Abstract
Purpose
Axitinib, a potent and selective inhibitor of vascular endothelial growth factor receptors, showed antitumor activity as a single agent against several solid tumor types in Phase II and III trials. This study was conducted to evaluate axitinib pharmacokinetics across a variety of solid tumors.
Methods
The current study analyzed the pharmacokinetics of axitinib in 110 patients with non-small cell lung cancer (NSCLC), thyroid cancer, or melanoma from three Phase II trials plus 127 healthy volunteers, using nonlinear mixed-effects modeling. Boxplots of maximum observed plasma concentration (C max) and area under the plasma concentration–time curve (AUC) of data from these tumor populations was compared to C max and AUC from the final population pharmacokinetic model developed for metastatic renal cell carcinoma (mRCC) to compare axitinib pharmacokinetics across different tumor types.
Results
Axitinib disposition based on data from 237 subjects was best described using a two-compartment model with first-order absorption and lag time. Population estimates for systemic clearance, central volume of distribution, absorption rate constant, absolute bioavailability, and lag time were 20.1 L/h, 56.2 L, 1.26/h−1, 0.663, and 0.448 h, respectively. Statistically significant covariates included gender on clearance, and body weight on central volume of distribution. However, predicted changes due to gender and body weight were found not clinically meaningful. The final analysis indicated that the pharmacokinetic model for mRCC was able to successfully describe axitinib pharmacokinetics in patients with NSCLC, thyroid cancer, and melanoma.
Conclusion
The pharmacokinetics of axitinib appears to be similar across a variety of tumor types.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axitinib is a potent and selective inhibitor of vascular endothelial growth factor (VEGF) receptors 1, 2, and 3 [1–3]. Axitinib blocked VEGF-mediated endothelial cell survival, tube formation, and downstream signaling pathways in vitro and inhibited angiogenesis and tumor growth in preclinical animal models [1]. In Phase II clinical trials, this antiangiogenic agent showed antitumor activity with acceptable safety profile as a single agent against several different solid tumor types, including metastatic renal cell carcinoma (mRCC), non-small cell lung cancer (NSCLC), thyroid cancer, and melanoma [4–8]. In a randomized pivotal Phase III clinical trial (AXIS) [9] of axitinib versus sorafenib in patients with previously treated mRCC, axitinib demonstrated significantly improved progression-free survival compared with sorafenib, leading to approval of axitinib as second-line therapy for mRCC in the USA, Europe, Japan, and elsewhere.
Pharmacokinetic evaluation of axitinib in a Phase I dose-finding study in patients with advanced solid tumors showed that axitinib plasma concentrations peaked within 2–6 h after oral dosing in the fed state and declined with an effective plasma half-life [10] of 2–5 h [11]. Maximum plasma concentration (C max) and area under the plasma concentration–time curve were linear at doses tested [up to 20 mg twice daily (BID)], and there was a negligible accumulation following multiple dosing [11]. The maximum-tolerated dose was determined to be 5 mg BID, which was recommended as a starting dose for subsequent clinical trials of axitinib. Individualized stepwise dose increases to 7 mg BID, and then to a maximum of 10 mg BID, or decreases to 3 mg BID, and then to 2 mg BID were permitted based on patient tolerability to the drug [12].
Axitinib pharmacokinetics has been studied extensively in over 500 healthy volunteers of different ethnic groups [13–16]. Inter-individual variability (IIV) in axitinib plasma exposure (area under the plasma concentration–time curve) has been observed in both healthy subjects and cancer patients (i.e., 9–62 % coefficient of variation [CV] in healthy volunteers after a single 5-mg dose of axitinib [14, 16] and 39–94 % in patients following multiple doses of axitinib 5 mg BID [11]). In the Phase I dose-finding study [11], dose-limiting toxicities, such as hypertension, were observed at higher doses of axitinib, indicating a potential exposure–toxicity relationship. There have been some reports of an association between pharmacokinetics and clinical outcome and/or toxicities for other tyrosine kinase inhibitors [17, 18]. Therefore, it is important to elucidate factors that may contribute to the IIV of axitinib pharmacokinetics to minimize its toxicities while maximizing the clinical benefits.
A base model (defined as the structural model prior to covariate analysis, including the effect of food and formulation) to describe the pharmacokinetics of axitinib has previously been developed using a nonlinear mixed-effects modeling approach based on pharmacokinetic data from 337 healthy volunteers from 10 Phase I studies [19]. The model was then applied to analyze data from patients with mRCC across three Phase II studies [20]. Although single-agent axitinib has also showed potential clinical benefits [objective response rate (defined as the percent of patients with confirmed complete or partial response according to Response Evaluation Criteria In Solid Tumors) 9–30 %; stable disease lasting longer than 16 weeks 19–38 %] in the treatment of NSCLC [7], thyroid cancer [6], and melanoma [8], the pharmacokinetics of axitinib has not been previously reported in these patient populations. The objectives of the current analysis were to (1) develop a model that describes the pharmacokinetics of axitinib following multiple oral dose administrations in patients with advanced NSCLC, advanced thyroid cancer, and metastatic melanoma, (2) identify covariates that are important determinants of pharmacokinetic variability in these patients, and (3) evaluate axitinib pharmacokinetics across different tumor types by comparing the results of the current population pharmacokinetic analysis with that reported previously for the mRCC population [20].
Patients and methods
Study design and subjects
This pooled population pharmacokinetic analysis was based on data from three Phase II clinical trials of single-agent axitinib in patients with NSCLC, thyroid cancer, or melanoma combined with four Phase I studies in healthy volunteers (Online Resource 1). The four Phase I studies in healthy volunteers included in this analysis were a subset of those used in the previous population pharmacokinetic analysis [19, 20] and were selected since these studies were conducted using the axitinib form IV, the same crystal polymorph used in the three Phase II patient studies. Clinical details of these studies in NSCLC, thyroid cancer, or melanoma patients have been described previously [6–8]. The results of axitinib population pharmacokinetic analysis obtained using data from three Phase II studies in patients with mRCC have been reported previously [20].
Study treatment and pharmacokinetic sampling
In all studies (studies 1–7, summarized in Online Resource 1), axitinib was administered as crystal polymorph form IV film-coated immediate-release tablets. In healthy volunteers (studies 1–4), blood samples were collected, typically at 0 (pre-dose), 1, 1.5, 2, 3, 4, 6, 8, 12, 16, 24, 36, and 48 h after oral administration of a single 5-mg dose of axitinib in the fasted state only (studies 1, 4) or in both the fasted and fed state (studies 2, 3). In one study (study 3), subjects also received 1 mg axitinib intravenously in a cross-over fashion to determine absolute oral bioavailability. In cancer patients (study 5 in NSCLC, study 6 in thyroid cancer, and study 7 in melanoma), axitinib was administered at a starting dose of 5 mg BID in the fasted state (with food in the NSCLC study). In the NSCLC study, the dose could be increased in 2-mg increments up to a maximum of 10 mg BID in patients who had no treatment-related grade >2 adverse events (AE) according to Common Terminology Criteria for Adverse Events version 3.0 and no hypertension during any 2-week period in cycle 1 or 2. Hypertension was defined as at least 2 in-clinic readings of systolic blood pressure >150 mmHg or diastolic blood pressure >90 mmHg, separated by at least 1 h. In the thyroid cancer and melanoma studies, dose could be increased by 20 % if patients did not have treatment-related grade >1 AE (the thyroid cancer study) or grade ≥2 AE (the melanoma study) for 8 weeks, unless the patient was responding to the treatment. Patients experiencing treatment-related grade ≥2 AEs that could not be controlled with supportive treatment had their dose temporarily interrupted and restarted at either the same dose (for grade 2 AE) or 20 % lower (for grade ≥3 AE) dose after resolution. Blood samples for pharmacokinetic analysis were collected from patients within 15 min prior to the morning dose and 1–2 h after dosing on days 1 (not in the NSCLC study), 29, and 57 and every 8 weeks thereafter.
Plasma samples were analyzed for axitinib concentrations using a validated high-performance liquid chromatography with tandem mass spectrometric detection method (Charles River Laboratories; Shrewsbury, MA, USA) [11]. All axitinib-treated subjects with drug concentrations and information on dosing and collection time available from at least one post-dose visit were included in the analysis (Online Resource 1).
Axitinib pharmacokinetic model development
A strategy used for building an axitinib population pharmacokinetic model involved development of a base model and assessment of random effects, followed by evaluation and identification of covariates to be retained in the final model [19]. The first-order estimation method was used for initial model development to gain insight into initial estimates. The first-order conditional estimation method with interaction was used for base model development and covariate testing. All analyses were performed using a nonlinear mixed-effects modeling (NONMEM® VI, level 1.2; ICON Development Solutions: Hanover, MD, USA).
The base model was developed using a two-compartment model defined in terms of systemic clearance (CL), central volume of distribution (V c), peripheral volume of distribution (V p), inter-compartmental clearance (Q), absorption rate constant (k a), absolute bioavailability (F), and lag time for absorption (tlag). The IIV in CL, V c, and k a was modeled using multiplicative exponential random effect of the form,
where θi is the individual value of the population parameter θ, and ηi is the inter-individual random effect assumed to have a mean of zero and a variance ω 2. Residual variability was modeled using the log-transformed error model of the form,
where Y ij denotes the observed concentration for the ith individual at time j and F ij denotes the corresponding predicted concentration. ε ij is the intra-individual residual error with a mean of zero and a variance σ 2. Attempts were made to define a full variance–covariance matrix omega, Ω, for the inter-individual random effects (ω) when possible.
Following validation of the base model and estimation of individual model parameters, relationships between covariates and IIV in CL and V c were explored graphically. Covariates were selected based on scientific and/or clinical interest and prior knowledge, and included gender, race, tumor type, smoking status [a known inducer of cytochrome P450 (CYP)1A2, which is involved in axitinib metabolism], body weight, and age on CL and gender and body weight on V c. Covariates were added to the base model in a stepwise manner. The effect of a categorical covariate x (gender, race, tumor type, and smoking status) with n groups was modeled as,
where θ 0 denotes the population value of the parameter and θ x denotes the fractional change in θ 0 for a group of the population within each category. Continuous covariates (age and body weight) were modeled as multiplicative effects of the form,
where θ 0 denotes the population value of the parameter when x = x median and θ denotes the population value conditional on the value x. When θ x = 1, θ is proportional to x.
For testing of covariates, the stepwise covariate model building tool, Perl-speaks-NONMEM (PsN® version 2.3.1; Karlsson M, Jonsson N, and Hooker A; http://psn.sourceforge.net/) was used, which implemented the forward selection followed by the backward elimination of each covariate to the model [21]. Each relevant parameter–covariate relationship was prepared and evaluated in a univariate manner. Two hierarchical models were compared by the chi-square test of the difference in their respective objective function values (OFV), with the number of degrees of freedom (df) equal to the difference in the number of parameters between two models. A covariate was retained in the forward selection if OFV decreased by at least 3.84 points (P < 0.05; 1 df) and increased by >10.83 points (P < 0.001; 1 df) in the backward elimination step.
Assessment of model adequacy
Throughout model development, goodness of fit of different models to the observed data was assessed using the following criteria: change in OFV, visual inspection of various diagnostic plots, precision of parameter estimates, and reductions in both IIV and residual variability. When evaluating alternative hierarchical structural models, a difference in OFV of 6.64 was considered significant under the likelihood ratio test (n = 1; P < 0.01).
Plots of predicted or individual predicted data versus observed data were evaluated for overt model misspecification. Plots of weighted residuals or conditional weighted residuals (CWRESI) versus time were used to assess randomness around the null line [22]. A comparison of ω 2 between the base and final model was used to determine the reduction in ω 2. The Eta (η; empirical Bayes prediction of the inter-individual random effect)-shrinkage was estimated and used as a diagnostic tool [23].
Validation of the final model
The predictive performance was evaluated by a visual predictive check (VPC) of simulated data. Simulations were conducted using subject characteristics, and dosing and sampling history from the original dataset implemented in Perl-speaks-NONMEM; resulting concentration–time data were summarized as median (50th percentile) and 2.5th and 97.5th percentiles. The general agreement between simulated and observed data, as well as their distributions, was evaluated.
A nonparametric bootstrap procedure using Perl-speaks-NONMEM was performed in order to further investigate bias and precision of the parameter estimates. Bootstrap allows calculation of standard errors and confidence intervals (CIs) of the parameter estimates. In all, 800 replicate datasets were generated by random sampling with replacement, and population parameters for each dataset were estimated and a distribution was derived. The parameter distribution of the bootstrap runs with successful convergence was compared with final model estimates.
Comparison of axitinib population pharmacokinetics across various tumor types
Axitinib population pharmacokinetics in patients with NSCLC, thyroid cancer, or melanoma was first compared using visual inspection of exploratory plots of Eta on axitinib CL across tumor types. In addition, a VPC was conducted using the final model in mRCC patients [20] and overlaying the observed data from patients with NSCLC, thyroid cancer, or melanoma. The final model parameter estimates and covariate effects from the mRCC model were used to simulate plasma concentrations, and resulting concentration–time data were summarized as 2.5th, 50th (median), and 97.5th percentiles. The extent of agreement between the distribution of simulated (mRCC) and observed (NSCLC, thyroid cancer, and melanoma) data was evaluated.
Results
Baseline characteristics of subjects included in axitinib population pharmacokinetic analysis among healthy volunteers and patients with NSCLC, thyroid cancer, or melanoma tumors
Of 257 subjects enrolled in seven studies, 237 subjects (127 healthy volunteers, 30 patients with NSCLC, 57 patients with thyroid cancer, and 23 patients with metastatic melanoma) had evaluable pharmacokinetic data and were included in this analysis (Online Resource 1). Median age and the percentage of females and active or ex-smokers were higher in the three Phase II studies of cancer patients than that in the four Phase I studies in healthy volunteers. The majority of subjects were white, and median body weight was similar across the seven studies. Baseline characteristics of subjects included in the analysis are summarized in Online Resource 2.
Population pharmacokinetic base model
A total of 4,028 plasma concentrations from 237 subjects following either single or multiple administrations of axitinib were available for the population pharmacokinetic analysis. Of the 4,028 observations, 612 (15 %) were below the level of quantification (BLQ, which was 0.1 ng/mL) and were omitted from the analysis since it has previously been showed that inclusion of BLQ samples did not significantly impact the final parameter estimates [24].
Based on prior knowledge, the base model was developed using a two-compartment model with first-order rate absorption and lag time [19]. Since the rate and extent of axitinib absorption has been shown to increase after fasting [11], the effect of food on ka and F was included to improve the stability of the base model. The parameter estimates from the base model are presented in Table 1. The estimates for CL, V c, k a, Q, V p, F, and tlag from the base model were 18.1 L/h, 55.4 L, 1.23 h−1, 1.98 L/h, 59.9 L, 0.667, and 0.448 h, respectively. The IIV in V c was 25.5 %, but IIV in CL and k a were relatively high (52.1 and 85.7 %, respectively). The model predicted that k a and F of axitinib in polymorph form IV would decrease by approximately 65 and 26 %, respectively, when administered with food. The η-shrinkage was found to be adequate (8.2 % for ηCL, 34 % for η Vc, and 24 % for η ka), thus allowing the use of EBEs as a diagnostic tool. The variance–covariance matrix omega, Ω, with inter-individual effects denoted by Eta (η1, η2,…ηi) was explored and refined through the modeling effort. Off diagonal elements were only considered for CL and V c and did not show a significant correlation.
Diagnostic plots from the base model indicated a good agreement between the population or individual predicted and observed concentrations (Online Resource 3a). CWRESI were evenly distributed across the range of observations and displayed no systematic deviation over time (Online Resource 4a). A few observations were identified as potential outliers based on |CWRESI| >6. However, analysis without these outliers did not substantially change pharmacokinetic parameters (i.e., >15 %), and, therefore, they were kept in the final dataset.
Covariates and final model
Following development of the base model and assessment of IIV and residual variability, the effect of additional covariates (body weight, age, smoking status, gender, race, and tumor type) on parameter estimates was first assessed graphically. Visual inspection of Eta plots of parameters from the base model versus each covariate revealed possible correlations between CL and body weight, age, smoking status, gender, race, or tumor type; and between V c and body weight or gender (Online Resource 5). These covariates were then tested sequentially in the forward selection followed by backward elimination process, resulting in gender on CL and weight on V c being statistically significant and retained in the final model. Estimates for CL, V c, k a, Q, V p, F, and tlag in the final model (20.1 L/h, 56.2 L, 1.26 h−1, 2.00 L/h, 63.3 L, 0.663, and 0.448 h, respectively) were comparable to those from the base model (Table 1). The IIV in CL, V c, and k a for the final model were 47.9, 16.9, and 87.4 %, respectively. The η-shrinkage was found to be adequate (8.6 % for ηCL, 24 % for η Vc, and 23 % for η ka).
Of the covariates examined, gender was found to significantly affect CL, whereas body weight substantially impacted V c and was retained in the final model. Thus, the model predicted a 35 % lower CL in female versus male subjects, leading to a proportionately greater plasma exposure in females. Axitinib V c was affected by body weight according to the following relationship,
where Wgt denotes body weight, and 80 is the median body weight for the populations studied. For the range of body weights observed in this pooled analysis (43.5–143 kg), the estimated lower and upper end of V c would be 31.8 and 96.6 L, respectively. The η-shrinkage for CL, V c, and k a (all <24 %) was considered adequate [25]. Results of the covariate analysis are summarized in Fig. 1. The magnitude of any change in axitinib plasma pharmacokinetic parameters that would require a dose modification to the next higher (7 mg BID) or lower (3 mg BID) level (i.e., 40 % higher or lower dose than the starting 5 mg BID) would be considered clinically meaningful. The 95 % CIs for gender on CL/F was contained within or close to the 40 % of the null value, i.e., clinically unimportant region for axitinib. The variation in the error bars for V c in Fig. 1 was likely due to the large range of body weights in the pooled dataset used for the analysis reported here.
Forest plot showing covariate effects on axitinib pharmacokinetic parameter estimates relative to typical (reference) individual. The points and horizontal bars around the points represent the parameter estimates from the bootstrap run and the 95 % CI around that parameter estimates, representing the precision of the estimates. The box and whiskers (Wt on V c) provide effects over the observed covariate range. The gray shaded area represents the area of clinical insignificance (0.6–1.40) relative to the typical individual. CL systemic clearance, k a absorption rate constant, V c central volume of distribution, Wt weight
The effect of gender was further explored by assessing the demographics of male and female subjects for potential imbalance in this analysis. Overall, females were older [median (range) age, 56 (26–84) years] compared with males [40 (18–84) years]. Furthermore, as the age of females increased, the post hoc CL values were lower (Fig. 2). Hence, it is possible that this covariate may be confounded by age, which has been shown to be a significant covariate on CL in mRCC model, especially for those older than 60 years of age [20].
CL parameter estimates versus age, stratified by gender. Median (range) age is 40 (18–85) years for males and 56 (26–84) years for females. Open and closed circles represent individual data points for males and females, respectively. The horizontal solid lines depict smooth (LOESS) trend for males (top) and females (bottom), respectively. The vertical dashed and solid lines indicate median age for males and females, respectively. CL systemic clearance, LOESS locally weighted scatter plot smoothing
Diagnostic plots demonstrated good agreement between the predicted population or individual predicted versus observed concentrations (Online Resource 3b); there was a lack of bias in the residuals as well as in the predicted concentrations over time (data not shown). CWRESI were distributed evenly across the range of concentrations and displayed no systemic deviation over time (Online Resource 4b). Overall, results of the model evaluation demonstrated the adequacy of the final model.
Model evaluation
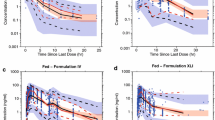
The predictive performance of the final model was validated by a VPC. Simulations with the final model and parameter estimates were conducted, using 1,000 replicates randomly sampled from the original dataset of 237 individuals. The results showed that simulated concentrations generally agreed well with the observed concentrations, with no systematic bias. Thus, the 2.5th, 50th, and 97.5th percentiles of the observed concentrations, stratified by covariates that were found to be significant (i.e., food effect or gender), mostly fell within the 95 % prediction interval of the respective predicted concentrations (Fig. 3).
Visual predictive check of log concentration versus time, stratified by (a) fed (left panel) or fasted (right panel) and (b) male (left panel) or female (right panel). Gray solid lines represent the median and 2.5th and 97.5th percentiles for the observed data; shaded area represents the 95 % prediction interval for simulated data; and circles represent the observed data
The distribution and certainty of the final model parameters were explored using the nonparametric bootstrap procedure (Table 1). The median parameter estimates from the 793 successful bootstrap runs were comparable with those from the original NONMEM run, indicative of lack of bias in the parameters. In addition, the final parameter estimates fell within the 95 % CI of the corresponding parameters obtained from the bootstrap analysis, suggesting the precision of the parameter estimates, a good diagnostic tool for the detection of misspecified parameter distributions.
Comparison of axitinib population pharmacokinetics across various tumor types
The individual values of CL across tumor types and healthy volunteer population are depicted in Fig. 4. Based on visual inspection, these appears to completely overlap. The VPC was performed using the final population pharmacokinetic model from the previously published mRCC model [20] and compared with the observed axitinib concentration data from the current analysis (data not shown).
Eta plots comparing post hoc CL values across different tumor types. The value for HV was from the current analysis and for mRCC was from Rini et al. [20]. CL systemic clearance, HV healthy volunteer, mRCC metastatic renal cell carcinoma, NSCLC non-small cell lung cancer
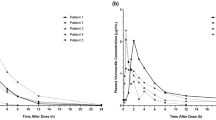
Furthermore, maximum observed plasma concentration and area under the plasma concentration–time curve (from time zero to time tau, where tau is the length of the dosing interval) were estimated for patients included in the current analysis and compared with those estimated for patients with mRCC published previously [20] (Fig. 5). There were no obvious differences.
Boxplots depicting the pharmacokinetic parameters C max and AUCtau for the final mRCC model published previously [20] and the tumor types assessed in the current analysis. AUC tau area under the plasma concentration–time curve from time zero to time tau, where tau is the length of the dosing interval, C max maximum observed plasma concentration, mRCC metastatic renal cell carcinoma
Discussion
Since the plasma pharmacokinetics of a drug can be altered in different patient populations due to a variety of reasons associated specifically with a particular tumor type (e.g., changes in protein binding, metabolism, transporter expression or even intestinal uptake of the drug), dose modifications based on different patient population may be necessary. The intent of the current analysis was to determine whether there is a systematic difference in the disposition of axitinib across populations of patients with different solid tumors. The population pharmacokinetic analysis in this study was based on pooled data, including rich data from healthy volunteers administered a single dose of axitinib and sparse data from patients with NSCLC, thyroid cancer, or metastatic melanoma treated with multiple doses of axitinib. The plasma pharmacokinetics of axitinib was best described using a two-compartment model with first-order absorption and elimination, and population pharmacokinetic parameters were estimated. Diagnostic plots for the final model revealed that both population and individual predictions agreed well with observed values and the CWRESI was evenly distributed, scattered across the range of observations as well as time. The VPC, stratified based on significant covariates identified in the final model, revealed model misspecification at the terminal phase where the observed data (median and 2.5th and 97.5th percentiles) were outside the 95 % prediction interval, based on simulations. The likely reason was the method (i.e., the M1 vs. M3 approach) used in handling BLQ concentrations. Effects of BLQ concentrations on axitinib pharmacokinetic parameter estimates had previously been evaluated using two approaches: M1, where BLQ concentrations were omitted, and M3, which is a likelihood-based approach where BLQ and at or greater than BLQ concentrations were treated as categorical-type and continuous-type data, respectively [24]. M3 method requires the Laplace approximation, and thus, results in substantially longer run times. Since no major discrepancies in pharmacokinetic parameter estimates (CL, in particular) were observed between the two approaches, the M1 method was applied in the current analysis.
This population pharmacokinetic analysis included patient population (with NSCLC, thyroid cancer, or melanoma) as a covariate that was formally tested and determined not to be significant in the model; hence, the final model did not include the patient population as a covariate of interest. With the observed data in this analysis, differences in the disposition of axitinib across the solid-tumor patient populations could not be concluded. Also, comparison of C max and AUCtau predicted based on the previously published final mRCC model and the one developed for NSCLC, thyroid cancer, and metastatic melanoma in the current study did not shown any obvious differences, supporting the notion that tumor type does not significantly impact axitinib plasma exposures. The analysis showed that parameter estimates of k a and F of axitinib administered as crystal polymorph form IV film-coated, immediate-release tablets would be greater when administered after fasting. It should be noted, however, that the food effect was found not to be clinically significant for crystal polymorph form XLI, which is used for the commercial formulation developed subsequently [16]. The model also predicted a strong correlation between gender and CL. Inclusion of gender on axitinib CL decreased IIV from 52.1 % in the base model to 47.9 % in the final model. The effect of gender on CL was not just a reflection of the lower body weight in females, since body weight was not identified as a significant covariate for CL. Body weight, however, was found to impact V c. Inclusion of body weight resulted in the change in the approximate % CV for IIV from 25.5 % in the base model to 16.9 % in the final model. To assess the clinical importance of these two covariates, simulations with the final model were performed using gender and weight to predict axitinib exposures at steady state, which showed overlap in predicted axitinib plasma concentrations for the extreme combinations (i.e., 44-kg female vs. 143-kg male); hence, they were not considered clinically significant (data not shown). The recommendation is that axitinib dose adjustment based on these covariates is not necessary. It should be pointed out that the current approved dosing paradigm for axitinib includes dose titration based on individual patient tolerability [12], which would likely lead to optimization of plasma exposures in patients who have higher or lower than typical values at the staring dose.
The statistically significant covariate effect of body weight on V c found in the current analysis is similar to that found in the previous analyses [19, 20]. On the other hand, a correlation between gender and CL predicted here differs from the previous analysis conducted in patients with mRCC [20]. As indicated earlier, this difference may be associated with gender confounded with age in the dataset used in this analysis (see Fig. 2). The females in the pooled dataset for this analysis were older than the males. Additionally, VPCs stratified by gender were able to predict the observed plasma concentrations for male and female whether they were healthy volunteer or patient population (see Fig. 3b). The number of female and male patients as well as age range was comparable. With the data in hand, the univariate analysis identified age as well as gender as statistically significant. Therefore, the possibility of the effects of these two covariates being confounded by differences between the healthy and patient populations exists, but the available data indicate that it is very unlikely.
The results of covariate testing for axitinib in this study were overall similar to those reported for other tyrosine kinase inhibitors (sunitinib [26] and sorafenib [27]) in that gender and body weight were found to be statistically significant covariates, affecting the respective pharmacokinetic parameters. Unlike in the current analysis, however, the sunitinib pharmacokinetic model additionally predicted a relationship between some tumor types and oral clearance. Because predicted changes in exposures based on these covariates identified as significant were smaller than their respective IIV, it was also concluded that these covariates were not clinically important in their studies. Other covariates need to be investigated in prospective studies. In this regard, it should be noted that the majority of axitinib in plasma is bound to plasma proteins [28] and is metabolized primarily by CYP3A4 and CYP3A5 and, to a lesser extent (<10 %), by CYP1A2, CYP2C19 and uridine diphosphate glucuronosyltransferase (UGT) 1A1 [29]. Genetic polymorphisms in these enzymes have been shown to influence plasma exposures for some drugs [30–32]. However, independent analyses performed using data from healthy volunteers indicated that axitinib disposition did not seem to be significantly affected by the common variants tested such as CYP3A4*1, CYP3A5*3, UGT1A1*28, or CYP2C19*17 [19, 33].
In conclusion, the current analysis characterized the pharmacokinetics of axitinib for the first time in NSCLC, thyroid cancer, or melanoma patients. Axitinib disposition was adequately described using a two-compartment model with first-order absorption and elimination. Tumor type did not account for the variability of axitinib pharmacokinetics among individuals. On the other hand, gender on CL and body weight on V c were identified as statistically significant covariates. However, based on predicted changes, neither covariate was considered to be clinically relevant, minimizing the necessity for dose adjustment on the basis of gender or body weight. Therefore, we did not find any clinically meaningful covariates, i.e., those that significantly drop the % CV, among those tested in the current analysis. The comparison between axitinib pharmacokinetics established for NSCLC, thyroid cancer, and melanoma with the results of the previous analysis in mRCC indicated no evidence of any major difference in axitinib pharmacokinetics across different tumor types; hence, the same dosing of axitinib may be used in the treatment of patients with different tumor types.
References
Hu-Lowe DD, Zou HY, Grazzini ML, Hallin ME, Wickman GR, Amundson K, Chen JH, Rewolinski DA, Yamazaki S, Wu EY, McTigue MA, Murray BW, Kania RS, O’Connor P, Shalinsky DR, Bender SL (2008) Nonclinical antiangiogenesis and antitumor activities of axitinib (AG-013736), an oral, potent, and selective inhibitor of vascular endothelial growth factor receptor tyrosine kinases 1, 2, 3. Clin Cancer Res 14:7272–7283
Choueiri TK (2008) Axitinib, a novel anti-angiogenic drug with promising activity in various solid tumors. Curr Opin Investig Drugs 9:658–671
Kelly RJ, Rixe O (2009) Axitinib–a selective inhibitor of the vascular endothelial growth factor (VEGF) receptor. Target Oncol 4:297–305
Rixe O, Bukowski RM, Michaelson MD, Wilding G, Hudes GR, Bolte O, Motzer RJ, Bycott P, Liau KF, Freddo J, Trask PC, Kim S, Rini BI (2007) Axitinib treatment in patients with cytokine-refractory metastatic renal-cell cancer: a phase II study. Lancet Oncol 8:975–984
Rini BI, Wilding G, Hudes G, Stadler WM, Kim S, Tarazi J, Rosbrook B, Trask PC, Wood L, Dutcher JP (2009) Phase II study of axitinib in sorafenib-refractory metastatic renal cell carcinoma. J Clin Oncol 27:4462–4468
Cohen EE, Rosen LS, Vokes EE, Kies MS, Forastiere AA, Worden FP, Kane MA, Sherman E, Kim S, Bycott P, Tortorici M, Shalinsky DR, Liau KF, Cohen RB (2008) Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. J Clin Oncol 26:4708–4713
Schiller JH, Larson T, Ou SH, Limentani S, Sandler A, Vokes E, Kim S, Liau K, Bycott P, Olszanski AJ, von Pawel J (2009) Efficacy and safety of axitinib in patients with advanced non-small-cell lung cancer: results from a phase II study. J Clin Oncol 27:3836–3841
Fruehauf JP, Lutzky J, McDermott DF, Brown CK, Meric JB, Rosbrook B, Shalinsky DR, Liau KF, Niethammer AG, Kim S, Rixe O (2011) Multicenter, phase II study of axitinib, a selective second-generation inhibitor of vascular endothelial growth factor receptors 1, 2, 3, in patients with metastatic melanoma. Clin Cancer Res 17:7462–7469
Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, Michaelson MD, Gorbunova VA, Gore ME, Rusakov IG, Negrier S, Ou Y-C, Castellano D, Lim HY, Uemura H, Tarazi J, Cella D, Chen C, Rosbrook B, Kim S, Motzer RJ (2011) Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet 378:1931–1939
Boxenbaum H, Battle M (1995) Effective half-life in clinical pharmacology. J Clin Pharmacol 35:763–766
Rugo HS, Herbst RS, Liu G, Park JW, Kies MS, Steinfeldt HM, Pithavala YK, Reich SD, Freddo JL, Wilding G (2005) Phase I trial of the oral antiangiogenesis agent AG-013736 in patients with advanced solid tumors: pharmacokinetic and clinical results. J Clin Oncol 23:5474–5483
INLYTA (axitinib) prescrining information. http://labeling.pfizer.com/ShowLabeling.aspx?id=759. Accessed July 2, 2014
Pithavala YK, Tortorici M, Toh M, Garrett M, Hee B, Kuruganti U, Ni G, Klamerus KJ (2010) Effect of rifampin on the pharmacokinetics of Axitinib (AG-013736) in Japanese and Caucasian healthy volunteers. Cancer Chemother Pharmacol 65:563–570
Chen Y, Jiang J, Zhang J, Tortorici MA, Pithavala YK, Lu L, Ni G, Hu P (2011) A Phase I study to evaluate the pharmacokinetics of axitinib (AG-13736) in healthy Chinese volunteers. Int J Clin Pharmacol Ther 49:679–687
Pithavala YK, Tong W, Mount J, Rahavendran SV, Garrett M, Hee B, Selaru P, Sarapa N, Klamerus KJ (2012) Effect of ketoconazole on the pharmacokinetics of axitinib in healthy volunteers. Invest New Drugs 30:273–281
Pithavala YK, Chen Y, Toh M, Selaru P, LaBadie RR, Garrett M, Hee B, Mount J, Ni G, Klamerus KJ, Tortorici MA (2012) Evaluation of the effect of food on the pharmacokinetics of axitinib in healthy volunteers. Cancer Chemother Pharmacol 70:103–112
Larson RA, Druker BJ, Guilhot F, O’Brien SG, Riviere GJ, Krahnke T, Gathmann I, Wang Y (2008) Imatinib pharmacokinetics and its correlation with response and safety in chronic-phase chronic myeloid leukemia: a subanalysis of the IRIS study. Blood 111:4022–4028
Houk BE, Bello CL, Poland B, Rosen LS, Demetri GD, Motzer RJ (2010) Relationship between exposure to sunitinib and efficacy and tolerability endpoints in patients with cancer: results of a pharmacokinetic/pharmacodynamic meta-analysis. Cancer Chemother Pharmacol 66:357–371
Garrett M, Poland B, Brennan M, Hee B, Pithavala YK, Amantea MA (2014) Population pharmacokinetic analysis of axitinib in healthy volunteers. Br J Clin Pharmacol 77:480–492
Rini BI, Garrett M, Poland B, Dutcher JP, Rixe O, Wilding G, Stadler WM, Pithavala YK, Kim S, Tarazi J, Motzer RJ (2013) Axitinib in metastatic renal cell carcinoma: results of a pharmacokinetic and pharmacodynamic analysis. J Clin Pharmacol 53:491–504
Lindbom L, Pihlgren P, Jonsson EN (2005) PsN-Toolkit–a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 79:241–257
Hooker AC, Staatz CE, Karlsson MO (2007) Conditional weighted residuals (CWRES): a model diagnostic for the FOCE method. Pharm Res 24:2187–2197
Savic RM, Karlsson MO (2009) Importance of shrinkage in empirical bayes estimates for diagnostics: problems and solutions. AAPS J 11:558–569
Garrett M, Amantea MA, Pithavala YK, Ruiz A (2010) Evaluation of the impact of omitting drug concentration data below the lower limit of quantification (LLOQ) on the pharmacokinetics of axitinib (AG-013736), an anti-angiogenic agent. Clin Pharmacol Thera 87(suppl 1; abstr PIII-33):S78–S79
Karlsson MO, Savic RM (2007) Diagnosing model diagnostics. Clin Pharmacol Ther 82:17–20
Houk BE, Bello CL, Kang D, Amantea M (2009) A population pharmacokinetic meta-analysis of sunitinib malate (SU11248) and its primary metabolite (SU12662) in healthy volunteers and oncology patients. Clin Cancer Res 15:2497–2506
Jain L, Woo S, Gardner ER, Dahut WL, Kohn EC, Kummar S, Mould DR, Giaccone G, Yarchoan R, Venitz J, Figg WD (2011) Population pharmacokinetic analysis of sorafenib in patients with solid tumours. Br J Clin Pharmacol 72:294–305
Tortorici MA, Toh M, Rahavendran SV, LaBadie RR, Alvey CW, Marbury T, Fuentes E, Green M, Ni G, Hee B, Pithavala YK (2011) Influence of mild and moderate hepatic impairment on axitinib pharmacokinetics. Invest New Drugs 29:1370–1380
Smith BJ, Pithavala Y, Bu H, Kang P, Hee B, Deese AJ, Pool WF, Klamerus KJ, Wu EY, Dalvie DK (2014) Pharmacokinetics, metabolism, and excretion of [14C]axitinib, a vascular endothelial growth factor receptor tyrosine kinase inhibitor, in humans. Drug Metab Dispos 42:918–931
Lamba JK, Lin YS, Schuetz EG, Thummel KE (2002) Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev 54:1271–1294
Zhao W, Elie V, Roussey G, Brochard K, Niaudet P, Leroy V, Loirat C, Cochat P, Cloarec S, Andre JL, Garaix F, Bensman A, Fakhoury M, Jacqz-Aigrain E (2009) Population pharmacokinetics and pharmacogenetics of tacrolimus in de novo pediatric kidney transplant recipients. Clin Pharmacol Ther 86:609–618
Han JY, Lim HS, Shin ES, Yoo YK, Park YH, Lee JE, Jang IJ, Lee DH, Lee JS (2006) Comprehensive analysis of UGT1A polymorphisms predictive for pharmacokinetics and treatment outcome in patients with non-small-cell lung cancer treated with irinotecan and cisplatin. J Clin Oncol 24:2237–2244
Brennan M, Williams JA, Chen Y, Tortorici M, Pithavala Y, Liu YC (2012) Meta-analysis of contribution of genetic polymorphisms in drug-metabolizing enzymes or transporters to axitinib pharmacokinetics. Eur J Clin Pharmacol 68:645–655
Acknowledgments
This study was sponsored by Pfizer Inc. Medical writing support was provided by Mariko Nagashima, PhD, at Engage Scientific Solutions (Southport, CT, USA) and was funded by Pfizer Inc.
Conflict of interest
The current study and trials included in the analyses were funded by Pfizer Inc. Yazdi K. Pithavala and Ana Ruiz-Garcia are employees of and own stock in Pfizer Inc. Michael A. Tortorici, May Garrett, and Sinil Kim were employed at Pfizer Inc during the time of this study and development of the manuscript. Michael A. Tortorici is currently an employee of CSL Behring Biotherapies for Life™ and owns stock in Pfizer Inc. May Garrett is currently a contracted employee of and owns stock in Pfizer Inc. Sinil Kim is currently an employee of Mirna Therapeutics and owns stock in Pfizer Inc and Mirna Therapeutics Inc. Ezra E.W. Cohen has nothing to disclose. John P. Fruehauf received research funding from Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Michael A. Tortorici, May Garrett, and Sinil Kim were employed at Pfizer Inc during the time of this study and development of the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tortorici, M.A., Cohen, E.E.W., Pithavala, Y.K. et al. Pharmacokinetics of single-agent axitinib across multiple solid tumor types. Cancer Chemother Pharmacol 74, 1279–1289 (2014). https://doi.org/10.1007/s00280-014-2606-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2606-6