Abstract
Purpose
To evaluate, for the first time, the mitomycin C (MMC) pharmacokinetics during intravesical hyperthermia treatment based on conductive heat and the stability and recovery of the drug at the end of the instillation period.
Methods
Eleven patients with recurrent intermediate-risk superficial transitional cell carcinoma of the bladder were treated weekly for six cycles with intravesical MMC (40 mg MMC in 50 ml) in local hyperthermia (45 °C) with Unithermia® system. Each instillation lasted 45 min, with the solution being replaced after the first 22 min. The MMC recovery at the end of the two instillation period and the plasmatic pharmacokinetics of MMC were evaluated by high-pressure liquid chromatography.
Results
Nine patients completed all the six planned cycles, whereas two patients missed the last cycle because of allergic reactions. No other systemic toxicity was observed, and the local toxicities were mild. Median MMC concentration in the instillation residual solution decreases from the initial 0.8 to 0.22 mg/ml for the 0–22-min instillation period and to 0.38 mg/ml for the 22–45-min instillation period; the median percentage of MMC recovered after instillation was 66.2 and 99.6, respectively. In all patients, MMC plasmatic C max resulted considerably lower than the toxic threshold (400 ng/ml).
Conclusions
The MMC is stable during the instillation, and its absorption occurs mainly during the first minutes of the treatment. The plasmatic MMC concentration is always well below the threshold level for myelosuppression, as confirmed by the total lack of hematological toxicity evidenced by the patients. In order to evaluate the efficacy of the treatment performed with UniThermia® in reducing the disease recurrence rate in short- and long-term follow-up, we are currently carrying out a clinical multicentric study involving a larger number of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Superficial transitional cell carcinoma (TCC) of the bladder accounts for more than 90 % of bladder cancers in developed countries. At diagnosis, 70–80 % of TCC are superficial and can be classified as Ta (confined to the urothelium), T1 (invading the lamina propria) or CIS (carcinoma in situ, a highly aggressive type of superficial TCC). According to the World Health Organization (WHO), superficial TCC can be further classified as low grade (grade 1 and 2) or high grade (grade 3) [1].
The standard of treatment for patients with superficial TCC is surgical transurethal resection (TUR) of tumors, performed with the dual purpose to resect every visible tumor and to collect sample tissue for pathological examination. The further treatment of superficial TCC after TUR depends on the degree of the risk of recurrence and progression of the tumor: low-risk TCC (small monofocal TaG1, still not relapsed) presents a low risk of recurrence and progression (20 % recurrence at one year post-TUR) and can be successfully managed with endovesical chemotherapy standard protocols, whereas high-risk TCC (plurifocal T1G2, mono- or plurifocal T1G3) presents a high risk of recurrence and progression (90 % recurrence at one year post-TUR) and should be treated with endovesical instillation of the immunomodulating agent bacille Calmette-Guérin (BCG). At the appearance of tumor multiple recurrences or progression after BCG treatment, the only remaining option is the radical cystectomy [2–4].
However, more than 50 % of the Ta or T1 superficial TCC cannot be classified exactly into the two above-mentioned categories, low and high risk, and they can be defined as intermediate-risk TCC. For the management of intermediate-risk TCC, that is characterized by a low risk of progression (10–15 % at 10 years post-TUR) but a high risk of recurrence (40 % at one year post-TUR) [5], the European Guidelines suggest adjuvant endovesical treatment with conventional cytostatic drugs (e.g., thiotepa, epirubicin or mitomycin C) or the immunomodulating agent BCG [6]. BCG treatment proved to be more effective than cytostatic drugs in preventing tumor recurrence and disease progression [5], but it displays a higher toxicity profile with local adverse effects (frequency, urgency, dysuria and/or hematuria) in up to 90 % of patients and significant systemic adverse effects (systemic BCG infection) in 5 % of patients [7, 8]. Moreover, although BCG treatment is able to significantly reduce the risk of both short-term and long-term recurrence, the rate of recurrence at 2 years remains still rather high, about 38 % [9].
Patients affected by intermediate-risk TCC that relapse after BCG represent a challenging clinical issue as they need repeated TURs. In these patients, on the other hand, radical cystectomy represents an overtreatment, since the risk of progression is low, anyway.
In an attempt to enhance the efficacy of intravesical chemotherapy, a number of different strategies (e.g., electromotive drug administration, local hyperthermia, co-administration of permeation enhancers or bioadhesive carriers) have been proposed and clinically tested. The goal of all these approaches was to improve the penetration and accumulation of drugs in bladder tissues [10–13].
Intravesical thermo-chemotherapy with mitomycin C (MCC) represents one of the most deeply studied strategies. From 1995 to now, in fact, the thermo-chemotherapy was compared with chemotherapy alone in a large number of clinical trial in intermediate- and high-risk patients [14–16]. All the authors agree that the chemo-hyperthermia regimen is more effective than the chemotherapy alone, and the results of a randomized controlled trial in intermediate- and high-risk patients showed that recurrence rate in short-term follow-up (2-year minimum) was significantly lower in the thermo-chemotherapy group (17.1 %), in comparison with MMC-alone group (57.5 %, P < 0.001) [17]. More recently, the results of this trial were updated with the 10-year disease-free survival rate. Data confirm the superiority of thermo-chemotherapy in long-term follow-up also, with a recurrence rate of 40 % for the thermo-chemotherapy group, in comparison with 80 % for MMC-alone group (P < 0.001) [18]. In all published studies, the intravesical thermo-chemotherapy was performed by means of Synergo® (Medical Enterprises, Amsterdam, the Netherlands), a specifically designed system that delivers hyperthermia to the bladder lumen by direct irradiation by a 915-MHz intravesical microwave applicator [19–21]. Paroni et al. [22] demonstrated that local hyperthermia, obtained with the Synergo® system, enhances the systemic absorption of MMC, in comparison with intravesical chemotherapy alone. The higher MMC plasma concentrations obtained with Synergo®, anyway, are safe for the patient, since the level was at all times well below the threshold concentration for myelosuppression. The routine clinical use of Synergo® system, however, is limited by the high costs of the proper catheters needed and the high skillfulness required to assure a correct positioning of the catheter. Furthermore, the direct microwave irradiation could determine a non-uniform temperature distribution that brings the formation of “Hot” or “Cold” spots into the bladder with the risk of burns or lower efficacy of the treatment [21].
More recently, Elmedical has developed UniThermia®, a new system for the delivery of intravesical thermo-chemotherapy based on conductive heat. The UniThermia® system comprises a console (Pelvix™), a peristaltic pump and an heat exchanger, and it is able to deliver intravesical chemotherapy, with moderate heat (42–45 °C) and high flow (whole bladder content replaced 5 times per minute), through a 3-way silicon catheter.
The aim of the study described in this paper was to evaluate, for the first time, the MMC pharmacokinetics during hyperthermia treatment performed with UniThermia® and the stability and recovery of the drug from the residual bladder contents at the end of the instillation period.
Patients and methods
Chemicals
Mitomycin C (MMC) used as standard for the HPLC calibration curve was from Sigma (Milan, Italy). Organic solvents (HPLC grade) were obtained from Carlo Erba (Milan, Italy). The MMC solution used for intravesical instillation was obtained from Kyowa Italiana Farmaceutici s.r.l. (Milan, Italy) and was freshly prepared in 0.9 % saline prior to each treatment.
Equipments
The system used for intravesical thermo-chemotherapy was the Unithermia®, provided from Elmedical (Hod-Hasharon, Israel), and already approved for sale in the European market. Unithermia® is an office-based system composed of a compact console and catheters that allows to obtain an uniform hyperthermia all over the bladder by high flow of a heated MMC solution.
Patients
Eleven patients with recurrent stage Ta and T1, grade G1 or G2, TCC of the bladder were enrolled onto this study in the Department of Urology of San Giovanni Battista-Molinette Hospital of Turin, Italy.
Patients were enrolled if affected by intermediate-risk, stage Ta and T1, grade G1 or G2, mono- or plurifocal (excepted plurifocal T1G2) TCC of the bladder, recurrent after almost a BCG complete cycle of treatment during the previous 24 month. Patients were included with a WHO performance status of 0–2 and an age ≤85 years. Before entering into study, patients underwent complete TUR of all tumors, confirmed by a post-TUR cystoscopy, cold-cup biopsies of suspicious areas and negative urinary cytology.
Exclusion criteria were the following: high-risk TCC (T1G3, CIS, multifocal T1G2, high-grade cellular atypia) or invasive bladder cancer; transitional cell carcinoma of the prostatic urethra or bladder cancer different from TCC; bladder capacity <150 mL or patient unable to hold the urine for at least 1 h; known allergy to MMC; WHO performance status 3–4; age >85 years; WBC count <3.000 cells/mm3 and/or platelets <100.000 cells/mm3; renal and liver function > twice the upper normal limit; urinary tract infection unresponsive to treatment; no previous treatment with BCG and pregnancy or breast feeding.
Before starting the experimental treatment, all patients were required to sign an informed consent form defined according to the Helsinki Committee and approved by the local Ethics Committee. Clinical and demographic characteristics of the patients are shown in Table 1.
Pretreatment and follow-up evaluation
Before starting the treatment, patients underwent complete TUR of all tumors, histological examination of resected tissue, cold-cup biopsies of all suspicious areas, bimanual palpation, blood tests (complete hematological analysis, AST, ALT, LDH, γGT, urea, creatinine), urinalysis with uroculture and urinary cytology, kidney and bladder ultrasound examination, chest radiography and quality-of-life evaluation by EORTC QLQ-C30 and QLQ-BLS24 questionnaires.
Blood tests were repeated before each instillation, and questionnaires were proposed again at the end of 6-cycle treatment and 1 year later.
Patients were monitored by kidney and bladder ultrasound examination after 6 and 12 months and by urinary cytology and cystoscopy every 3 months during the first year and then every 6 months. All lesions detected by cystoscopy were subjected to biopsy, and the recurrence was evaluated by histological examination. Patients with positive cytology without cystoscopically noticeable lesions were subjected to biopsies by a bladder mapping in order to evidence a possible CIS. Patients diagnosed with CIS were withdrawn from the study.
Treatment
Within 24 h from TUR, patients were treated with intravesical MMC in local hyperthermia with Unithermia® system: a solution of 40 mg MMC in 50 ml 0.9 % saline (concentration 0.8 mg/ml), heated at 45 °C, was instilled in the bladder and maintained in continuous circulation for 22 min; then, the bladder was emptied and infused with fresh MMC solution at the same dosage and temperature for a second 23-min period. The same treatment was repeated weekly for a total number of 6 cycles.
Sampling
The MMC recovery at the end of the two instillation periods was evaluated for all the 11 patients in all the instillation cycles, whereas the plasmatic pharmacokinetics of MMC was evaluated during the third cycle for 7 patients.
The volume and pH of the solution recovered from the bladder were measured after both the first 22-min (when the bladder was emptied and the drug solution replaced with a fresh one) and the second 23-min instillation period. Aliquots were stored immediately at −80 °C until analysis.
Blood samples were collected in heparinized tubes immediately before instillation and at 11, 22 (time of replacing the MMC solution), 45 (time of voiding), 75 and 105 min. Plasma was immediately separated by centrifugation and stored at −80 °C until analysis.
Sample preparation
Frozen aliquots of the solution recovered from the bladder were thawed, vortexed for 10 s and centrifuged for 5 min at 15,800×g and 4 °C; then, 20 μl was diluted 1:2,000 in HPLC mobile phase (0.01 M NaH2PO4 buffer pH 6.5/acetonitrile, 84:16) immediately before the HPLC analysis.
MMC was extracted from plasma samples as described by Joseph et al. [23] with minimal modification. Briefly, frozen aliquots of plasma were thawed and vortexed for 10 s, 1 ml of plasma was transferred into a centrifuge tube and 1 ml of acetonitrile was added for protein precipitation and MMC extraction. The tube was vortexed for 1 min and centrifuged for 10 min at 10,000×g; then, the supernatant was transferred into a clean tube. The MMC extraction was repeated with 1 ml of acetonitrile, and the second supernatant was added to the first and dried under nitrogen protected from light. The residue was reconstituted with 400 μl of HPLC mobile phase (0.01 M NaH2PO4 buffer pH 6.5/acetonitrile, 84:16) and analyzed in HPLC.
In vitro degradation of MMC
MMC at concentrations of 0.8 mg/ml was prepared in 0.9 % saline and incubated for up to 60 min at 45 °C protected from light. Samples were diluted in 2,000-fold with mobile phase (0.01 M NaH2PO4 buffer pH 6.5/acetonitrile, 84:16) and analyzed in HPLC.
HPLC analysis of MMC
MMC concentration in plasma and in the solution recovered after the two instillation period was determined by isocratic reverse-phase HPLC by a method adapted from Dalton. et al. [24]. The HPLC system consisted of a Shimadzu LC-10ADvp pump and a Shimadzu SPD-10Avp UV–Vis detector set at 365 nm; the analytical column was a Symmetry C18 (250 × 4.6 mm i.d., particle size 5 μm) equipped with a Symmetry C18 guard column supplied by Waters (Vimodrone, Milan, Italy). The mobile phase consisted of a mixture of 0.01 M NaH2PO4 buffer pH 6.5/acetonitrile (84:16 v/v) and was delivered at 0.8 ml/min at room temperature (20 ± 2 °C). In these conditions, the recovery of MMC was >95 %, its retention time was about 8 min and its limit of quantification (LOQ) was 1 ng/ml.
Results
In vitro degradation of MMC
Incubation of 0.8 mg/ml MMC in 0.9 % saline at 45 °C in the dark for 30, 45 or 60 min resulted in a mean loss of 6.6, 7.6 and 7.9 %, respectively. The MMC stability was comparable to previous published data [22].
MMC recovery in the instillation residual solution at the end of instillation
A total of 64 instillations were performed for the 11 enrolled patients (mean of 5.8 instillation for each patient). The volume and pH of the residual bladder contents were similar for the 0–22 and 22–45-min instillation periods. Median volume was 90 ml (range 65–150) and 100 ml (range 85–150), respectively, whereas median pH was 5.66 (range 5.51–5.92) and 5.81 (range 5.70–5.96), respectively.
Median MMC concentration in the instillation residual solution decreases from the initial 0.8 to 0.22 mg/ml (range 0.11–0.41) for the 0–22-min instillation period and to 0.38 mg/ml (range 0.18–0.59) for the 22–45-min instillation period; the median percentage of MMC recovered after instillation was 66.2 (range 38.6–92.3) and 99.6 (range 68.6–136), respectively. These results indicate that the MMC absorption occurs mainly during the 0–22-min instillation period and that the degradation of MMC maintained at 45 °C in the bladder was minimal, as indicated by the high recovery after the 22–45-min period.
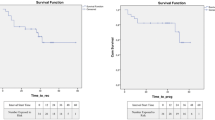
Plasmatic MMC concentration–time profile
Plasmatic MMC concentration–time profiles were examined in 7 patients during the third cycle, in order to better compare our results with those obtained by Paroni et al. [22] that measured the MMC pharmacokinetics at 21–40 days after TUR. Figure 1 shows the plasma MMC concentration–time profiles for the 7 patients; for patient 3, the analysis was repeated during the fourth cycle as the concentrations measured during the third cycle were abnormally high, probably due to an irritation of the bladder wall. In all patients, MMC plasmatic levels were very low, and C max resulted always considerably lower than the reported threshold concentration for toxicity (400 ng/ml), even when the permeability of the bladder wall was increased as occurred in patient 3 (C max = 142 ng/ml). The almost negligible passage of MMC through the bladder into the systemic circulation accounts for the lack of systemic toxicity observed during the treatment for all patients.
Efficacy analysis
The clinical study is still in progress, and the data of efficacy are available for all patients only after 1 year of follow-up. Overall, we observed a recurrence rate of 27.3 % (3 of the 11 patients) during the first year.
Safety analysis
During the positioning of the catheter and the execution of procedure, no technical miscarriage was reported for any of the 64 instillations performed. Nine patients completed all the 6 planned cycles, whereas for 2 patients, the treatment was discontinued at the fifth cycle because of an allergic reaction (skin rash, Grade 3). None of the treated patients complained of nausea or vomiting, and no hematological or other systemic toxicity, apart from allergic reaction, was reported; the reported side effects were local and mild (≤Grade 2) (Table 2). During the endoscopic follow-up, we did not observe neither bladder wall necrosis nor heating injuries.
Discussion
The management of patients affected by intermediate-risk TCC, after TUR, represents a still unsolved problem for the urologic oncology, as this type of TCC is characterized by a low risk of progression, but a high risk of recurrence. Endovesical instillation of BCG proved to be the most effective treatment in order to delay or prevent recurrence, but it is associated with a number of local and systemic side effects and a rate of recurrence of about 38 % after 2 years post-TUR [5, 9]. At present, the only remaining therapeutic options for patients that relapse after BCG are the resection of tumors by repeated TURs (or a radical cystectomy for the worst cases), as intravesical instillation of conventional cytostatic drugs proved to be less effective than BCG in reducing the risk of tumor recurrence [3, 5].
In the last 20 years, a number of different alternative strategies have been tested in order to enhance the penetration of the drug into the tumor, with the aim to increase the efficacy of conventional cytostatic drugs. One of the most promising among these strategies is the intravesical instillation of MMC by thermo-chemotherapy that is able to improve the recurrence-free survival without determining a rising in the local or systemic side effects compared to intravesical chemotherapy alone [18]. Till now, however, each and all the authors that published papers about the application of intravesical thermo-chemotherapy in the treatment of bladder cancer described the use of a microwave-generating device, in order to induce intravesical hyperthermia. This device, distributed by Medical Enterprises with the name of Synergo® is currently already approved by the European Standard Authorities (CE), and it is waiting for approval from the US Food and Drug Administration (FDA). The common clinical application of Synergo® for intravesical thermo-chemotherapy, however, is still limited by the high costs of the necessary equipment and the requirement of expressly trained staff.
In our clinical trial, we evaluated, for the first time, the feasibility of the intravesical thermo-chemotherapy performed by UniThermia®, a new alternative experimental system, based on conductive instead of microwave-induced heating.
At present, some aspects regarding the enhancement obtained by hyperthermia, the extent of systemic absorption of MMC intravesically administered with different protocols and the efficacy of an early instillation of MMC are still unclear. A number of studies demonstrated that an early instillation of MMC (within 24 h from TUR) is able to reduce the odds of tumor recurrence and it is safe, but limited information is available in the literature regarding the systemic absorption of MMC [3]. Very recently, Maffezzini et al. [25] demonstrated low peak blood levels of MMC (average 18.5 ng/ml for large transurethral resection of bladder) after a single-dose instillation given immediately after TUR, with low systemic and local toxicity, but the study was performed with MMC alone, without hyperthermia. Dalton et al. [24] compared the systemic MMC pharmacokinetics in patient treated with intravesical MMC (without hyperthermia) at different time since TUR. The results demonstrated higher peak blood levels of MMC (average 43 ng/ml) in patients treated 1–3 days since TUR, compared to patients treated 1 or more weeks later, but MMC plasma levels were, in any case, below the threshold for toxicity. Finally, Paroni et al. compared the plasmatic MMC pharmacokinetics in patients treated 21–40 days after TUR with intravesical MMC with or without hyperthermia, and observed a significative increase in plasmatic MMC C max in the group treated with hyperthermia compared to the group treated with MMC alone (5.6 vs. 1.1 ng/ml, respectively, P ≤ 0.001), but for all the patients, the levels of MMC were always very low [22].
In this study, 11 patients, affected by intermediate-risk TCC and relapsing after TUR and BCG treatment, were treated with 6 cycles of weekly instillation of MMC 40 mg for 45 min at 45 °C. In our study, we decided to treat the patients with a first cycle 24 h post-TUR in order to benefit from the early instillation, assuming that the plasmatic MMC C max induced by hyperthermia should be only a little higher than the C max described in the literature for intravesical MMC alone [24, 25]. The total lack of systemic toxicity evidenced in our study by the patients during the first cycle demonstrated that the early instillation is safe even if administered in hyperthermia.
The amount of MMC in the residual bladder content at the end of the instillation period was evaluated, in order to determine the stability and the absorption of drug during the treatment, and, at the same time, the systemic exposure of the patients to the drug was assessed by evaluating the MMC plasmatic pharmacokinetics during hyperthermia treatment.
UniThermia® proved to be a safe and easy-to-use system for the delivering of MMC by intravesical thermo-chemotherapy, as no technical miscarriage nor serious side effects was reported. Nine patients completed all the 6 planned cycles, whereas 2 patients missed the last cycle because of an allergic reaction. However, the rate of allergic reaction reported in our study, about 3 %, is comparable with the rate reported in the literature for the use of intravesical MMC alone [9]. No other systemic toxicities were observed; the local toxicities were in any case mild.
MMC at concentration of 0.8 mg/ml in 0.9 % saline showed a good stability (less than 10 % loss) after a 60-min incubation in vitro at 45 °C in the dark. This finding was confirmed by the good intravesical MMC stability during the 22–45-min instillation period, with a recovery of 99.6 % in the residual bladder content. Despite this stability, our results suggest to maintain a schedule that provides for a replacement of MMC solution after the first 22 min of treatment, since the MMC absorption occurs mainly during the first minutes of instillation, as demonstrated by the low amount of recovered MMC (66.2 %) at the end of this period. For that reason, the replacement of instillation solution is important to assure an optimal intravesical concentration of MMC for the entire duration of the hyperthermia treatment.
The plasmatic MMC concentration during the instillation was always very low and well below the threshold level for myelosuppression, even if the permeability of the bladder wall is increased as a result of an inflammatory condition or the TUR procedure. This finding was well confirmed by the total lack of hematological toxicity evidenced by the patients during the study.
The results obtained in our study demonstrate that the MMC stability and systemic absorption during the hyperthermia treatment performed with UniThermia® are comparable with the results described by Paroni et al. [17, 22] with the Synergo® system.
The use of conductive heating in order to induce intravesical hyperthermia prevents the risk of burns during the treatment, as demonstrated by the total lack of bladder wall necrosis or heating injuries observed in our patients during the endoscopic follow-up. However, the temperature of the bladder wall has not been monitored during the procedure; therefore, the efficacy of conductive heating to uniformly increase the temperature across the different layers of bladder wall is still to be demonstrated, as the blood flow could dissipate the heat, especially at submucose and muscle level. Very recently, Cordeiro et al. [26] described a novel multisensor probe for monitoring bladder temperature during locoregional thermo-chemotherapy. This probe should be useful in order to resolve this issue.
In order to evaluate the efficacy of the treatment performed with UniThermia® in reducing the disease recurrence rate in short- and long-term follow-up, we are currently carrying out a clinical multicentric study involving a larger number of patients.
References
Epstein JI, Amin MB, Reuter VR, Mostofi FK (1998) The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol 22(12):1435–1448
Vogeli TA (2005) The management of superficial transitional cell carcinoma of the bladder: a critical assessment of contemporary concepts and future perspectives. BJU Int 96(8):1171–1176. doi:10.1111/j.1464-410X.2005.05928.x
Witjes JA, Hendricksen K (2008) Intravesical pharmacotherapy for non-muscle-invasive bladder cancer: a critical analysis of currently available drugs, treatment schedules, and long-term results. Eur Urol 53(1):45–52. doi:10.1016/j.eururo.2007.08.015
Kaufman DS, Shipley WU, Feldman AS (2009) Bladder cancer. Lancet 374(9685):239–249. doi:10.1016/S0140-6736(09)60491-8
Shelley MD, Mason MD, Kynaston H (2010) Intravesical therapy for superficial bladder cancer: a systematic review of randomised trials and meta-analyses. Cancer Treat Rev 36(3):195–205. doi:10.1016/j.ctrv.2009.12.005
Roupret M, Babjuk M, Comperat E, Zigeuner R, Sylvester R, Burger M, Cowan N, Bohle A, Van Rhijn BW, Kaasinen E, Palou J, Shariat SF (2013) European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. doi:10.1016/j.eururo.2013.03.032
Lamm DL, Steg A, Boccon-Gibod L, Morales A, Hanna MG Jr, Pagano F, Alfthan O, Brosman S, Fisher HA, Jakse G et al (1989) Complications of Bacillus Calmette-Guerin immunotherapy: review of 2602 patients and comparison of chemotherapy complications. Prog Clin Biol Res 310:335–355
Horvath A, Mostafid H (2009) Therapeutic options in the management of intermediate-risk nonmuscle-invasive bladder cancer. BJU Int 103(6):726–729. doi:10.1111/j.1464-410X.2008.08094.x
Bohle A, Jocham D, Bock PR (2003) Intravesical Bacillus Calmette-Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. J Urol 169(1):90–95. doi:10.1097/01.ju.0000039680.90768.b3
Dalbagni G (2007) The management of superficial bladder cancer. Nat Clin Pract Urol 4(5):254–260. doi:10.1038/ncpuro0784
Gwynn ES, Clark PE (2006) Bladder cancer. Curr Opin Oncol 18(3):277–283. doi:10.1097/01.cco.0000219258.75961.1a
Hendricksen K, Witjes JA (2007) Current strategies for first and second line intravesical therapy for nonmuscle invasive bladder cancer. Curr Opin Urol 17(5):352–357. doi:10.1097/MOU.0b013e3281c55f2b
Shen Z, Shen T, Wientjes MG, O’Donnell MA, Au JL (2008) Intravesical treatments of bladder cancer: review. Pharm Res 25(7):1500–1510. doi:10.1007/s11095-008-9566-7
Gofrit ON, Shapiro A, Pode D, Sidi A, Nativ O, Leib Z, Witjes JA, van der Heijden AG, Naspro R, Colombo R (2004) Combined local bladder hyperthermia and intravesical chemotherapy for the treatment of high-grade superficial bladder cancer. Urology 63(3):466–471. doi:10.1016/j.urology.2003.10.036
Lammers RJ, Witjes JA, Inman BA, Leibovitch I, Laufer M, Nativ O, Colombo R (2011) The role of a combined regimen with intravesical chemotherapy and hyperthermia in the management of non-muscle-invasive bladder cancer: a systematic review. Eur Urol 60(1):81–93. doi:10.1016/j.eururo.2011.04.023
Rampersaud EN, Vujaskovic Z, Inman BA (2010) Hyperthermia as a treatment for bladder cancer. Oncology (Williston Park) 24(12):1149–1155
Colombo R, Da Pozzo LF, Salonia A, Rigatti P, Leib Z, Baniel J, Caldarera E, Pavone-Macaluso M (2003) Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma. J Clin Oncol 21(23):4270–4276. doi:10.1200/JCO.2003.01.089
Colombo R, Salonia A, Leib Z, Pavone-Macaluso M, Engelstein D (2010) Long-term outcomes of a randomized controlled trial comparing thermochemotherapy with mitomycin-C alone as adjuvant treatment for non-muscle-invasive bladder cancer (NMIBC). BJU Int 107(6):912–918. doi:10.1111/j.1464-410X.2010.09654.x
Colombo R, Da Pozzo LF, Lev A, Salonia A, Rigatti P, Leib Z, Servadio C, Caldarera E, Pavone-Macaluso M (1998) Local microwave hyperthermia and intravesical chemotherapy as bladder sparing treatment for select multifocal and unresectable superficial bladder tumors. J Urol 159(3):783–787
Colombo R, Lev A, Da Pozzo LF, Freschi M, Gallus G, Rigatti P (1995) A new approach using local combined microwave hyperthermia and chemotherapy in superficial transitional bladder carcinoma treatment. J Urol 153(3 Pt 2):959–963
Colombo R, Salonia A, Da Pozzo LF, Naspro R, Freschi M, Paroni R, Pavone-Macaluso M, Rigatti P (2003) Combination of intravesical chemotherapy and hyperthermia for the treatment of superficial bladder cancer: preliminary clinical experience. Crit Rev Oncol Hematol 47(2):127–139
Paroni R, Salonia A, Lev A, Da Pozzo LF, Cighetti G, Montorsi F, Rigatti P, Colombo R (2001) Effect of local hyperthermia of the bladder on mitomycin C pharmacokinetics during intravesical chemotherapy for the treatment of superficial transitional cell carcinoma. Br J Clin Pharmacol 52(3):273–278
Joseph G, Biederbick W, Woschee U, Theisohn M, Klaus W (1997) Sensitive and convenient high-performance liquid chromatographic method for the determination of mitomycin C in human plasma. J Chromatogr B Biomed Sci Appl 698(1–2):261–267
Dalton JT, Wientjes MG, Badalament RA, Drago JR, Au JL (1991) Pharmacokinetics of intravesical mitomycin C in superficial bladder cancer patients. Cancer Res 51(19):5144–5152
Maffezzini M, Campodonico F, Manuputty EE, Puntoni M, Martelli A, Marini V, Tamagno S, Mattioli F (2013) Systemic absorption and pharmacokinetics of single-dose early intravesical mitomycin C after transurethral resection of non-muscle-invasive bladder cancer. Urology 82(2):400–404. doi:10.1016/j.urology.2013.03.036
Cordeiro ER, Geijsen DE, Zum Vorde Sive Vording PJ, Schooneveldt G, Sijbrands J, Hulshof MC, de la Rosette J, de Reijke TM, Crezee H (2013) Novel multisensor probe for monitoring bladder temperature during locoregional chemohyperthermia for nonmuscle-invasive bladder cancer: technical feasibility study. J Endourol 27(12):1504–1509. doi:10.1089/end 2013.0179
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milla, P., Fiorito, C., Soria, F. et al. Intravesical thermo-chemotherapy based on conductive heat: a first pharmacokinetic study with Mitomycin C in superficial transitional cell carcinoma patients. Cancer Chemother Pharmacol 73, 503–509 (2014). https://doi.org/10.1007/s00280-014-2381-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2381-4