Abstract
Purpose
The aim of this study was to characterize trastuzumab population pharmacokinetics (PKs) in patients with human epidermal growth factor receptor 2-positive advanced gastric or gastroesophageal junction cancer and the relationship of trastuzumab PK with patient response.
Methods
A nonlinear mixed effects PK model was built using data from the ToGA study. Patients were randomized to intravenous trastuzumab plus chemotherapy or chemotherapy alone. The influence of demographic, laboratory, and disease characteristics on PK parameters was assessed. An exploratory exposure–response analysis compared various PK parameters at steady state with best overall tumor response and overall survival (OS).
Results
Trastuzumab PK was best described by a two-compartment model with parallel linear and nonlinear (Michaelis–Menten) elimination from the central compartment. Total clearance (and half-life) of trastuzumab was concentration-dependent. Body weight, prior gastrectomy, and serum albumin had the greatest influence on trastuzumab PK; increasing weight and decreasing albumin levels were associated with increased clearance, while prior gastrectomy correlated with decreased clearance. Median values for AUC, C max, and C min were lower in patients with progressive disease (PD) than other response categories, although the 1.5 interquartile ranges overlapped. Patients with the lowest C min had the highest PD rate and a shorter OS.
Conclusions
In the advanced gastric cancer population, trastuzumab PK was best described by a two-compartment model with parallel linear and nonlinear elimination. Predicted PK exposure was lower than previously reported for breast cancer. Patients with the lowest C min had a shorter OS and the highest PD rate, but a distinct correlation was not observed for tumor response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human epidermal growth factor receptor 2 (HER2) is a transmembrane tyrosine kinase receptor encoded by the HER2 gene on chromosome 17q21 [1, 2]. Activation of members of the HER family of receptors initiates an intracellular transduction cascade involved in cell proliferation, apoptosis, adhesion, migration, and differentiation [3]. In the 1980s, researchers discovered that overexpression of the HER2 receptor occurred in human breast cancers, conferring a negative impact on prognosis, with shorter overall survival (OS) and time to relapse [4]. This led to the development of breast cancer therapies specifically targeted to HER2. Since then, high-level amplification of the HER2 gene and overexpression of the HER2 receptor have been identified in several solid tumor types, including gastric cancer [3]. Between 10 and 24 % of gastric/gastroesophageal cancers overexpress HER2 [3, 5, 6].
In 2010, trastuzumab (Herceptin; Genentech Inc., South San Francisco, CA), a humanized monoclonal antibody (mAb) targeting HER2, was approved in Europe and the USA for the treatment of HER2-positive metastatic adenocarcinoma of the stomach or gastroesophageal junction (GEJ), based on data from the large-scale, randomized trastuzumab for gastric cancer (ToGA) trial (NCT01041404) [7]. This study showed that adding trastuzumab to chemotherapy with a fluoropyrimidine (5-fluorouracil or capecitabine) and cisplatin resulted in a significant 26 % improvement in OS compared with chemotherapy alone (P = 0.0046) [7]. Serum samples were collected from patients in the experimental arm of the ToGA study to investigate the pharmacokinetics (PK) of trastuzumab in this patient population, and the relationship between trastuzumab exposure and tumor response. This paper describes the population modeling approach used to characterize the PK of trastuzumab in the ToGA study population, to estimate the between-subject variability (BSV) and to quantify the effects of demographic, laboratory, and disease characteristics on the PK of trastuzumab. Additionally, exploratory analyses examining the relationship between trastuzumab exposure and best overall response and survival were performed.
Materials and methods
Patients and study design
The ToGA study has been described previously [7]. Briefly, this was an international, phase III, randomized, open-label trial in patients with HER2-positive inoperable, locally advanced, recurrent, or metastatic adenocarcinoma of the stomach or GEJ. HER2-positive status was defined as 3+ on immunohistochemistry (IHC) (HercepTest; Dako, Denmark) or a HER2:CEP17 ratio of ≥2 on fluorescence in situ hybridization (HER2 FISH pharmDx; Dako, Denmark). Patients were randomized 1:1 to trastuzumab plus chemotherapy or chemotherapy alone. The chemotherapy regimen consisted of cisplatin plus capecitabine or fluorouracil given in 3-week cycles for up to six cycles. Trastuzumab was administered by intravenous (IV) infusion at a dose of 8 mg/kg over 90 min on day 1 of the first cycle and then at 6 mg/kg over 30 min, if tolerated, every 3 weeks until disease progression, unacceptable toxicity, or withdrawal of consent. The study was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written informed consent, and the protocol was approved by independent ethics committees [7].
PK sampling and bioanalytic method
Eight blood samples were collected from each patient in the trastuzumab arm of the study at the following times: before the first dose of trastuzumab, at the end of the infusion, and on days 8 and 15 of cycle 1; before the trastuzumab infusion in cycle 2; before and at the end of the trastuzumab infusion in cycle 4; and before the trastuzumab infusion in cycle 6. The PK population consisted of all patients who had at least one measurement of trastuzumab serum concentration associated with documented trastuzumab dosing history. Within the PK population, exposure–response relationships were analyzed in two groups of patients: those in whom a best overall response was reported (population 1), those in whom a best overall response was reported, and the time course of tumor size was available (population 2; see the following section).
Serum concentrations of trastuzumab were determined by enzyme-linked immunosorbent assay. The stationary phase of this assay was a recombinant version of the extracellular domain of the p185HER2 receptor (shed antigen). The lower limit of quantification of the assay was 156 ng/mL.
Population PK base model development
Population PK estimation and model evaluation were undertaken using NONMEM software version 7.2.0 (GloboMax; Hanover, MD). The model was developed using first-order conditional estimation with interaction [8].
To explore the suitability of a nonlinear structural PK model for trastuzumab in these gastric cancer patients, two models were evaluated and compared: a two-compartment disposition PK model with parallel first-order and Michaelis–Menten elimination and a two-compartment disposition model with first-order elimination process. The following PK parameters were estimated during model development: linear clearance (CL), volume of distribution of the central compartment (V1), intercompartmental clearance (Q), and volume of distribution of the peripheral compartment (V2); and for nonlinear clearance, maximum elimination rate (VM), and the Michaelis–Menten constant (KM). Knowing that measures of body size are the covariates most commonly identified as influencing the PK of monoclonal antibodies [9, 10], body weight [WT; kg] dependencies were investigated on clearances (CL and Q) and volumes (V1 and V2) of the best structural model, using either fixed (a power of 0.75 for the clearances and a power of 1 for the volumes) or estimated allometric scaling. In addition, as the target antigen density (indirectly represented by the tumor burden) may affect non-specific and target-mediated clearance [9, 10] and volumes, effects of the two main covariates characterizing the tumor burden, (i.e., lesion sizes at baseline [BTMZ, mm] documented as the sum of the measurements of the longest diameters of the individual target lesions as per RECIST 1.0 and occurrence of prior gastrectomy [GOMY]), were investigated on CL, VM, KM, V1 and V2 of the best structural model. For the patients with non-measurable lesions (representing 9 % of the population), the tumor size of the individual target lesions was imputed to half the size of the smallest lesion that can be detected by spiral CT scan (i.e., 10 mm as per RECIST 1.0 requirements). The investigation of other disease-related covariate dependencies of model parameters was left to the covariate model development.
The model selection was based on various goodness-of-fit indicators, including visual inspection of diagnostic plots (e.g., observed versus predicted concentration, conditional weighted residual versus predicted concentration or time, histograms of individual random effects), plausibility of the parameter estimates, precision of the parameter estimates, the minimum objective function value (the objective function was equal to minus twice the maximum log likelihood), and the number of estimated parameters. All parameter estimates were reported with their 95 % confidence intervals.
All BSV on the PK parameters were described by a log-normal parameter distribution. To account for the difference between model-predicted and actual trastuzumab concentrations, various residual error models were tested.
Covariate model development
Baseline demographic covariates (sex [SEX], age [AGE], race [RACE; Asian/non-Asian], ethnicity [ETHN; Japanese versus non-Japanese]), baseline laboratory covariates (alkaline phosphatase [ALK; U/L], serum albumin [ALB; g/L], total bilirubin [BIL; μmol/L], alanine aminotransferase [ALT; U/L], and aspartate aminotransferase [AST; U/L]), disease-related covariates (HER2 status [HER; IHC 0 to 2+/IHC 3+], Eastern Cooperative Oncology Group [ECOG] performance status, primary tumor site [PRIM], extent of disease at study entry [EXT; metastatic/locally advanced], measurable disease [MEAS], number of metastatic lesions [NLES], number of metastatic sites [MSIT], type of gastric cancer [TARG], presence of visceral metastases [MVIS]), and chemotherapy regimen (CHEM; 5-fluorouracil plus cisplatin/capecitabine plus cisplatin) were included in the covariate analysis. Among the disease-related covariates, in addition to GOMY and BTMZ, which were investigated during the base model development, NLES, MSIT, and MVIS were linked to tumor burden. The categories Asian/non-Asian race and Japanese versus non-Japanese ethnicity were included as covariates because of the differences in incidence, mortality, and survival rates between Western Europe/North America and East Asia [11–13].
The full model with the covariate effects was built using the stepwise inclusion at a significance level of P < 0.005, which corresponds to the difference in objective function of 7.88 (chi-squared distribution for 1 degree of freedom). The significance of covariate effects in the full model was then retested by the backward deletion. The significance level for retaining a covariate in the final model was P < 0.001, which corresponded to the difference in objective function exceeding 10.83 for 1 degree of freedom.
Model evaluation
The PK model was qualified by a visual predictive check. The simulated PK parameters were randomly sampled from their respective estimated distributions, and serum trastuzumab concentrations were calculated based on the sampled PK parameter values and residual variability. A thousand simulations were performed, and the 90 % confidence intervals (i.e., 5th and 95th percentiles) computed from the simulated PK profiles were derived for each statistic (i.e., the median and the 5th and the 95th percentiles) and compared with the median and the 5th and the 95th percentiles of the observed PK profiles. The total number of points found to be outside the 90 % prediction interval was counted.
Exposure–response analyses
Exploratory analysis of the link between trastuzumab exposure and best overall response (defined as the best response recorded from the start of trial treatment until disease progression/recurrence or death) was undertaken. The link between tumor response, i.e., best overall response and time course of relative change in tumor size (which was calculated as 100 × [tumor size at time t]/[tumor size at time 0]), and trastuzumab exposure was evaluated by comparing the response between categories of trastuzumab exposure using the trough minimum concentration (C min) at steady state. Patients were categorized according to quartiles of the trastuzumab C min (≤25th percentile, >25th percentile to ≤50th percentile, >50th percentile to ≤75th percentile, and >75th percentile). Additionally, post hoc exploratory analysis of OS by trastuzumab exposure (C min at steady state by quartiles) was estimated via the Kaplan–Meier method for patients in the trastuzumab plus chemotherapy arm whose trastuzumab concentrations were available. OS was defined as the time between randomization date and date of death due to any cause. Data for patients who were known not to have died or progressed at the time of the analysis were censored at the date they were last known to be alive or the clinical data cutoff date (January 7, 2010), whichever occurred first.
Results
Base PK model
The population PK model was developed using 1,419 trastuzumab serum concentrations collected from 266 patients from the trastuzumab arm of the ToGA study. Most of the patients (77.8 %) were male, and 96.2 % had metastatic disease at study entry. The median sum of the longest diameters of target tumors at baseline was 82 mm. Patients’ ages ranged from 23 to 83 years (median, 61 years), and patients’ body weight ranged from 35 to 111 kg (median, 62 kg). Other baseline and demographic information is shown in Supplementary Table S1. Trastuzumab PK was best described by a two-compartment disposition model with parallel first-order (linear) and Michaelis–Menten (non-linear) elimination. The model with estimated body weight effect on CL and V1 was superior to the model with fixed allometric scaling on both clearances and volumes. In addition, clearance was found to be affected by the occurrence of prior gastrectomy and V2 was affected by the tumor size at baseline. BSV was incorporated on CL, V1, and V2; the data did not support estimation of BSV for Q, VM, or KM. All BSV components were found to be significantly correlated with the strongest correlations being between the BSV on CL and V1 with a correlation coefficient of 0.63 and between the BSV on V1 and V2 with a correlation coefficient of 0.51. The coefficient of the correlation between the BSV on CL and V2 was very small (−0.07). RV was best described by a proportional error model with the magnitude of this error varying between individuals. The diagnostic plots for the base model indicated that observed and predicted data were in good agreement with a random distribution around the identity lines, indicating the absence of systematic bias and the adequacy of the model. Additionally, conditional weighted residuals also showed random distribution around zero and no specific pattern.
Final PK model
During the building of the covariate model, the impact of the covariates was tested on CL, V1, and V2. After the incorporation of the additional covariates, the effect of tumor size on V2 became smaller and poorly estimated with a RSE greater than 50 %, and it did not remain in the final model when the effect of alkaline phosphatase was added. The graph of target tumor size at baseline versus alkaline phosphatase showed some level of correlation between the two covariates. The final PK model included the effects of body weight [WT], prior gastrectomy [GOMY], and baseline albumin levels [ALB] on CL, the effect of body weight [WT] on V1, and the effect of ethnicity [ETHN] and baseline alkaline phosphatase levels [ALK] on V2. The covariate models in the final model were:
The final population PK model estimated a typical CL of 0.23 L/day for linear elimination, V1 of 3.63 L, Q of 0.37 L/day, and V2 of 3.74 L, as well as a typical VM of 5.76 mg/day and a KM of 3.7 μg/mL for nonlinear elimination. All of the population parameters were well estimated with relative standard error below 43 %. The parameter estimates with relative standard errors in the final model are shown in Table 1.
Dependencies of the PK model parameters on the covariates investigated in this analysis were captured by the final model, as evidenced by the absence of trends for the random effects on covariates (data on file). Figure 1 shows the relationship between the statistically significant covariates in the final model and individual PK parameters. The CL of trastuzumab is increased in patients with low levels of albumin (power of −0.7) and is decreased in those with a prior gastrectomy. Within the range of baseline albumin levels (24–75 g/L), trastuzumab CL could be increased by 39.8 % or reduced by 38.5 %, respectively, from the typical value of CL calculated for an albumin level of 38 g/L. Prior gastrectomy reduced CL by 21.6 % compared with that in a patient without gastrectomy. The power coefficients of body weight effect on CL and V1 were 1 and 0.65, respectively, indicating a steep increase of those parameters with body weight. Patients with the lowest body weight of 35.3 kg had 45.3 % lower trastuzumab CL than the typical value of CL calculated for a patient weighing 62 kg, while patients with the highest body weight of 111 kg had an 86.5 % increase in CL versus typical CL. V1 showed a reduction of –30.6 % versus typical at the lowest body weight and an increase of 45.8 % versus typical at the highest body weight. V2 was affected by both ethnicity and baseline alkaline phosphatase levels. Patients of Japanese ethnicity had a V2 that was 33.8 % lower than that of non-Japanese patients. Increasing levels of alkaline phosphatase increase the V2 (power of 0.38); within the range of baseline alkaline phosphatase levels of between 26 and 834 U/L, trastuzumab V2 could be reduced by 39.8 % or increased by 128 %, respectively, from the typical value of V2 calculated for an alkaline phosphatase level of 98 U/L.
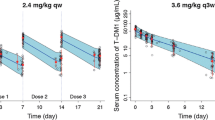
The goodness-of-fit plots presented in Fig. 2 (Panels A–D) showed good agreement between observed and predicted data. Similar agreement was seen when modeled and observed data were compared using the logarithmic scale (data not shown). The plots of conditional weighted residuals versus time or versus population prediction showed a random distribution of data points around the zero line, with the majority of data within two standard deviations (between −2 and +2). The distribution of the conditional weighted residuals did not indicate any major deviation from normality. The results of the visual predictive check (Fig. 2, panel E) indicated that the model correctly captured both the central tendency and the BSV of trastuzumab PK. The shrinkage for CL, V1, and V2 was 11, 18, and 29 %, respectively, indicating that the sampling scheme was informative to derive individual PK parameter estimates.
Goodness-of-fit plot. a Observed (DV) versus population-predicted trastuzumab serum concentrations (PRED); b Observed (DV) versus individual population-predicted trastuzumab serum concentrations (IPRED); c Conditional weighted residual (CWRES) versus predicted trastuzumab serum concentrations (PRED); d Conditional weighted residual (CWRES) versus time; e Visual predictive check of the observed trastuzumab concentration (DV) and the simulated concentrations of trastuzumab from the model, using 1,000 simulations. The solid line represents the median of the observed trastuzumab concentrations, and the beige shaded areas indicate 90 % confidence intervals (i.e., 5th and 95th percentiles) computed from the simulations around the predicted median. The dotted line indicates the 5th and 95th percentiles of the observed trastuzumab concentrations, and the green-shaded areas are the 90 % confidence intervals for the observed concentrations around the 5th and 95th predicted percentiles
Dependence of clearance on trastuzumab serum concentrations
The population PK model development demonstrated that trastuzumab is eliminated by two pathways, linear and nonlinear. Consequently, the total clearance of trastuzumab is dependent on trastuzumab serum concentrations (see Supplementary Fig. S1). Both CL and nonlinear clearance contribute equally to total trastuzumab clearance for concentrations of ~25 μg/mL. At very low concentrations (<10 μg/mL), nonlinear clearance is approximately sevenfold higher than CL, accounting for almost all of the total trastuzumab clearance. For trastuzumab concentrations >75 μg/mL, CL predominates, and nonlinear clearance represents <30 % of total clearance. Because the clearance of trastuzumab is concentration-dependent, so is the half-life, which can only be calculated at a given serum concentration. During a given dosing interval at steady state, the effective half-life [14] of trastuzumab varied between 9.6 and 23 days, reflective of the changing concentration following the dose. At high concentrations (when total clearance is dominated by CL), a terminal half-life of ~26 days was calculated using the population PK model.
The combined CL and nonlinear clearance of trastuzumab prevents the direct derivation of time to steady state from the primary PK parameters. However, time to steady state could be estimated by simulating trastuzumab concentrations over 20 cycles of treatment, administered as an IV infusion every 3 weeks at a dose of 8 mg/kg (i.e., first [loading dose]) followed by 19 cycles at 6 mg/kg, with 100 replicates of the patient population used to develop the model. The simulated time course of trastuzumab following 15 cycles is shown in Supplementary Figure S2. The time to reach 95 % of steady state for area under the concentration–time curve (AUC) was 126 days (seven cycles), for maximum concentration (C max) was 84 days (five cycles), and for C min was 168 days (nine cycles). The predicted mean steady-state values were AUC of 1,269 mg day/L; C max of 135 mg/L; C min of 31.1 mg/L, using these simulations. The predicted steady-state values were very similar to the estimated mean steady-state values for these parameters using NONMEM for the patients in the PK data set, which were AUC of 1,240 mg day/L, C max of 134 mg/L, and C min of 29.4 mg/L.
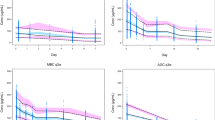
Exposure–response relationship: objective responses
The median and 1.5 interquartile ranges for AUC, C max, and C min at different cycles or at steady state were similar among patients with objective tumor response (complete response [CR] or partial response [PR]) or stable disease (SD), but lower in patients with progressive disease (PD; see Fig. 3 for median AUC, C max, and C min at steady state). Although median values for AUC, C max, and C min showed a visual trend to be lower in PD patients than other response categories, there was a large overlap in the exposure range between the response categories. The same conclusions were drawn when comparing the mean and the 90 % prediction intervals (data on file).
When tumor response was evaluated by quartiles of C min at steady state, the percentage of patients with PD was highest in the quartile with the lowest C min and the percentage with CR was highest in the quartile with the highest C min (Table 2). Objective tumor response assessed by CR plus PR in the lowest quartile of exposure was also slightly lower than that for the upper three quartiles of exposure: 46 % in the lowest quartile and 55–64 % in the upper three quartiles. Similar findings were observed when assessed by non-PD (CR + PR + SD), where non-PD is observed in 69 % of the lowest quartile of C min compared with 91–92 % in the upper three quartiles of exposure. However, when the individual time course of tumor size by category of C min at steady state was plotted, there was no obvious difference in the time course profile of the relative change in tumor size and the categories of C min (Supplementary Fig. S3). Similar findings were seen when the analyses were repeated for different categories of C max or AUC at steady state (data not shown).
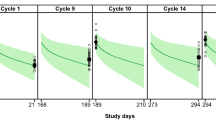
Exposure–response relationship: overall survival
It was observed from the results of the exploratory analysis of OS by C min at steady state that patients with low C min (defined as ≤25th percentile of C min) appeared to have shorter median OS duration compared with other quartiles (Fig. 4). To explore whether other factors could contribute to this observed shorter duration of OS in the lowest C min percentile group, further analyses of baseline patient characteristics by C min quartile were performed. Compared with other quartiles, more patients in the lowest C min quartile subgroup had Eastern Cooperative Oncology Group performance status (ECOG PS) of 2 (21 vs 2–11 %), low baseline serum albumin (median of 35 vs 38–40 g/L), and greater tumor burden, as evidenced by visceral (lung or liver) metastases (63 vs 52–56 %), higher number of metastatic lesions (>4; 64 vs 36–63 %), higher number of metastatic sites (>2; 63 vs 35–46 %), and no prior gastrectomy (90 vs 59–83 %) (see Supplementary Table S2). When investigating the effects of those disease-related covariates on the PK of trastuzumab, only history of gastrectomy was found to be statistically significant; thus, it is unclear whether the lower OS is due to low drug concentration or to disease burden.
Duration of survival by trough trastuzumab concentrations in cycle 1: patients in trastuzumab + chemotherapy arm with trough trastuzumab concentrations in cycle 1. Kaplan–Meier estimates are shown. OS was defined as the time between randomization date and date of death due to any cause. Data for patients who were known not to have died at the time of the analysis were be censored at the date they were last known to be alive or the clinical data cutoff date (January 7, 2010), whichever occurred first
Discussion
This is the first report on the population PK profile of trastuzumab in patients with HER2-positive gastric cancer, which includes the analysis of laboratory and patient covariates influencing trastuzumab PKs. In addition, we report the PK exposure–response relationship for objective tumor response and OS. These data are unique, both complementing and extending the previous publication by the US Food and Drug Administration (FDA), which provided a case–control analysis of the ToGA study using the population PK model reported here [15].
The model that best described trastuzumab serum concentration was a two-compartment model, incorporating parallel linear and nonlinear (Michaelis–Menten) pathways for elimination from the central compartment. The nonlinear elimination pathway for trastuzumab can be attributed to its interaction with its target, the HER2 receptor, which is a membrane-associated internalizing antigen. When the mAb binds to the receptor, the antibody–antigen complex is internalized and degraded within the cell [16]. This elimination pathway is the main route of elimination of the mAb until the target is saturated. Once saturation is reached, the mAb clearance is then mediated through catabolism by the reticuloendothelial system. This is a linear process, slower than the target-dependent elimination pathway. Similar parallel elimination pathways have been reported for other mAbs targeting different membrane-associated internalizing antibodies, such as cetuximab and panitumumab, which target the epidermal growth factor receptor [16, 17]. As described by this model, trastuzumab PK exposure in advanced gastric cancer was lower than previously reported for patients with metastatic breast cancer (MBC) receiving the same dosing regimen; median values for AUC, C max, and C min at steady state were approximately 30–40 % lower in the patients with gastric cancer [18]. The reasons for these differences are unknown and are the focus of ongoing investigations.
In patients with gastric cancer, the contribution of the nonlinear pathway to the total clearance of trastuzumab was equivalent to the contribution of the linear pathway when the serum level of trastuzumab was approximately 25 μg/mL (Supplementary Fig. S1). At trastuzumab serum concentrations >75 μg/mL, the nonlinear pathway becomes progressively saturated, and linear CL dominates. However, the nonlinear pathway is not continuously saturated during the every 3-week dosing schedule used in the ToGA study, resulting in a change in total trastuzumab clearance between infusions. At steady state, between successive doses, the total clearance of trastuzumab increases by ~48 % as the concentrations decline (see Supplementary Fig. S4). At high trastuzumab concentrations, where total clearance is determined by the linear component, a terminal half-life of approximately 26 days was derived from the population PK model. This is similar to the terminal half-life of 28.5 days estimated in a population PK model of trastuzumab in patients with MBC [19] and to the terminal half-life of the endogenous immunoglobulin G1 component from which trastuzumab is derived (23 days) [20]. The nonlinear elimination pathway also contributes to the variable time to steady state of different PK parameters. For C max, 95 % of steady state is reached after cycle 5, whereas it is reached after cycle 7 and cycle 9 for AUC and C min, respectively.
As for many therapeutic monoclonal antibodies [10], body weight was found to have a significant effect on the PK of trastuzumab and among the covariates tested, it was the one with the greatest effect on the PK of trastuzumab. When compared with the value of CL in a patient weighing 62 kg, the linear CL decreased 45 % for patients with the lowest body weight (i.e., 35 kg) and increased by 87 % for those with the highest weight (i.e., 111 kg). Similarly, weight positively correlated with V1, leading to a deviation from typical of −31 % for patients with the lowest weight and +46 % for those with the highest weight.
The linear CL of trastuzumab is believed to result from the action of reticuloendothelial cells [16], which are widely distributed throughout the body. Therefore, it is not surprising that body size influenced CL and V1. In an analysis of the population PK of trastuzumab in patients with MBC, body weight was also significantly associated with V1 but not with clearance [19]; the reasons for this difference are unknown. In gastric cancer patients, the CL of trastuzumab was also influenced by prior gastrectomy (CL was 22 % lower in patients who had undergone gastrectomy) and serum albumin levels (CL increased with decreasing albumin levels). Gastrectomy may correlate with tumor mass and indirectly to the target antigen density, since surgery reduces tumor mass and may result in higher systemic exposure to trastuzumab.
Hypoalbuminemia is a marker of malnutrition and cachexia and is generally a prognostic factor in cancer patients [21]. As hypoalbuminemia typically reflects low systemic levels of protein, this may be related in affected patients to an elevated protein (including Ig) catabolism, which would explain why the clearance of trastuzumab was increased in these patients; however, this assertion is highly speculative. Ethnicity (Japanese versus non-Japanese) and baseline levels of alkaline phosphatase had a statistically significant influence on V2 in our study. Clinically elevated alkaline phosphatase levels in an oncology patient can come from two sources: (1) from hepatobiliary disease, such as liver metastasis and (2) from bone metastasis. In our population of gastric cancer patients, liver metastasis is much more common than bone metastasis. It is therefore possible that high alkaline phosphatase levels may serve as a marker of tumor burden in place of tumor size at baseline, especially when 9 % of the population had tumors that were non-detectable in size, or where clinical symptomatology may not have warranted a scan of the liver. However, the clinical impact of ethnicity, history of gastrectomy, serum albumin, or alkaline phosphatase levels on trastuzumab exposure was minimal, i.e., there was <20 % difference in exposure between categories of dichotomous variables and between the lowest and highest quartile of continuous variables. Therefore, none of these covariates exert enough of an influence on trastuzumab PK to require a dose adjustment.
The post hoc exploratory exposure–response analyses show that the median AUC, C max, and C min of trastuzumab at steady state are lower in patients with PD than in those with SD or who achieved an objective response, but the overlapping 1.5 interquartile ranges do not suggest a distinct correlation between trastuzumab exposure and tumor response. The analysis might suggest that patients with the lowest trastuzumab exposure, as indicated by C min at steady state, derived a slightly lower benefit from trastuzumab in terms of objective tumor response; however, the overall impact was reflected in a small difference in the percentage of patients with response (CR, PR), which was observed in 46 % of patients in the lowest quartile of exposure versus 55–64 % in the three highest quartiles of exposure. As the analyses of the relative change in tumor size over time by quartiles of exposure did not show obvious differences, any interpretations about a potential exposure–response relationship in this patient population need to be made with caution.
With regard to OS, we observed that patients who had an objective response lived longer, on average, than patients who did not achieve an objective response (data not shown). Our post hoc exploratory analysis of OS by C min at steady state found that patients in the lowest C min quartile had the shortest median duration of OS compared with patients in the other three quartiles. Taken together with the results of further analysis of baseline characteristics for patients by C min quartile, we can conclude that in the subgroup of patients with the lowest trastuzumab exposure, clinical status was poorer at the time of study entry and disease progression occurred sooner. In the low C min patients, the question of whether the shortest median duration of OS is a consequence of the disease burden or of the low trastuzumab concentration remains. However, except for history of gastrectomy, the tumor burden (as evidenced by presence of visceral metastases, a higher number of metastatic lesions, and a higher number of organs involved) did not influence the PK of trastuzumab, supporting a hypothesis that PK exposure could drive a change in OS.
In the FDA’s exposure–response analysis of data from the ToGA study, C min during cycle 1 was used for the exposure parameter and OS as the response endpoint in a case–control analysis [15]. The FDA analysis found that patients in the lowest quartile of C min during cycle 1 had shorter OS than patients with C min in the higher quartiles. It also found that patients in the lowest quartile for C min had a worse risk profile than patients in the higher C min quartiles. Therefore, the FDA also undertook a case–control analysis in which patients in the lowest quartile of trastuzumab C min were matched for risk factors (ECOG PS, history of gastrectomy, Asian ethnicity, number of metastatic sites, and level of HER2 overexpression) with those in the control arm of the study, who were not receiving trastuzumab. After matching, the differences in patient characteristics were minimized, and none of the risk factors were significant. In this analysis, the median OS was 7.7 months in the lowest trastuzumab C min quartile compared with 7.5 months in the matched control group, suggesting that trastuzumab conferred no benefit in terms of OS when C min during cycle 1 was <11.8 μg/mL [15]. Our covariate analysis in the population PK model complements the risk factors identified by the FDA; in our analysis, six laboratory and patient covariates were found to influence the PK of trastuzumab, such as body weight, serum albumin, gastrectomy, and alkaline phosphatase.
While our analysis and the FDA analyses cannot be directly compared, it is noteworthy that the findings consistently suggest a worse response in patients with the lowest C min values. Taken together, these data suggest that a higher dose of trastuzumab may be required in at least some patients with advanced gastric cancer. The FDA has recommended that a post-marketing trial be conducted to investigate whether the shortened OS within the quartile of patients with lowest C min is due to either poor prognosis associated with the underlying disease or to low trastuzumab exposure. To investigate this question, the Roche HELOISE study (NCT01450696), a phase IIIb study in patients with HER2-positive metastatic gastric or GEJ cancer [22], has been initiated. The inclusion criteria for this study have been informed by the FDA analysis and by the current covariate analysis, as well as by additional analyses performed by the sponsor, such that only patients at high risk of more rapid progression and/or shortened survival (ECOG PS 2 and metastatic disease involving ≥2 organs), without a history of prior treatment for metastatic disease or gastrectomy are eligible for inclusion; these risk factors were chosen based on the analysis results (Supplementary Table S2) where higher proportion of patients in the lowest Cmin quartile subgroup have these risk factors compared with patients in the other three quartile subgroups. Patients are being randomized to receive trastuzumab at the dose studied in ToGA (8 mg/kg loading dose, followed by 6 mg/kg every 3 weeks) or at a higher maintenance dose (8 mg/kg loading dose followed by 10 mg/kg every 3 weeks). Patients with creatinine clearance ≥60 mL/min are also receiving cisplatin at the dose given in the ToGA study (80 mg/m2 on the first day of each 3-week cycle; this dose is reduced by 25 % for patients with creatinine clearance 45–59 mL/min) and capecitabine at a dose of 1,600 mg/m2/day on days 1–14 of each 3-week cycle. This is lower than the capecitabine dose used in ToGA, which was 2,000 mg/m2/day as two divided doses [7]. This study will show whether a higher dose of trastuzumab will improve outcomes. The primary outcome measure is OS based on all randomized patients, but duration of OS, progression-free survival, and objective response rate are also being investigated as secondary endpoints in the subgroup of patients with a trastuzumab Cmin of <12 μg/mL on day 21 of cycle 1. The study is currently recruiting patients, with the aim of having a total of 400 randomized. It is hoped that the results of this study will inform the optimal dosing of trastuzumab in the subset of patients with lower concentrations and poorer survival.
References
Akiyama T, Sudo C, Ogawara H, Toyoshima K, Yamamoto T (1986) The product of the human c-erbB-2 gene: a 185-kilodalton glycoprotein with tyrosine kinase activity. Science 232:1644–1646
Coussens L, Yang-Feng TL, Liao YC et al (1985) Tyrosine kinase receptor with extensive homology to EGF receptor shares chromosomal location with neu oncogene. Science 230:1132–1139
Gravalos C, Jimeno A (2008) HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol 19:1523–1529
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235:177–182
Tanner M, Hollmén M, Junttila TT et al (2005) Amplification of HER-2 in gastric carcinoma: association with Topoisomerase IIalpha gene amplification, intestinal type, poor prognosis and sensitivity to trastuzumab. Ann Oncol 16:273–278
Hofmann M, Stoss O, Shi D et al (2008) Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology 52:797–805
Bang YJ, van Cutsem E, Feyereislova A, ToGA Trial Investigators et al (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376:687–697
Wählby U, Jonsson EN, Karlsson MO (2001) Assessment of actual significance levels for covariate effects in NONMEM. J Pharmacokinet Pharmacodyn 28:231–252
Mould DR, Green B (2010) Pharmacokinetics and pharmacodynamics of monoclonal antibodies: concepts and lessons for drug development. BioDrugs 24:23–39
Dirks NL, Meibohm B (2010) Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet 49:633–659
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Boxenbaum H, Battle M (1995) Effective half-life in clinical pharmacology. J Clin Pharmacol 35:763–766
Yang J, Zhao H, Garnett C et al (2013) The combination of exposure-response and case-control analyses in regulatory decision making. J Clin Pharmacol 53:160–166
Tabrizi MA, Tseng CM, Roskos LK (2006) Elimination mechanisms of therapeutic monoclonal antibodies. Drug Discov Today 11:81–88
Rowinsky EK, Schwartz GH, Gollob JA et al (2004) Safety, pharmacokinetics, and activity of ABX-EGF, a fully human anti-epidermal growth factor receptor monoclonal antibody in patients with metastatic renal cell cancer. J Clin Oncol 22:3003–3015
European Medicines Agency (2012) EPAR summary for the public http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/000278/WC500049819.pdf Accessed 29 Oct 2013
Bruno R, Washington CB, Lu JF, Lieberman G, Banken L, Klein P (2005) Population pharmacokinetics of trastuzumab in patients with HER2+ metastatic breast cancer. Cancer Chemother Pharmacol 56:361–369
Mager DE, Ramanathan M (2007) Preclinical pharmacokinetics. In: Gad SC (ed) Handbook of pharmaceutical biotechnology. Wiley, Hoboken, pp 253–278
Gupta D, Lis CG (2010) Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 9:69
F. Hoffman-La Roche (2013) HELOISE study: a study of Herceptin (trastuzumab) in combination with cisplatin/capecitabine chemotherapy in patients with HER2-positive metastatic gastric or gastro-esophageal junction cancer (NCT01450696). www.clinicaltrials.gov. Accessed 17 Sep 2013
Acknowledgments
The study was funded by F. Hoffmann-La Roche Ltd. Support for third-party writing assistance for this manuscript was provided by Genentech, Inc.
Conflict of interest
Valérie F. Cosson and Michaela Lehle are employed by F. Hoffman-La Roche Ltd. Vivian W. Ng and Bert L. Lum are employed by Genentech, Inc., a member of the Roche group.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cosson, V.F., Ng, V.W., Lehle, M. et al. Population pharmacokinetics and exposure–response analyses of trastuzumab in patients with advanced gastric or gastroesophageal junction cancer. Cancer Chemother Pharmacol 73, 737–747 (2014). https://doi.org/10.1007/s00280-014-2400-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2400-5