OB, Hall AG, Gibson BE (1999) Analysis of thiopurine methyltransferase variant alleles in childhood acute lymphoblastic leukaemia. Br J Haematol 105(3):696–700
Lennard L, Welch J, Lilleyman JS (1996) Mercaptopurine in childhood leukaemia: the effects of dose escalation on thioguanine nucleotide metabolites. Br J Clin Pharmacol 42(4):525–527
Bhatia S, Landier W, Hageman L, Chen Y, Kim H, Sun CL, Kornegay N, Evans WE, Angiolillo AL, Bostrom B, Casillas J, Lew G, Maloney KW, Mascarenhas L, Ritchey AK, Termuhlen AM, Carroll WL, Wong FL, Relling MV (2015) Systemic exposure to thiopurines and risk of relapse in children with acute lymphoblastic leukemia: a children’s oncology group study. JAMA oncology 1(3):287–295. doi:10.1001/jamaoncol.2015.0245
Relling MV, Hancock ML, Boyett JM, Pui CH, Evans WE (1999) Prognostic importance of 6-mercaptopurine dose intensity in acute lymphoblastic leukemia. Blood 93:2817–2823
Evans WE, Horner M, Chu YQ, Kalwinsky D, Roberts WM (1991) Altered mercaptopurine metabolism, toxic effects, and dosage requirement in a thiopurine methyltransferase-deficient child with acute lymphocytic leukemia. J Pediatr 119:985–989
Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM (1990) Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet 336(8709):225–229
McLeod HL, Krynetski EY, Relling MV, Evans WE (2000) Genetic polymorphism of thiopurine methyltransferase and its clinical relevance for childhood acute lymphoblastic leukemia. Leukemia 14(4):567–572
Hartford C, Vasquez E, Schwab M, Edick MJ, Rehg JE, Grosveld G, Pui CH, Evans WE, Relling MV (2007) Differential effects of targeted disruption of thiopurine methyltransferase on mercaptopurine and thioguanine pharmacodynamics. Cancer Res 67(10):4965–4972
Liu C, Yang W, Pei D, Cheng C, Smith C, Landier W, Hageman L, Chen Y, Yang JJ, Crews KR, Kornegay N, Karol SE, Wong FL, Jeha S, Sandlund JT, Ribeiro RR, Rubnitz JE, Metzger ML, Pui CH, Evans WE, Bhatia S, Relling MV (2016) A genome-wide approach validates that thiopurine methyltransferase activity is a monogenic pharmacogenomic trait. Clin Pharmacol Ther. doi:10.1002/cpt.463
Stocco G, Yang W, Crews KR, Thierfelder WE, Decorti G, Londero M, Franca R, Rabusin M, Valsecchi MG, Pei D, Cheng C, Paugh SW, Ramsey LB, Diouf B, McCorkle JR, Jones TS, Pui CH, Relling MV, Evans WE (2012) PACSIN2 polymorphism influences TPMT activity and mercaptopurine-related gastrointestinal toxicity. Hum Mol Genet 21(21):4793–4804. doi:10.1093/hmg/dds302
Scheuermann TH, Keeler C, Hodsdon ME (2004) Consequences of binding an S-adenosylmethionine analogue on the structure and dynamics of the thiopurine methyltransferase protein backbone. Biochemistry 43(38):12198–12209. doi:10.1021/bi0492556
Fessing MY, Krynetski EY, Zambetti GP, Evans WE (1998) Functional characterization of the human thiopurine S- methyltransferase (TPMT) gene promoter. Eur J Biochem 256(3):510–517
Yang JJ, Landier W, Yang W, Liu C, Hageman L, Cheng C, Pei D, Chen Y, Crews KR, Kornegay N, Wong FL, Evans WE, Pui CH, Bhatia S, Relling MV (2015) Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J Clin Oncol Off J Am Soc Clin Oncol 33(11):1235–1242. doi:10.1200/JCO.2014.59.4671
Wielinga PR, Reid G, Challa EE, van der Heijden I, van Deemter L, de Haas M, Mol C, Kuil AJ, Groeneveld E, Schuetz JD, Brouwer C, De Abreu RA, Wijnholds J, Beijnen JH, Borst P (2002) Thiopurine metabolism and identification of the thiopurine metabolites transported by MRP4 and MRP5 overexpressed in human embryonic kidney cells. Mol Pharmacol 62(6):1321–1331
Schuetz JD, Connelly MD, Sun D, Paibir SG, Flynn PM, Srinivas RV, Kumar A, Fridland A (1999) MRP4: a previously unidentified factor in resistance to nucleoside-based antiviral drugs. Nat Med 5(9):1048–1051
Chen ZS, Lee K, Kruh GD (2001) Transport of cyclic nucleotides and estradiol 17-beta-D-glucuronide by multidrug resistance protein 4. Resistance to 6-mercaptopurine and 6-thioguanine. J Biol Chem 276(36):33747–33754. doi:10.1074/jbc.M104833200
Peng XX, Shi Z, Damaraju VL, Huang XC, Kruh GD, Wu HC, Zhou Y, Tiwari A, Fu L, Cass CE, Chen ZS (2008) Up-regulation of MRP4 and down-regulation of influx transporters in human leukemic cells with acquired resistance to 6-mercaptopurine. Leukemia Res 32(5):799–809. doi:10.1016/j.leukres.2007.09.015
Krishnamurthy P, Schwab M, Takenaka K, Nachagari D, Morgan J, Leslie M, Du W, Boyd K, Cheok M, Nakauchi H, Marzolini C, Kim RB, Poonkuzhali B, Schuetz E, Evans W, Relling M, Schuetz JD (2008) Transporter-mediated protection against thiopurine-induced hematopoietic toxicity. Cancer Res 68(13):4983–4989
Takenaka K, Morgan JA, Scheffer GL, Adachi M, Stewart CF, Sun D, Leggas M, Ejendal KF, Hrycyna CA, Schuetz JD (2007) Substrate overlap between Mrp4 and Abcg2/Bcrp affects purine analogue drug cytotoxicity and tissue distribution. Cancer Res 67(14):6965–6972. doi:10.1158/0008-5472.CAN-06-4720
Tanaka Y, Manabe A, Fukushima H, Suzuki R, Nakadate H, Kondoh K, Nakamura K, Koh K, Fukushima T, Tsuchida M, Koike K, Kiyokawa N, Noguchi E, Sumazaki R, Komiyama T (2015) Multidrug resistance protein 4 (MRP4) polymorphisms impact the 6-mercaptopurine dose tolerance during maintenance therapy in Japanese childhood acute lymphoblastic leukemia. Pharm J 15(4):380–384. doi:10.1038/tpj.2014.74
Ban H, Andoh A, Imaeda H, Kobori A, Bamba S, Tsujikawa T, Sasaki M, Saito Y, Fujiyama Y (2010) The multidrug-resistance protein 4 polymorphism is a new factor accounting for thiopurine sensitivity in Japanese patients with inflammatory bowel disease. J Gastroenterol. doi:10.1007/s00535-010-0248-y
Leggas M, Adachi M, Scheffer GL, Sun D, Wielinga P, Du G, Mercer KE, Zhuang Y, Panetta JC, Johnston B, Scheper RJ, Stewart CF, Schuetz JD (2004) Mrp4 confers resistance to topotecan and protects the brain from chemotherapy. Mol Cell Biol 24(17):7612–7621. doi:10.1128/MCB.24.17.7612-7621.2004
Dervieux T, Chu YQ, Su E, Pui CH, Evans WE, Relling MV (2002) HPLC determination of thiopurine nucleosides and nucleotides in vivo in lymphoblast following mercaptopurine. Clin Chem 48:161–168
Su Y, Hon YY, Chu Y, Van de Poll ME, Relling MV (1999) Assay of 6-mercaptopurine and its metabolites in patient plasma by high-performance liquid chromatography with diode-array detection. J ChromatographyB, Biomed Sci Appl 732(2):459–468
Pui CH, Evans WE (2006) Treatment of acute lymphoblastic leukemia. N Engl J Med 354(2):166–178
Evans WE, Hon YY, Bomgaars L, Coutre S, Holdsworth M, Janco R, Kalwinsky D, Keller F, Khatib Z, Margolin J, Murray J, Quinn J, Ravindranath Y, Ritchey K, Roberts W, Rogers ZR, Schiff D, Steuber C, Tucci F, Kornegay N, Krynetski EY, Relling MV (2001) Preponderance of thiopurine S-methyltransferase deficiency and heterozygosity among patients intolerant to mercaptopurine or azathioprine. J Clin Oncol Off J Am Soc Clin Oncol 19(8):2293–2301
Furmanski BD, Hu S, Fujita K, Li L, Gibson AA, Janke LJ, Williams RT, Schuetz JD, Sparreboom A, Baker SD (2013) Contribution of ABCC4-mediated gastric transport to the absorption and efficacy of dasatinib. Clin Cancer Res Off J Am Assoc Cancer Res 19(16):4359–4370. doi:10.1158/1078-0432.CCR-13-0980
Stolk JN, Boerbooms AM, De Abreu RA, de Koning DG, van Beusekom HJ, Muller WH, van de Putte LB (1998) Reduced thiopurine methyltransferase activity and development of side effects of azathioprine treatment in patients with rheumatoid arthritis. Arthritis Rheum 41(10):1858–1866
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study is supported by National Institutes of Health R01CA194057, R01CA194206, P50 GM115279, and R01 R01CA142665.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, C., Janke, L.J., Yang, J.J. et al. Differential effects of thiopurine methyltransferase (TPMT) and multidrug resistance-associated protein gene 4 (MRP4) on mercaptopurine toxicity. Cancer Chemother Pharmacol 80, 287–293 (2017). https://doi.org/10.1007/s00280-017-3361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3361-2