Abstract
Purpose
TAS266 is a novel agonistic tetravalent Nanobody® targeting the DR5 receptor. In preclinical studies, TAS266 was more potent than a cross-linked DR5 antibody or TRAIL. This first-in-human study was designed to evaluate the safety and tolerability, maximum tolerated dose, pharmacokinetics, pharmacodynamics, immunogenicity, and preliminary efficacy of TAS266.
Methods
Adult patients with advanced solid tumors were to receive assigned doses of TAS266 (3, 10, 15, or 20 mg/kg) intravenously on days 1, 8, 15, and 22 of a 28-day treatment cycle.
Results
Grade ≥3 elevations in aspartate aminotransferase and/or alanine aminotransferase levels, occurring during cycle 1 in three of four patients at the 3 mg/kg dose level, were attributed to TAS266 and led to early study termination. Liver enzyme levels quickly returned to grade ≤1 following TAS266 discontinuation. Evidence of preexisting antibodies able to bind to TAS266 was found in the three patients who experienced these dose-limiting toxicities. Immunogenic responses remained elevated and strengthened at end-of-treatment (EOT). In the one patient who did not develop hepatotoxicity, no evidence of immunogenicity was observed at baseline or following administration of 4 TAS266 doses; however, incipient positive immunogenicity was observed at the EOT visit.
Conclusion
TAS266 was associated with unexpected, significant but reversible hepatotoxicity. Although the underlying mechanism is not fully elucidated, factors including the molecule’s high potency, immunogenicity to TAS266, and possibly increased DR5 expression on hepatocytes further enhancing the activity of the Nanobody® may have contributed to enhanced DR5 clustering and activation of hepatocyte apoptosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoring sensitivity to and exploiting the induction of apoptosis as a means to eradicate cancer cells is considered an attractive anticancer strategy. As a result, tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) and TNF-family death receptors, DR4 and DR5, have received considerable attention, primarily because of their ability to induce rapid caspase-dependent apoptosis in a tumor cell-selective manner in preclinical studies [1–6]. TRAIL induces apoptosis through trimerization of its DR4 and DR5 receptor, leading to the formation of the death-inducing signaling complex (DISC), which ultimately results in caspase activation and initiation of apoptosis [7–10].
Compounds targeting DR5 in clinical development have involved either soluble recombinant human Apo2L/TRAIL ligand or conventional bivalent DR5 agonist antibodies [11–16]. Despite promising preclinical data, results from single and combination chemotherapy clinical studies have been generally unimpressive.
Nanobodies® (Ablynx, Belgium) are a novel class of therapeutic proteins based on high affinity single variable domains (VHH) derived from heavy chain antibodies, occurring naturally in camelids, which can be linked to form multivalent molecules (Fig. 1) [17]. TAS266, a novel agonistic 60 kDa Nanobody® that targets the DR5 receptor, is tetravalent, consisting of four identical humanized VHH antibody fragments connected through three linkers of 35 amino acids each. Each VHH monomer domain of TAS266 can bind with high affinity to a DR5 molecule, and the tetravalent TAS266 can potentially cluster 4 DR5 molecules or bridge 2 DR5 trimers, initiating more rapid DISC formation and downstream apoptotic signaling as compared with other conventional DR5 agonists or TRAIL (Fig. 2). The tetravalent structure circumvents the need for secondary receptor cross-linking, a potential drawback of the conventional monoclonal agonist antibodies, and improves receptor clustering, potentially enhancing TAS266 potency as a DR5 agonist.
Preclinical testing suggested that TAS266 was safe and possessed highly potent in vivo biologic and pharmacologic activities. In human tumor cell death assays, TAS266 was ≥1000-fold more potent when compared with a cross-linked DR5 antibody LBY135 or TRAIL [17]. In vivo, TAS266 elicited single-dose tumor regressions in multiple human tumor xenograft models. Furthermore, administration of weekly TAS266 resulted in superior anti-tumor activity in vivo compared with a DR5 agonist antibody in patient-derived pancreatic and colon xenograft models [17]. These data supported further clinical development of TAS266.
DR5 receptors are differentially expressed; they are upregulated in a range of tumors but also expressed at low levels on normal hepatocytes [18]. Toxicology studies performed in cynomolgus monkeys, where binding affinity of TAS266 to DR5 is comparable to humans, indicated no clinical or histopathologic evidence of target organ toxicity with doses up to the highest non-severely toxic dose (HNSTD) of 200 mg/kg administered twice weekly, with similar findings in animals with or without preexisting or treatment-emergent TAS266-binding IgG antibodies. In particular, caspase immunohistochemistry of liver tissue was negative. In addition, bioactivity of TAS266 was maintained (data on file, Novartis Pharmaceuticals). Preliminary data on preexisting IgG binding to TAS266 in human serum were obtained by screening sera in an immunogenicity sandwich ELISA. Overall, a majority of these samples [57 % in healthy donors (n = 88) and 80 % in colorectal cancer patients (n = 40), respectively, data on file Novartis Pharmaceuticals] demonstrated preexisting TAS266-binding IgG antibodies. Of relevance, the presence of human anti-VH autoantibodies (HAVH), a novel type of autoantibody in humans that binds a cryptic epitope in the VH domain of human IgG and interacts with heavy chain therapeutic domain antibodies, was reported in approximately 50 % of healthy human subjects in a study evaluating an anti-TNFR1 VH domain antibody [19]. Autoantibodies to other antibody-derived fragments have been reported and may constitute different immunological entities, depending on the biotherapeutic under study [20, 21]. Thus, the presence of preexisting antibodies in patients enrolled in the first-in-human study might be anticipated. The primary objective of this multicenter, open-label, single-arm study of TAS266 was to estimate the maximum tolerated dose (MTD) or the recommended dose for expansion (RDE) and the associated dose-limiting toxicities (DLTs) of TAS266 when administered intravenously (IV) in patients with relapsed or refractory solid tumors. The secondary endpoints included safety and tolerability, immunogenicity, antitumor activity, and pharmacokinetics (PK) of TAS266 following single and multiple doses.
Materials and methods
Patients
Adults with pathologically confirmed advanced solid tumors were included in this study. Key eligibility criteria included: an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of ≤2; adequate hematologic, renal, and hepatic function. Key exclusion criteria included: central nervous system tumor involvement; cyclical chemotherapy, wide field radiation therapy, or major surgery within 4 weeks before study treatment; prior anaphylactic or other severe infusion reactions to human immunoglobulin or antibody formulations; impaired cardiac function; previous hepatitis B, hepatitis C, or HIV infection. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and good clinical practice. The protocol was approved by the institutional review boards of the participating institutions. Written informed consent was obtained from all patients.
Study design and treatment
Patients were to be enrolled in cohorts receiving doses of TAS266 (3, 10, 15, or 20 mg/kg) IV over 1 h (±10 min) on days 1, 8, 15, and 22 of a 28-day treatment cycle. A 1-week interval between the first and subsequent patients in each cohort was required. TAS266 was to be continued until a patient experienced unacceptable toxicities, disease progression, withdrawal of consent, failure to comply with study requirements, and/or at the discretion of the investigator or sponsor.
DLTs were defined as any AE or abnormal laboratory value occurring in the first treatment cycle that met either of the following criteria: (1) CTCAE grade ≥3 hematologic or non-hematologic toxicity of any duration related to TAS266 or (2) any hematologic or non-hematologic AE or abnormal laboratory value related to TAS266 that resulted in either a dose delay or interruption for more than 14 days (two consecutive doses) or resulted in permanent discontinuation of TAS266, regardless of severity. Safety and tolerability were assessed at baseline and weekly during treatment. AEs were graded according to the CTCAE version 4.03.
Pharmacokinetics
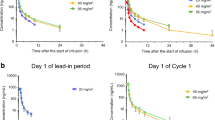
Blood samples for TAS266 concentrations were collected as follows: pre-infusion, end of infusion, and 2, 8, 24, 48, and 72-h post-infusion of the first dose in cycle 1. Pre-infusion PK samples were also collected on days 8, 15, and 22, and at end-of-treatment (EOT). Although PK samples were planned for subsequent cycles, PK samples were only collected in cycle 1 because the study was terminated early due to the occurrence of DLTs in cycle 1. Additional PK samples were collected during the occurrences of these DLTs. Determination of TAS266 in human serum was based on a validated bridging ELISA using target [DR5 extracellular domain (ECD)-IgG-Fc] fusion protein as the capture reagent and biotinylated target (ECD-IgG-FC) as the secondary reagent. The lower limit of quantification was 15 ng/mL in serum. A non-compartmental PK analysis was performed using WinNonlin Phoenix (Pharsight Corporation; Mountain View, CA).
Immunogenicity
Immunogenicity testing to assess the presence and formation of anti-TAS266 antibodies was performed in all enrolled patients. Immunogenicity blood samples were drawn concurrently with TAS266 PK samples pre-infusion on days 1, 8, 15, and 22, and at EOT. Although immunogenicity samples were planned in subsequent cycles, immunogenicity samples were only collected in cycle 1 because the study was terminated early due to the occurrence of DLTs. Additional immunogenicity samples were collected during the occurrences of these DLTs in cycle 1.
Anti-TAS266 IgG antibodies were detected by sandwich ELISA by first immobilizing TAS266 on a microtiter plate. After sample incubation, anti-TAS266 antibodies were detected by horseradish peroxidase (HRP)-conjugated goat antihuman IgG-Fc polyclonal antibody. Due to the high incidence of preexisting antibodies in naive individual sera, only individual sera obviously negative for this were selected to determine the screening cut-point (SCP), confirmatory cut-point (CCP), and sensitivity of the assay. The SCP was calculated as the 95th percentile of 30 individual antidrug antibody (ADA) negative sera. An optical density (OD) value of 0.16 or higher was considered to be a positive screening sample. The CCP, after spiking of individual ADA negative sera with TAS266 5 mg/mL, was defined as the 99th percentile of signal inhibition and was calculated to be 54 %. Assay sensitivity was 329.5 ng/mL based on a monoclonal antibody positive control.
Efficacy Assessments
Tumor responses, using computed tomography (CT) or magnetic resonance imaging (MRI) scans, were determined by investigators according to the response evaluation criteria in solid tumors (RECIST) v1.1. Post-baseline tumor evaluations were planned at the end of even cycles.
Statistical analyses
Escalation with overdose control (EWOC) principle guided by an adaptive Bayesian logistics regression model (BLRM) was used to recommend TAS266 doses [22]. Individual data are presented for each patient. PK measurements were summarized using descriptive statistics.
Results
Patient characteristics and disposition
From June 2012 to September 2012, a total of five patients were enrolled, of whom four received at least one dose of TAS266; the fifth patient was not treated because the study was terminated early. All four patients treated with TAS266 were male and had an ECOG PS of ≤1 and metastatic disease (only one patient had liver metastases). All patients had received ≥2 systemic anticancer therapies including ≥1 monoclonal antibody (Table 1). All four patients received at least one dose of TAS266 3 mg/kg (Fig. 3). Two patients received only the day one dose; one patient received the day 1 and eight doses, and one patient received one cycle of treatment, with dosing on days 1, 8, 15, and 22. At the time of the second DLT occurrence, the 3-mg/kg dose cohort was expanded to six patients, and the BLRM recommended lowering the dose for subsequent patients. Before implementation of a reduced dose, a third patient experienced a DLT. Following this third DLT, treatment was discontinued for all patients, and further enrollment was halted.
Safety and tolerability
Treatment with TAS266 was marked by grade ≥3 aspartate aminotransferase (AST) and/or alanine aminotransferase (ALT) elevations in three of four patients (Table 2; Fig. 3). These three patients experienced grade 3 increases in AST and/or ALT levels within the first 13 days on study, which were considered DLTs related to TAS266. After discontinuing TAS266, liver enzyme levels returned to grade ≤1 within 5–18 days following onset of liver toxicity. Bilirubin levels increased to grade 1 in two patients and returned to normal following TAS266 discontinuation.
Two patients with liver enzyme elevations were symptomatic. In one patient (patient 4), increases in AST and ALT levels progressed to grade 4 and were considered SAEs (Fig. 3d; Table 2). This patient had a concomitant grade 2 increase in serum creatinine, grade 1 increase in total bilirubin, grade 1 edema, and grade 2 weight gain of 10 pounds. At study discontinuation, his total bilirubin had normalized and serum creatinine had improved to grade 1; however, his weight gain had not resolved. The second patient (patient 3) experienced right-sided musculoskeletal chest pain and dizziness, both of which began on the same day he experienced grade 3 liver enzyme elevations. The pain and dizziness resolved, respectively, within 4 and 2 days of onset, coincident with a decline in his liver enzyme levels.
Other treatment-related grade 1 and 2 AEs are listed by patient in Table 2. No dose reductions or infusion-related reactions were reported.
Immunogenicity
Immunogenicity analyses were not performed in real time and were available only after study enrollment had been halted. Clinical decisions regarding patient management were based on AEs and laboratory assessments.
Preexisting antibodies able to bind TAS266 were found to be present at baseline in three of the four patients treated with TAS266 (Table 3). Baseline liver function tests were normal in these patients, with the exception of hypoalbuminemia (grade 1) and increased alkaline phosphatase (grade 1) in one patient. Two of these three patients (patients 1 and 4) experienced DLTs of grade 3 elevated liver enzyme levels within 8 days of receiving the first dose of TAS266 (Fig. 3a, d). These increases in AST/ALT levels coincided with an increase in immunogenicity response with OD values 2.8- and 1.6-fold higher than baseline on day 10 and day 8, respectively (Fig. 3; Table 3). At the end of the study, AST/ALT levels had returned to grade ≤1. Immunogenicity response in these two patients remained significantly higher (three and twofold higher, respectively, based on measured OD values) than at baseline.
The other patient (patient 3) had a 4.4-fold increase in his immunogenicity response (based on measured OD values) on day 9 (measured before administration of the second dose); his liver enzyme levels on that day were normal (Fig. 3c). By day 13, the patient had DLTs of grade 3 elevated liver enzyme levels. Following discontinuation of TAS266, the patient’s liver enzyme levels returned to grade 1, but the immunogenicity response continued to increase and was 6.8-fold higher at EOT compared with baseline based on the OD value.
In the patient who completed treatment cycle 1, no TAS266-related immunogenicity was observed at baseline or before any of the 4 TAS266 doses. This patient’s liver function tests also remained normal throughout the treatment period. At the EOT visit, this patient was noted to have developed a confirmed TAS266-specific positive immunogenicity with an OD value of 0.41 (Fig. 3b; Table 3).
Pharmacokinetics
Following administration of TAS266 3 mg/kg as a 1-hour IV infusion, the median maximum serum concentration (Cmax) occurred 1.06 h (range 1.0–1.1 h) after the end of the infusion (Table 4). Thereafter, the concentration–time profiles declined in a bi-exponential manner, with a median terminal phase half-life (t1/2) of 14.29 h (range 9.7–22.8 h). The mean total systemic clearance (CL) was 0.47 L/hr (standard deviation [SD] 0.12 L/hr). The mean volume of distribution (Vd) was 3.13 L (SD 1.08). IV administration of TAS266 resulted in a low to moderate PK variability (Table 4). There was no correlation between Cmax or mean concentration parameters and observed hepatotoxicity.
Efficacy
Two patients had one post-baseline evaluation, at cycle 1 day 29 (melanoma) and cycle 1 day 15 (laryngeal squamous cell carcinoma), showing stable disease by RECIST v1.1 As these assessments were performed earlier than planned with fewer than the expected number of TAS266 doses delivered, the efficacy of TAS266 could not be determined.
Discussion
This first-in-human study of TAS266 was terminated early following the occurrence of DLTs of grade ≥3 increases in liver enzyme levels in cycle 1 in three of four patients enrolled in the first dose level (3 mg/kg). All three patients who developed hepatotoxicity had normal baseline liver enzyme levels, no hepatic metastases, and no history of hepatitis, active infection, or alcoholism. The starting dose of 3 mg/kg was based on the HNSTD, with a tenfold safety margin, the predicted minimal biological effect level (MABEL), and historical safety information on target binding. No DLT was anticipated at the planned provisional dose levels. The temporal relationship to TAS266 dose administration was indicative of drug-induced hepatotoxicity and was unexpected, particularly since TAS266 had not shown hepatotoxicity in preclinical safety studies in cynomolgus monkeys nor in ex vivo human hepatocyte culture assays.
All three patients who developed a DLT had preexisting antibodies, which bind to TAS266 based on OD values at baseline. The patient without liver enzyme AEs had no evidence of immunogenicity at baseline. In this patient, immunogenicity developed after four doses of TAS266, suggesting repeated exposure to TAS266 was required in this patient for the development of ADAs that may have potentially led to the hepatotoxicity with continued treatment. As a class of agents, significant hepatocyte toxicity or immunogenicity has been reported infrequently with other DR5 antibody agonists, despite preclinical evidence for a role of DR5 in liver injury [6, 11–14, 23–28]. Importantly, grade 3 or 4 elevations in liver enzyme levels were reported in 5.4 % (n = 2) and 4 % (n = 2) of patients receiving lexatumumab (DLT at 20 mg/kg, the highest dose administered) and drozitumab, respectively, but neither increase was associated with immunogenicity [12, 25, 26]. The presence of ADAs has been reported in 21.9 % (n = 16) of patients receiving LBY135 and 9 % (n = 10) of patients receiving dulanermin, the recombinant ApoL2/TRAIL; no significant hepatotoxicity was reported with either agent in these patients [11, 13, 28].
Preexisting and treatment-emergent antibodies to TAS266 were present in 28 % of cynomolgus monkeys (data on file Novartis Pharmaceuticals), but their presence did not cause AEs that would preclude patient administration. Importantly, bioactivity of TAS266 in cynomolgus monkeys was maintained despite the presence of ADAs, suggesting the affinity or avidity of TAS266 for DR5 is high enough to overcome interference by ADAs. In screening assays of human sera, the presence of preexisting antibodies to TAS266 was reported in the majority of samples (data on file Novartis Pharmaceuticals). It is possible that preexisting antibodies could form immune complexes with TAS266 that would accumulate in the liver for clearance by the reticuloendothelial system. In the liver, these complexes could potentially bind to DR5 receptors and induce apoptosis in normal hepatocytes, with resultant hepatotoxicity. Notably, no hepatotoxicity and minimal immunogenicity has been reported with bivalent and trivalent Nanobodies® that have been investigated in non-oncology diseases or healthy volunteers [29–32]. Interestingly, Holland and colleagues investigated the effect of HAVH autoantibodies on an anti-TNFR1 VH domain antibody (GSK1995057) in healthy human subjects [19]. Similar to TAS266 immunogenicity, these HAVH autoantibodies were found in about 50 % of subjects. In vitro, HAVH autoantibody/GSK1995057 complexes were shown to activate TNFR1 in concordance with the mode of action. Clinically, the administration of GSK1995057 resulted in mild to moderate cytokine release-like symptoms in subjects positive for preexisting HAVH autoantibodies [19]. These effects were not predicted by in vivo toxicological investigations in cynomolgus monkeys, some of which had similar preexisting VH autoreactivity. Unlike our study, the administration of GSK1995057 to HAVH autoantibody-negative and autoantibody-positive subjects did not result in treatment-induced immunogenicity; antibody levels remained stable irrespective of the HAVH reactivity at baseline [19].
Stress factors including prior chemotherapy or inflammation have been demonstrated to upregulate DR5 and render hepatocytes more sensitive to TRAIL-induced apoptosis in preclinical models [33, 34]. Therefore, DR5 agonists, like TAS266, may bind to more abundant DR5 receptors of stressed liver cells and induce apoptosis of hepatocytes, resulting in hepatotoxicity. This may provide a potential explanation for the difference in toxicity findings between cynomolgus monkeys and patients treated on this study. All three patients with hepatotoxicity entered the study with normal baseline liver function and did not have liver metastases nor a history of hepatitis or alcoholism. Concomitant medications and prior antineoplastic medications were reviewed as potential confounding and/or contributing factors. Use of medications with known liver toxicity (acetaminophen and atorvastatin) were reported in one patient, and prior antineoplastic agents (5-fluorouracil, irinotecan and oxaliplatin) associated with steatohepatitis and hepatocyte damage were reported in the three patients experiencing hepatotoxicity [35, 36]. These prior therapies and their contribution to potential upregulation of DR5 and subsequent toxicity in the three patients is another potential explanation for the findings.
Moreover, multivalent DR5 Nanobodies® are significantly more potent than conventional DR5 agonists preclinically due to their ability to induce more efficient caspase activation [17]. As a tetravalent molecule, TAS266 could potentially cluster 4 DR5 receptors, as opposed to its native trimeric state, or bridge 2 or more DR5 trimers, thereby inducing superclustering. We previously demonstrated that multivalent DR5 Nanobodies® elicit a more rapid and intense apoptotic signaling response in cancer cells through more efficient recruitment of signaling proteins [17]. Thus, the combination of a very active agonist molecule (either alone or possibly complexed with antidrug antibodies) and possibly increased DR5 expression or function on hepatocytes in patients could result in a higher rate of apoptosis, resulting in hepatoxicity [2].
Intravenous administration of TAS266 resulted in a low to moderate PK variability. The mean CL for TAS266 was relatively high, and the median terminal phase t1/2 (14.29 h) was relatively short as was expected for this format. At 3 mg/kg, the mean Vd was 3.13 L, indicating TAS266 had limited distribution into peripheral tissue compartments. These PK characteristics may have contributed to the relatively rapid resolution (within 5–18 days of onset) of the observed liver enzyme toxicities. The mean observed Cmax achieved with 3 mg/kg was predicted by modeling from preclinical studies and was associated with preclinical efficacy. The clinical efficacy of TAS266 could not be adequately determined due to early study termination.
The results of this study show that the current tetravalent Nanobody® TAS266 is not safe for human administration. The underlying mechanism of hepatotoxicity is unknown, but may be related to the combination of a highly active agonist molecule (alone or complexed with antidrug antibodies) and possibly increased DR5 expression on hepatocytes in patients, thereby resulting in a higher level of apoptosis and liver enzyme elevations. The exact role that preexisting or emerging immunogenicity plays in the observed toxicity is unclear, but reinforces the need for exploration of the potential impact of preexisting antibodies on the safety of biotherapeutics on a case by case basis, particularly those with agonist function [20, 21]. Relevant to the development of drugs targeting death receptors is that multimerization of DR5 molecules by multivalent DR5 antibodies could increase the effectiveness of apoptosis initiation, potentially narrowing the therapeutic window and increasing the risk of hepatotoxicity. The development of TAS266 has been halted based on these findings.
References
Ghobrial IM, Witzig TE, Adjei AA (2005) Targeting apoptosis pathways in cancer therapy. CA Cancer J Clin 55:178–194
Ashkenazi A (2002) Targeting death and decoy receptors or the tumor-necrosis factor superfamily. Nat Rev Cancer 2:420–430
Pan G, O’Rourke K, Chinnaiyan AM et al (1997) The receptor for the cytotoxic ligand TRAIL. Science 276:111–113
Roth W, Isenmann S, Naumann U et al (1999) Locoregional Apo2L/TRAIL eradicates intracranial human malignant glioma xenografts in athymic mice in the absence of neurotoxicity. Biochem Biophys Res Commun 265:479–483
Mitsiades CS, Treon SP, Mitsiades N et al (2001) TRAIL/Apo2L ligand selectively induces apoptosis and overcomes drug resistance in multiple myeloma: therapeutic applications. Blood 98:795–804
Ashkenazi A, Pai RC, Fong S et al (1999) Safety and antitumor activity of recombinant soluble Apo2 ligand. J Clin Invest 104:155–162
Duiker WE, Mom CH, de Jong S et al (2006) The clinical of TRAIL. Eur J Cancer 42:2233–2240
Oikonomou E, Pintzas A (2013) The TRAIL of oncogenes to apoptosis. Biofactors 39:343–354
Gonzalvez F, Ashkenazi A (2010) New insights into apoptosis signaling by Apo2L/TRAIL. Oncogene 29:4752–4765
Alamasan A, Ashkenazi A (2003) Apo2L/TRAIL: apoptosis signaling, biology, and potential for cancer therapy. Cytokine Growth Factor Rev 14:337–348
Soria JC, Márk Z, Zaltoukal P et al (2011) Randomized phase II study of dulanermin in combination with paclitaxel, carboplatin, and bevacizumab in advanced non-small-cell lung cancer. J Clin Oncol 29:4442–4451
Wakelee HA, Patnaik A, Sikic BI et al (2010) Phase I and pharmacokinetic study of lexatumumab (HGS-ETR2) given every 2 weeks in patients with advanced solid tumors. Ann Oncol 21:376–381
Sharma S, de Vries EG, Infante JR et al (2014) Safety, pharmacokinetics, and pharmacodynamics of the DR5 antibody LBY135 alone an in combination with capecitabine in patients with advanced solid tumors. Invest New Drugs 32:135–144
Forero-Torres A, Shah J, Wood T et al (2010) Phase I trial of weekly tigatuzumab, an agonistic humanized monoclonal antibody targeting death receptor 5 (DR5). Cancer Biother Radiopharm 25:13–19
Paz-Ares L, Bálint B, de Boer RH et al (2013) A randomized phase 2 study of paclitaxel and carboplatin with or without conatumumab for first-line treatment of advanced non-small-cell lung cancer. J Thorac Oncol 8:329–337
Rocha Lima CM, Bayraktar S, Flores AM et al (2012) Phase Ib study of drozitumab combined with first-line mFOLFOX plus bevacizumab in patients with metastatic colorectal cancer. Cancer Invest 30:727–731
Huet HA, Growney JD, Johnson JA et al (2014) Multivalent nanobodies targeting death receptor 5 elicit superior tumor cell killing through efficient caspase induction. MAbs 6:1560–1570
Hao C, Song JH, His B et al (2004) TRAIL inhibits tumor growth but is nontoxic to human hepatocytes in chimeric mice. Cancer Res 64:8502–8506
Holland MC, Wurthner JU, Morley PJ et al (2013) Autoantibodies to variable heavy (VH) chain Ig sequences in humans impact the safety and clinical pharmacology of a VH domain antibody antagonist of TNF-α receptor 1. J Clin Immunol 33:1192–1203
Xue L, Rup B (2013) Evaluation of pre-existing antibody presence as a risk factor for posttreatment anti-drug antibody induction: analysis of human clinical study data for multiple biotherapeutics. AAPS J 15:893–896
Xue L, Fiscella M, Rajadhyaksha M et al (2013) Pre-existing biotherapeutic-reactive antibodies: survey results within the American Association of Pharmaceutical Scientists. AAPS J 15:852–855
Neuenschwander B, Branson M, Gsponer T (2008) Critical aspects of the Bayesian approach to phase I cancer trials. Stat Med 27:2420–2439
Jo M, Kim TH, Seol DW et al (2000) Apoptosis induced in normal human hepatocytes by tumor necrosis factor-related apoptosis-inducing ligand. Nat Med 6:564–567
Volkmann X, Fischer U, Bahr MJ et al (2007) Increased hepatotoxicity of tumor necrosis factor-related apoptosis-inducing ligand in diseased human liver. Hepatology 46:1498–1508
Plummer R, Attard G, Pacey S et al (2007) Phase 1 and pharmacokinetic study of lexatumumab in patients with advanced cancers. Clin Cancer Res 13:6187–6194
Camidge DR, Herbst RS, Gordon MS et al (2010) A phase I safety and pharmacokinetic study of the death receptor 5 agonistic antibody PRO95780 in patients with advanced malignancies. Clin Cancer Res 16:1256–1263
Demetri GD, Le Cesne A, Chawla SP et al (2012) First-line treatment of metastatic or locally advanced unresectable soft tissue sarcomas with conatumumab in combination with doxorubicin or doxorubicin alone: a phase I/II open-label and double-blind study. Eur J Cancer 48:547–563
Herbst RS, Eckhardt SG, Kurzrock R et al (2010) Phase I dose-escalation study of recombinant human Apo2L/TRAIL, a dual proapoptotic receptor agonist, in patients with advanced cancer. J Clin Oncol 28:2839–2846
Bartunek J, Barbato E, Heyndrickx G et al (2013) Novel antiplatelet agents: ALX-0081, a Nanobody directed towards von Willebrand factor. J Cardiovasc Transl Res 6:363–366
Holz JB, Sargentini-Maier L, De Bruyn S et al (2013) Twenty-four weeks of treatment with a novels anti-IL-6 receptor Nanobody® (ALX-0061) resulted in 84% ACR20 improvement and 58% DAS28 remission in a phase I/II study in RA. Ann Rheum Dis 72(suppl 3):64
Schoen P, Jacobs S, Verschueren K et al (2013) Anti-RANKL Nanobody ALX-0141 shows sustained biomarker inhibition in a phase I study in healthy postmenopausal women. Bone Abstr. doi:10.1530/boneabs.1.PP135
Fleischmann Roy M, Bruyn De et al (2012) A novel individualized treatment approach in open-label extension study of ozoralizumab (ATN-103) in subjects with rheumatoid arthritis on a background of methotrexate. Arthritis Rheum 64(Suppl 10):1311
Corazza N, Kassahn D, Jakob S et al (2009) TRAIL-induced apoptosis: between tumor therapy and immunopathology. Ann N Y Acad Sci 1171:50–58
Mundt B, Wirth T, Zender L et al (2005) Tumour necrosis factor related apoptosis inducing ligand (TRAIL) induces hepatic steatosis in viral hepatitis and after alcohol intake. Gut 54:1590–1596
Pilgrim CH, Thomson BN, Banting S et al (2012) The developing clinical problem of chemotherapy-induced hepatic injury. ANZ J Surg 82:23–29
Ryan P, Nanji S, Pollett A et al (2010) Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol 34:784–791
Acknowledgments
The authors thank Syntaxx Communications, Inc who provided manuscript development and medical writing services, with the support of Novartis Pharmaceuticals Corporation and to Glenda Chambers, the TAS266 study coordinator at South Texas Accelerated Research Therapeutics.
Conflict of interest
SB and ZT are employees of Novartis Pharmaceuticals Corporation. RI, NK, HH, KK, SB, and MH are employees of Novartis Institutes for Biomedical Research. RI, NK, HH, and ZT own stock in Novartis Pharmaceuticals Corporation. START received funding from Novartis Pharmaceuticals Corporation for conduct of this clinical trial by KP and DR. JC and AM have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papadopoulos, K.P., Isaacs, R., Bilic, S. et al. Unexpected hepatotoxicity in a phase I study of TAS266, a novel tetravalent agonistic Nanobody® targeting the DR5 receptor. Cancer Chemother Pharmacol 75, 887–895 (2015). https://doi.org/10.1007/s00280-015-2712-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2712-0