Abstract
Purpose
Trifluridine (TFT) is an antitumor component of a novel nucleoside antitumor agent, TAS-102, which consists of TFT and tipiracil hydrochloride (thymidine phosphorylase inhibitor). Incorporation of TFT into DNA is a probable mechanism of antitumor activity and hematological toxicity. The objective of this study was to examine the TFT incorporation into tumor- and white blood cell-DNA, and to elucidate the mechanism of TFT-related effect and toxicity. TFT effect on the colony formation of mouse bone marrow cells was also investigated.
Methods
Pharmacokinetics of TFT was determined in nude mice after single oral administration of TAS-102, while the antitumor activity and body weight change were evaluated in the tumor-bearing nude mice after multiple oral administrations for 2 weeks. TFT concentrations in the blood- and tumor-DNA were determined by LC/MS/MS. The colony formation was evaluated by CFU-GM assay.
Results
TFT systemic exposure in plasma increased dose-dependently. The tumor growth rate and body weight gain decreased dose-dependently, but TFT concentrations in the DNA of tumor tissues and white blood cells increased dose-dependently. TFT inhibited colony formation of bone marrow cells in a concentration-dependent manner.
Conclusions
A significant relationship between systemic exposure of TFT and pharmacological effects including the antitumor activity and body weight change was well explained by the TFT incorporation into DNA. TFT inhibited proliferations of mouse bone marrow cells and human colorectal carcinoma cells implanted to nude mice dose-dependently. The highest tolerable TFT exposure provides the highest antitumor activity, and the hematological toxicity may serve as a potential surrogate indicator of TAS-102 efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
TAS-102 is a novel oral nucleoside antitumor agent consisting of trifluridine (TFT) and tipiracil hydrochloride (TPI) at a molar ratio of 1:0.5 and has been approved in Japan for the treatment of patients who have a treatment history of two or more regimens of standard therapy for colorectal adenocarcinoma and are refractory or intolerant to fluoropyrimidine, irinotecan, and oxaliplatin. Yoshino et al. [17] demonstrate that TAS-102 significantly improved the overall survival in the TAS-102 treatment (9.0 months) group, which is compared with placebo (6.6 months) group in their phase 2 study. The study also confirms a manageable safety profile of TAS-102 in the patients, and its major adverse events were hematological toxicity such as neutropenia, leucopenia, and anemia. The recommended dose was determined based on the results of a phase 1 study [4], in which TAS-102 was orally administered at doses ranging from 15 to 35 mg/m2 twice a day in a 28-day cycle consisting of 2 consecutive 1-week cycles (5 days of treatment followed by a 2-day rest period) and subsequent 14-day rest period. Tumor shrinkage was not a useful indicator for the efficacy of TAS-102 in the phase 2 study, because only one out of 112 patients showed a partial response and other 48 patients showed no change in disease conditions. Neutropenia was one of the most common toxicities of TAS-102, and the percentage of decrease in neutrophil count was significantly correlated with the exposure of TFT in patients. The antitumor activity of TAS-102 and neutropenia due to TAS-102 are attributable to the same pharmacological mechanism, that is, TFT incorporation to DNA in tumors and bone marrow cells. Several studies report that chemotherapy-induced neutropenia was significantly correlated with the survival in advanced non-small cell lung cancer, advanced gastric carcinoma, and metastatic colorectal cancer [3, 12, 16]; the results indicate that TAS-102-induced neutropenia is likely to be correlated with the efficacy in colorectal cancer patients, but there remains some uncertainty.
When TFT, which is a thymidine analogue and an antitumor component of TAS-102, was intravenously administered to humans at 27 mg/kg, it was quickly metabolized by thymidine phosphorylase to form trifluorothymine (FTY) [2], followed by rapid elimination with a serum half-life of 18 min in the terminal phase. Since TPI is a potent inhibitor against thymidine phosphorylase, TFT is combined with TPI, in order to enhance metabolic stability and bioavailability of TFT. As expected, plasma TFT concentrations were markedly increased by the co-administration of TPI in monkeys [8], and the combination allows for the exposure of TFT to achieve an effective level in patients.
Once TFT is taken into tumor cells, it rapidly phosphorylated and TFT monophosphate thus formed inhibits thymidylate synthase (TS), which is a rate-limiting enzyme of DNA synthesis; the inhibition of TS is known as an important mechanism for the antitumor activity of nucleoside antitumor agents such as 5-fluorouracil (5-FU) and fluorodeoxyuridine (FdUrd). In addition to the ordinary mechanism (TS inhibition) for the antitumor activity among nucleoside antitumor agents, the sequentially formed TFT triphosphate is known to be incorporated into DNA in tumor cells, which is likely to be a more important mechanism for the antitumor activity of TFT, because TFT was effective against 5-FU- and FdUrd-resistant cancer cell lines, which abundantly express TS [6], and the TFT-dependent inhibition to TS rapidly declined after washout of TFT from the medium in vitro unlike FdUrd [14]. The incorporation of TFT into DNA was consistently much higher than those of 5-FU and FdUrd into DNA in NUGC-3 cells [13, 14], and there was no detectable excision of TFT from DNA by uracil DNA glycosylase, thymine DNA glycosylase, or methyl-CpG binding domain 4, where TFT was pairing to adenine [13]. As a result, it has been hypothesized that the amount of TFT incorporated into DNA was related to both improvement in OS and dose-limiting hematological toxicity (e.g., neutropenia) of TAS-102.
Hematological toxicity has been assessed by using in vitro models in investigative hematopathology and preclinical safety studies. These models are also useful for determining the relative sensitivities of various animal species to hematotoxic effects and for studying the synergistic/antagonistic effects of several compounds [5]. The most frequently observed hematotoxicity is the acute effect of compounds on bone marrow progenitors including granulocyte macrophages (CFU-GM), erythroid (CFU-E), and megacaryocytes (CFU-MK). For several compounds, in vitro/in vivo correlations have been found between the severity of neutropenia and the inhibition of CFU-GM [7, 11].
In this study, we firstly examined the correlation between the systemic exposure of TFT and the concentration of TFT incorporated into the DNA of tumor in a nude mouse bearing human colon cancer xenograft. Secondly, we examined the relationship between the concentrations of TFT incorporated into the DNA in tumors and those of white blood cells. Finally, the inhibition of colony formation of mouse bone marrow cells by TFT was evaluated by a CFU-GM assay.
Materials and methods
Materials
Human colon cancer cell line, KM20C, was kindly provided by the National Cancer Center (Tokyo, Japan). Hydroxypropyl methylcellulose (HPMC) was purchased from Shin-Etsu Chemical Co., Ltd. (Tokyo Japan). TFT and TPI were synthesized by Yuki Gosei Kogyo Co., Ltd. (Tokyo, Japan) and Junsei Chemical (Tokyo, Japan), respectively. FTY was purchased from Tokyo Chemical Industry Co., Ltd. (Tokyo, Japan). TFT and FTY labeled with stable isotope (13C, 15N2-TFT and 13C, 15N2-FTY, respectively) were synthesized by Daiichi Pure Chemicals Co., Ltd. (currently Sekisui Medical Co., Ltd., Tokyo, Japan). 13C, 15N2-TPI was synthesized by Taiho Pharmaceutical Co., Ltd. (Tokyo, Japan).
Animals
Five- and eight-week-old male nude mice (BALB/cA Jcl-nu/nu) were purchased from CLEA Japan Inc. (Tokyo, Japan). They were maintained in accordance with the animal experimental regulations of Taiho Pharmaceutical Co., Ltd. The mice were allowed free access to a commercial diet (CLEA Japan, Inc.) and water (filtered and chlorinated) and acclimated to a 12-h light/12-h dark cycle in a barrier facility.
Cell culture and nude mouse bearing human colon cancer xenograft
KM20C was maintained by serial transplantation in the dorsum of nude mice. About 2-mm3 cubic fragments were implanted subcutaneously into the axilla of nude mice. When the tumor volume was estimated to reach 100–150 mm3, the mice were assigned into the control and treatment groups based on the tumor volume.
Administration and sampling
TAS-102 dosing solution was prepared by dissolving TFT and TPI at the molar ration of 1:0.5 in 0.5 % aqueous solution of hydroxypropyl methylcellulose (HPMC). The dose of TAS-102 was expressed on the amount of TFT. The TAS-102 dosing solution was administrated orally to the mice. For the evaluation of pharmacokinetics (PK), the TAS-102 dosing solution was administered to the mice at 15.5, 62.5, and 150 mg/kg in one dose. Blood was collected from the mice before and at 10, 20, 30, 60, 120, 240, 480, and 1440 min after the administration. Mouse plasma was separated by centrifugation (13,000 rpm, 4 °C, 2 min) and stored at −80 °C until the analysis. Three mice were assigned to each time point. For the evaluation of antitumor activity, nude mice bearing human colon cancer xenografts (KM20C) in the treatment groups were administered the TAS-102 dosing solution at 37.5, 75, and 150 mg/kg once a day for 2 weeks, while the control group had no administration. The first day and the last day were defined as Day 1 and Day 14, respectively. Each group consisted of 6 mice. The tumor volume (TV) and relative tumor volume (RTV) were calculated by the following equations: TV = (width)2 × (length)/2 and RTV = (TV during treatment)/(TV at the start of treatment). The tumor growth inhibition rate (TGI) was calculated by the following equation: TGI (%) = [1 − (mean RTV of the treatment group)/(mean RTV of the control group)]. The body weight (BW) changes were monitored and used as a surrogate measure of side effects and calculated by the following equation: BW changes (%) = [(BW during the treatment) − (BW at the start of the treatment)] × 100/(BW at the start of the treatment). Blood and tumor were collected on Day 15 for the evaluation of TFT concentrations incorporated into the DNA of white blood cells and tumors and stored at −80 °C until analysis. For the mouse bone marrow CFU-GM assay, femurs were isolated from mice and the muscle and other connective tissues were removed. The bone medullary cavity was accessed by removing the epiphysis of the femur located at the end of the bones. A blunt syringe needle (23G) was inserted into the medullary cavity, and the cavity was flushed with 2.5 mL of sterile Iscove’s modified Dulbeco’s medium (Gibco, Invitrogen, Carlsbad, CA) with 2 % fetal bovine serum (FBS) (Gibco, Invitrogen, Carlsbad, CA) until the color of bone shaft became pale. The cell suspension was filtrated with 40-μm cell strainer (BD Falcon, Franklin Lakes, NJ) followed by keeping on ice.
DNA extraction from white blood cell and tumor
DNAs in the blood and tumor were extracted by NucleoSpin Blood L kit (Macherey–Nagel GmbH & Co. KG, Düren, Germany) and by DNA Isolation Kit for Cells and Tissues (Roche Diagnostics GmbH, Mannheim, Germany) without partitioning tumors, respectively. The DNA concentrations were determined based on the absorbance at 260 nm.
Extraction of TFT from DNA of white blood cells and tumor tissues
TFT was extracted from digested DNA by the following method reported previously [14]. Briefly, in the method, the DNA was diluted in the reaction buffer consisting of 100 mM Tris–HCl (pH 7.0), 50 mM NaCl, 2.5 mM CaCl2, 10 mM MgCl2, 1 U DNase I, 40 μg phosphodiesterase I, and 2 U alkaline phosphatase. The reaction solution was incubated at 37 °C for 2 h. The reaction solution was mixed with a one-tenth quantity of the reaction solution of 4.2 N perchloric acid, cooled in the ice for 5 min, and centrifuged (15,000 rpm, 4 °C, 3 min). After the centrifugation, the supernatant was mixed with threefold amount of 4.2 N perchloric acid of 1 M K2HPO4. The solution was cooled in the ice for 5 min followed by centrifugation (15,000 rpm, 4 °C, 3 min) again. The resultant supernatant was separated and stored at −80 °C until the analysis.
Determination of TFT, FTY, and TPI concentrations in mouse plasma
The plasma was mixed with 13C,15N2-TFT and 13C,15N2-FTY, and 1 M hydrochloric acid, to determine TFT and FTY concentrations in mouse plasma. After the sample was mixed with methyl tert-butyl ether, the resultant organic layer was separated and dried under a nitrogen stream. The residue was dissolved with the mobile phase [0.1 % acetic acid–methanol (75:25, v/v)] and analyzed by the LC/MS/MS system (API4000, Sciex Division of MDS, Toronto, Ontario, Canada) with a reverse phase column (CAPCELL PAK C18 MGIIV; 2.0 mm I.D. × 150 mm, 5 μm, Shiseido Co., Ltd, Tokyo, Japan). The quantitative concentrations ranged from 5 (lower limits of quantification, LLOQ) to 5000 ng/mL for both TFT and FTY in plasma.
For the purpose of determining the TPI concentration in the mouse plasma, the plasma was mixed with 13C,15N2-TPI and 0.1 M hydrochloric acid. The sample was applied to Bond ELUT PRS (Agilent Technologies, Palo Alto, CA), activated sequentially with methanol and 0.1 M hydrochloric acid in advance, and the analytes were eluted with 2 % ammonia water/methanol (2:98, v/v). After the eluate was dried under a nitrogen stream, the residue was dissolved with the mobile phase (10 mM ammonium acetate–methanol [90:10, v/v]) and analyzed by API4000 with a reverse phase column (CAPCELL PAK C18 UG120; 2.0 mm I.D. × 150 mm, 5 μm, Shiseido Co., Ltd., Tokyo, Japan). The mobile phase used in the analysis was 10 mM ammonium acetate/methanol (90:10, v/v). The quantitative concentrations ranged from 1 (LLOQ) to 200 ng/mL in plasma. The flow rate of the mobile phase for both analyses was set at 0.2 mL/min in the isocratic mode.
Determination of TFT concentration in digested solution of DNA
For the purpose of determining the TFT concentration in the digested solution of DNA, the solution was mixed with 13C,15N2-TFT and 1 M hydrochloric acid, and the sample was processed in the same way as described for the plasma. The quantitative concentrations for the digested solution ranged from 0.1 (LLOQ) to 100 ng/mL. TFT concentration in DNA was calculated by the following equation: TFT concentration in DNA (pmol/μg DNA) = [TFT concentration in the digested solution (ng/ml)] × 1000/[DNA concentration in the digested solution (mg/L) × molecular weight of TFT].
Bone marrow CFU-GM assay
Mouse bone marrow cells freshly isolated were mixed with IMDM (Gibco, Invitrogen, Carlsbad, CA) with 2 % FBS to make the concentration at 8 or 16 × 106 cells/mL. The cell suspension (0.4 mL) was combined with 3 mL of methylcellulose-based media (MethoCult M3001, StemCell Technologies, Vancouver, BC) containing 1 % methyl cellulose, 30 % FBS, 1 % BSA, 2 mM l-glutamine, and 10 ng/mL GM-CSF with or without TFT, FTY, or AZT, and the mixture was incubated at 37 °C for about 2 weeks. CFU-GM colonies were counted with an inverted microscope.
PK and statistical analysis
PK parameters were calculated by using non-compartmental model in WinNonlin (version 5.2, Pharsight, Mountain View, CA). The plasma concentration below LLOQ was regarded as 0. The AUC values were calculated by the trapezoidal method. Significance tests for the antitumor activity and BW change between the control and treatment groups were performed by using the Dunnett’s test in SAS (version 8.02, SAS Institute Inc., Cary, NC). The relationship was analyzed by JMP (version 8.0.1, SAS Institute Inc., Cary, NC). The IC50 value for TFT and 95 % confidence interval in CFU-GM assay were estimated by nonlinear logistic regression (JMP, version 8.0.1, SAS Institute Inc., Cary, NC).
Results
PK of TFT, FTY, and TPI in nude mice after a single oral administration of TAS-102
PK of TFT, FTY, and TPI were evaluated in the nude mice after single oral administrations of TAS-102 at 15.5, 62.5, and 150 mg/kg. The PK parameters (Cmax, AUC0–t , and AUC0–24h) generally linearly increased in a dose-dependent manner for TFT, TPI (Fig. 1), and FTY (data not shown). TFT was only detectable at 24 h after all the administrations, and the concentrations were close to LLOQ (5 ng/ml).
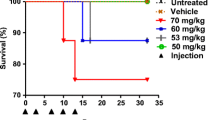
Antitumor activity and BW change in nude mice bearing human colon cancer xenografts during multiple administrations of TAS-102
TAS-102 was repeatedly administered to nude mice bearing human colon cancer xenograft (KM20C) once a day for 2 weeks at oral dose of 37.5, 75, and 150 mg/kg, in order to examine the dose–response relationships with antitumor activity and BW change (Fig. 2). Significant antitumor activity was observed dose-dependently in all of the groups. The values of BW in the treatment groups also decreased dose-dependently, but the average BW of the mice in the 37.5-mg/kg treatment group was not significantly different from that in the control group.
Antitumor activity and body weight change during the multiple oral administrations of TAS-102 to nude mouse xenograft model of human colon cancer (KM20C). TAS-102 was administered orally once a day for 2 weeks to nude mice subcutaneously implanted with human colon cancer, KM20C. The tumor volume (a) and body weight (b) were measured twice a week. The values represent the mean + SD (n = 6). Antitumor activity was evaluated on Day 15, and body weight change was evaluated between Day 0 and Day 15. *P < 0.01 according to Dunnett’s test
Relationships between doses of TAS-102 and TFT concentrations in DNA of white blood cells or tumor tissues
TFT incorporated into DNA was extracted as described in Materials and Methods by using DNase I, phosphodiesterase I, and alkaline phosphatase originating from white blood cells and tumors in the nude mice bearing the xenografts collected on Day 15 after the multiple oral administrations of TAS-102 for 14 days. Almost all the TFT were estimated to disappear from the blood on Day 15 based on the results of PK. The amount of extracted DNA per gram of tumors was comparable among the control and the treatment groups: 5.315 mg in the control group; 5.113 mg in the 37.5-mg/kg treatment group; 4.727 mg in the 75-mg/kg treatment group; and 4.591 mg in the 150-mg/kg treatment group. The concentrations of TFT incorporated into the DNA of tumors (pmol/μg DNA) increased with the increase of dose (Fig. 3a). TFT concentrations in DNA of white blood cells similarly increased in an apparently dose-proportional manner (Fig. 3b). The TFT concentrations in DNA of both tumors and white blood cells correlated with TFT AUC0–24h represented in Fig. 1 (Fig.3c and d, respectively). In addition, there was a statistically significant relationship between the TFT concentrations incorporated into the DNA of tumors and white blood cells (Fig. 4).
Relationship between the doses and concentrations of TFT incorporated into the DNA of tumors (a) or white blood cells (b), and between the systemic TFT exposure and TFT concentration in the DNA of tumors (c) and white blood cells (d). Tumors and white blood cells were harvested from mice subcutaneously implanted with human colon cancer, KM12C, after multiple oral administrations of TAS-102 once a day for 2 weeks. TFT was extracted from DNA obtained from tumors and blood using kits. The TFT exposures (AUC0–24h) for 37.5, 75, and 150 mg/kg of TAS-102 were estimated from the linear regression curve shown in Fig. 1 (AUC0–24h = 342.63 × x + 4362.7, R 2 = 0.9883). The TFT concentration was determined by LC/MS/MS. Each symbol represents the TFT concentration in DNA of materials collected from the individual mice. The lines represent the results of the linear regressions (a R 2 = 0.691, P < 0.0001; b R 2 = 0.5778, P = 0.0003, c R 2 = 0.691, P < 0.0001, d R 2 = 0.5778, P = 0.0003)
Inhibition of TFT against proliferation of mouse bone marrow progenitor cells
Mouse bone marrow progenitor cells were collected from the femurs and cultured with TFT, FTY, or AZT (positive control inhibitor) for 2 weeks. The number of CFU-GM colonies was counted and compared between the control and the treatment groups (Table 1). Percent of control of colony formation was 62.2 ± 8.7 % (Mean ± SEM, n = 3) in the presence of 10 μM TFT, while no colony was observed in the conditions at 30 and 100 μM TFT. There was little effect of FTY on the colony formation under the condition which AZT significantly inhibited the colony formation in a concentration-dependent manner. The value of IC50 for the TFT-mediated inhibition of colony formation was 9.87 ± 0.59 μM (Estimate ± SEM) in the assay with TFT ranging from 0.01 to 300 μM (Fig. 5).
Discussion
Based on the time-courses of antitumor activity and body weight change during multiple oral administrations of TAS-102 at various doses to nude mice bearing KM20C tumors, the present study demonstrates that both antitumor activity and toxicity of TAS-102 were found to closely correlate with the dose and TFT exposure (Cmax, AUC0–t , and AUC0–24h) in plasma. In addition, there were good correlations between the whole TFT concentrations in DNA of tumors (or white blood cells) and plasma, and between the concentrations of TFT incorporated into the DNA of tumors and white blood cells. The IC50 value for the TFT-mediated inhibition of colony formation of mouse bone marrow cells was 9.87 μM, which was similar to the IC50 values for the growth inhibition of human colorectal carcinoma cell lines (H630, 15.8 μM: WiDr, 29.8 μM: Colo320, 15.0 μM) [15]. These results suggest that the exposure-dependent TFT incorporation into DNA was similar between tumors and bone marrow cells, and therefore, the systemic exposure of TFT and/or hematological toxicity of TAS-102 can serve as a surrogate indicator of the antitumor activity for TAS-102.
A significant relationship was observed between the dose (or TFT exposure in plasma) and the concentrations of TFT incorporated into the DNA of both blood and tumors. The TFT concentrations in DNA of tumors were higher than those of white blood cells (Fig. 3); the average TFT concentrations were 13.5 and 2.2 pmol/μg DNA of tumors and white blood cells, respectively, in the group dosed at 150 mg/kg. Granulocytes are the most probable candidate providing TFT-incorporating DNA in white blood cells, which circulate with blood with relatively short turnover time (<3 days, [1]) after they incorporate TFT into their DNA during the proliferation in the bone marrow. The population of the cells containing TFT in their DNA would be actually minor because granulocytes rarely incorporate TFT in the blood. On the other hand, the tumor cells implanted in mice are similarly capable to constantly incorporate and accumulate TFT into their DNA directly from circulating TFT during the proliferation, although the amount of TFT in the DNA would be different among cells. Therefore, it is likely that the concentration of TFT in DNA is higher in tumors than that in white blood cells (Fig. 3).
The concentrations of TFT incorporated into the DNA of tumors were measured after the administration of TAS-102 containing radio-labeled TFT at 150 mg/kg for 2 weeks to mice bearing several tumors including KM20C tumor in a previous study [14]. The concentrations of TFT incorporated into the DNA of human colon cancer (KM20C) in this study were similar to those (10.4–25.7 pmol/μg DNA) reported in the previous study; this indicates that the results obtained from the present analytical method with LC/MS/MS are consistent with those quantified by using radio-labeled TFT and that the present analytical method is useful as an alternative method of the previous one because no radio-labeled TFT and facility for the use of it are needed to measure TFT concentration in DNA.
Systemic exposures (Cmax and AUC) of TFT and TPI after single oral administrations of TAS-102 at 15.5, 62.5, and 150 mg/kg to the nude mice increased linearly with the increase in dose (Fig. 1). The results demonstrate that the combination of TPI with TFT at a molar ratio of 0.5:1.0 will maximize the systemic exposure of TFT and ensure the dose-dependent increase in the TFT exposure by fully inhibiting thymidine phosphorylase activity toward TFT during the first pass metabolism. Little accumulations of TFT and TPI were observed during multiple (once a day) oral administrations of TAS-102 at all dose levels, because the concentrations of TFT in the samples collected at 24 h were close to the LLOQ, which were 1000-fold lower than TFT Cmax (data not shown). Therefore, the systemic exposure of each component of TAS-102 at steady state is calculable from that obtained after a single oral administration of TAS-102.
The safety, activity, and PK of TAS-102 were evaluated with different dosing regimens in phase 1 studies. Systemic TFT exposure in plasma increased dose-dependently, and the hematological toxicity, neutropenia, or granulocytopenia were observed as a dose-limiting toxicity in all of the studies [4, 9, 10]. In those studies, the extent of hematological toxicity indicated a negative correlation with the TFT exposure [4, 10], suggesting that the concentrations of TFT incorporated into the DNA of neutrophils would increase, accompanied by the increases in the TFT exposure, which resulted in a negative correlation between the TFT exposure and the neutrophil count. Actually, only one dose (the highest tolerable dose) was applied as the recommended dose in the phase 2 and subsequent phase 3 studies [17, 18], which demonstrates a significant improvement in the overall survival in comparison with the placebo group in patients with colorectal adenocarcinoma; thus, the median overall survival was 7.1 months (95 % CI 6.5–7.8) in the TAS-102 group and 5.3 months (95 % CI 4.6–6.0) in the placebo group in the phase 3 study. Although the other dose was not evaluated in the phase 2 and 3 studies, the highest tolerable dose is likely to provide the highest TFT concentration in DNA of tumors, leading to the promising efficacy in patients with colorectal cancer.
In conclusion, both antitumor activity and concurrently observed decrease in the BW were correlated dose-dependently with the systemic exposure of TFT during multiple oral administrations of TAS-102, indicating that the activity and toxicity of TAS-102 could be explained by the increases in TFT incorporated into the DNA of tumors and white blood cells, respectively. The TFT concentration in DNA of tumors was also correlated with that of white blood cells. TFT inhibited proliferations of mouse bone marrow cells and human colorectal carcinoma cells implanted to nude mice in a similar dose-dependent manner. These results indicate that the highest tolerable TFT dose (and its exposure in plasma) provides most promising antitumor activity, and therefore, the hematological toxicity may serve as a potential surrogate indicator of the efficacy of TAS-102.
Abbreviations
- AZT:
-
Zidovudine
- TFT:
-
Trifluridine
- C max :
-
Maximum plasma concentration
- AUC:
-
Area under plasma concentration–time curve
- AUC0–t :
-
AUC from time 0 to the time (t) of the last quantifiable concentration
- AUC0–12h :
-
AUC from time 0 to the last time point (12 h)
- TPI:
-
Tipiracil hydrochloride
- BW:
-
Body weight
- LLOQ:
-
Lower limit of quantification
- LC/MS/MS:
-
Liquid chromatography–tandem mass spectrometry
- FTY:
-
Trifluorothymine
- HPMC:
-
Hydroxypropyl methylcellulose
- PK:
-
Pharmacokinetics
- PD:
-
Pharmacodynamics
- TV:
-
Tumor volume
- RTV:
-
Relative tumor volume
- TGI:
-
Tumor growth inhibition rate
References
Basu S, Hodgson G, Katz M, Dunn AR (2002) Evaluation of role of G-CSF in the production, survival, and release of neutrophils from bone marrow into circulation. Blood 100:854–861
Dexter DL, Wolberg WH, Ansfield FJ, Helson L, Heidelberger C (1972) The clinical pharmacology of 5-trifluoromethyl-2′-deoxyuridine. Cancer Res 32:247–253
Di Maio M, Gridelli C, Gallo C, Shepherd F, Piantedosi FV, Cigolari S, Manzione L, Illiano A, Barbera S, Robbiati SF, Frontini L, Piazza E, Ianniello GP, Veltri E, Castiglione F, Rosetti F, Gebbia V, Seymour L, Chiodini P, Perrone F (2005) Chemotherapy-induced neutropenia and treatment efficacy in advanced non-small-cell lung cancer: a pooled analysis of three randomised trials. Lancet Oncol 6:669–677
Doi T, Ohtsu A, Yoshino T, Boku N, Onozawa Y, Fukutomi A, Hironaka S, Koizumi W, Sasaki T (2012) Phase I study of TAS-102 treatment in Japanese patients with advanced solid tumours. Br J Cancer 107:429–434
Du DL, Volpe DA, Grieshaber CK, Murphy MJ Jr (1990) Effects of l-phenylalanine mustard and L-buthionine sulfoximine on murine and human hematopoietic progenitor cells in vitro. Cancer Res 50:4038–4043
Emura T, Suzuki N, Yamaguchi M, Ohshimo H, Fukushima M (2004) A novel combination antimetabolite, TAS-102, exhibits antitumor activity in FU-resistant human cancer cells through a mechanism involving FTD incorporation in DNA. Int J Oncol 25:571–578
Erickson-Miller CL, May RD, Tomaszewski J, Osborn B, Murphy MJ, Page JG, Parchment RE (1997) Differential toxicity of camptothecin, topotecan and 9-aminocamptothecin to human, canine, and murine myeloid progenitors (CFU-GM) in vitro. Cancer Chemother Pharmacol 39:467–472
Fukushima M, Suzuki N, Emura T, Yano S, Kazuno H, Tada Y, Yamada Y, Asao T (2000) Structure and activity of specific inhibitors of thymidine phosphorylase to potentiate the function of antitumor 2′-deoxyribonucleosides. Biochem Pharmacol 59:1227–1236
Hong DS, Abbruzzese JL, Bogaard K, Lassere Y, Fukushima M, Mita A, Kuwata K, Hoff PM (2006) Phase I study to determine the safety and pharmacokinetics of oral administration of TAS-102 in patients with solid tumors. Cancer 107:1383–1390
Overman MJ, Varadhachary G, Kopetz S, Thomas MB, Fukushima M, Kuwata K, Mita A, Wolff RA, Hoff PM, Xiong H, Abbruzzese JL (2008) Phase 1 study of TAS-102 administered once daily on a 5-day-per-week schedule in patients with solid tumors. Invest New Drugs 26:445–454
Parchment RE, Volpe DA, LoRusso PM, Erickson-Miller CL, Murphy MJ Jr, Grieshaber CK (1994) In vivo–in vitro correlation of myelotoxicity of 9-methoxypyrazoloacridine (NSC-366140, PD115934) to myeloid and erythroid hematopoietic progenitors from human, murine, and canine marrow. J Natl Cancer Inst 86:273–280
Rambach L, Bertaut A, Vincent J, Lorgis V, Ladoire S, Ghiringhelli F (2014) Prognostic value of chemotherapy-induced hematological toxicity in metastatic colorectal cancer patients. World J Gastroenterol 20:1565–1573
Suzuki N, Emura T, Fukushima M (2011) Mode of action of trifluorothymidine (TFT) against DNA replication and repair enzymes. Int J Oncol 39:263–270
Tanaka N, Sakamoto K, Okabe H, Fujioka A, Yamamura K, Nakagawa F, Nagase H, Yokogawa T, Oguchi K, Ishida K, Osada A, Kazuno H, Yamada Y, Matsuo K (2014) Repeated oral dosing of TAS-102 confers high trifluridine incorporation into DNA and sustained antitumor activity in mouse models. Oncol Rep 32:2319–2326
Temmink OH, de Bruin M, Comijn EM, Fukushima M, Peters GJ (2005) Determinants of trifluorothymidine sensitivity and metabolism in colon and lung cancer cells. Anticancer Drugs 16:285–292
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M (2007) Predictive value of chemotherapy-induced neutropenia for the efficacy of oral fluoropyrimidine S-1 in advanced gastric carcinoma. Br J Cancer 97:37–42
Yoshino T, Mizunuma N, Yamazaki K, Nishina T, Komatsu Y, Baba H, Tsuji A, Yamaguchi K, Muro K, Sugimoto N, Tsuji Y, Moriwaki T, Esaki T, Hamada C, Tanase T, Ohtsu A (2012) TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol 13:993–1001
Yoshino T, Mayer R, Falcone A et al (2014) Results of a multicenter, randomized, double-blind, phase III study of TAS-102 vs placebo, with best supportive care (BSC) in patients (PTS) with metastatic colorectal cancer (MCRC) refractory to standard therapies (RECOURSE). Ann Oncol 25(suppl 2):ii114
Acknowledgments
We thank Dr. Kiyoshi Morikawa for providing the KM20C cells. All authors are employees of Taiho Pharmaceutical Co., Ltd., the company that developed TAS-102.
Conflict of interest
Authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamashita, F., Komoto, I., Oka, H. et al. Exposure-dependent incorporation of trifluridine into DNA of tumors and white blood cells in tumor-bearing mouse. Cancer Chemother Pharmacol 76, 325–333 (2015). https://doi.org/10.1007/s00280-015-2805-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2805-9