Abstract
Purpose
Monitoring of plasma methotrexate (MTX) concentrations allows for therapeutic adjustments in treating childhood acute lymphoblastic leukemia (ALL) or non-Hodgkin lymphoma (NHL) with high-dose MTX (HDMTX). We tested the hypothesis that assessment of creatinine clearance (CrCl) and/or serum Cr may be a suitable means of monitoring plasma MTX concentrations.
Methods
All children in the study had ALL or NHL, were in complete remission, and received HDMTX (3 or 5 g/m2)+leucovorin. Plasma MTX concentrations were measured at 24, 48, and 96 h. CrCl was determined at 24 and 48 h. Correlations between 24- and 48-h plasma MTX concentrations and CrCl and serum Cr concentrations were determined. CrCl and serum Cr concentrations were compared over time between children who had delayed and non-delayed MTX elimination.
Results
A total of 105 children were included. There were significant negative correlations between CrCl at 24 and 48 h and plasma MTX concentrations at 24 (both p < 0.001) and 48 h (both p < 0.001). There were significant positive correlations between serum Cr concentrations at both 24 and 48 h and plasma MTX concentrations at 24 (both p < 0.001) and 48 h (both p < 0.001). There were 88 (30.2 %) instances of elimination delay. Children with elimination delay had significantly lower CrCl and higher Cr concentrations at 24 and 48 h compared with children without elimination delay (all p < 0.05).
Conclusion
Our findings suggest that, with further refinement, assessment of renal function may be a useful means of monitoring plasma MTX concentrations during HDMTX for ALL and NHL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-dose methotrexate (HDMTX) chemotherapy with leucovorin (LV) rescue is the mainstay of treatment for preventing extramedullary infiltration in childhood acute lymphoblastic leukemia (ALL) [1]. Despite the fact that HDMTX is a very effective treatment, plasma MTX concentrations may become excessively high in a small proportion of patients, resulting in toxicity and elimination delay [2, 3]. Elimination delay may lead to kidney and/or liver dysfunction, bone marrow suppression, oral mucosal lesions, secondary infection, and delays in the next course of chemotherapy [2, 4]. Renal toxicity is a particular concern [5]. In contrast, lower than optimal concentrations of MTX can result in a greater risk of relapse [6–8]. Hence, optimizing the dose of HDMTX through therapeutic monitoring is critical for maximizing the therapeutic benefit, reducing the risk of potential harms, and indeed reducing the cost of treatment.
In developed countries, careful monitoring of plasma MTX concentrations generally allows for appropriate adjustments of MTX and LV dose, hydration, and alkalization to minimize the risk of elimination delay/MTX toxicity. Indeed, using such methods, we previously reported that a MTX dose of 3–5 g/m2 was safe [4]. Recent reports have also highlighted the utility of measuring plasma MTX concentrations to individualize dosing based on MTX clearance [9] and, in conjunction with other factors (e.g. LV, urinary pH, hydration), for generating an algorithm to predict subsequent MTX concentrations [10]. Unfortunately, monitoring of plasma MTX concentrations is not always possible or feasible in less developed countries because of the limited availability of appropriate equipment, the associated analytical costs, and the lack of suitably trained staff [11]. In such settings, having a simple, alternative/indirect means of monitoring plasma MTX concentrations would be of obvious use.
Methotrexate is predominantly eliminated by the kidneys [12–14]. Indeed, 70–90 % of the administered MTX dose is excreted unchanged in the urine [13]. Therefore, we hypothesized that assessment of renal function by measuring the creatinine clearance (CrCl) and/or serum Cr may be a suitable means of monitoring plasma MTX concentrations in place of direct plasma measurement. Such monitoring, if found to be appropriate, would potentially allow for the real-time optimization of MTX therapy (as opposed to delayed optimization with direct monitoring of plasma MTX concentrations). To test this hypothesis, we conducted a retrospective study of children with ALL and non-Hodgkin’s lymphoma (NHL) who received HDMTX therapy at our hospital. Specifically, we assessed correlations between 24- and 48-h plasma MTX concentrations and the CrCl and serum Cr concentration at 24 and 48 h. We also compared the endogenous CrCl and serum Cr concentration between children who had delayed and non-delayed elimination of MTX.
Materials and methods
Patients
This study involved children with ALL and NHL who were treated at our hospital from May 2009 to December 2009.
Patients with ALL were classified as being high, moderate, or low risk according to previously described criteria [15]. Another 10 NHL patients are included to low-risk group. All children were in complete remission and had received HDMTX+LV to prevent extramedullary infiltration. HDMTX was administered after consolidation and during maintenance therapy. Prior to each HDMTX dose, children were required to have a white blood cell count ≥3.0 × 109/L, an absolute neutrophil count >1.0 × 109/L, and a platelet count ≥80 × 109/L, without any evidence of liver or kidney impairment, or infection.
The study was approved by the Medical Ethics Committee of Children’s Hospital of Zhejiang University (2012096).
High-dose methotrexate regimen
Low-severity children received MTX 3 g/m2, whereas moderate- and high-severity children received MTX 5 g/m2. The first dose (1/5–1/6 of the full dose; no more than 500 mg) was intravenously transfused within 1 h. The remainder of the full dose was infused during the following 23 h. Patients underwent urinary alkalinization with sodium bicarbonate and received hydration therapy starting 3 days before to chemotherapy. Low-risk children received 5 % sodium bicarbonate (3–4 mL/kg/day) and saline (2,000–3,000 mL/m2/day) for 4 days, whereas moderate- and high-risk children received 5 % sodium bicarbonate (4–5 mL/kg/day) and saline (3,000–4,000 mL/m2/day for 5 days. Thiourea (6-thioguanine) purine (50 mg/m2) was given to keep mild bone marrow suppression state [16].
Leucovorin rescue (LV) regimen
Leucovorin rescue was commenced 36 h of the start of MTX treatment. The first dose was 15 mg/m2 for low-severity children and 30 mg/m2 for moderate- and high-severity children. Thereafter, for children without elimination delay, LV (15 mg/m2) was given once every 6 h until the plasma MTX concentration was <0.1 μmol/L. A total of 5–8 LV doses were given. For children with elimination delay, the LV rescue regimen was prescribed as previously detailed [16] until the plasma MTX concentration was <0.1 μmol/L.
Measurement of plasma methotrexate concentrations
Plasma MTX concentrations were measured 24, 48, and 96 h after the start of treatment by fluorescent polarization immunoassay. For children with elimination delay, monitoring was stopped when the plasma MTX concentrations were <0.1 μmol/L.
Endogenous creatinine clearance
Twenty-four-hour urine samples were collected over the first 48 h after the start of chemotherapy and treated with 6 N HCl as preservative. After mixing, a portion of the sample was used to measure the urine Cr concentration. Within the last hour of urine sample collection, a venous blood sample was drawn for the measurement of serum Cr concentrations. The following formula was used to calculate the endogenous CrCl:
CrCl = urine Cr (mg/dL) × 24 h urine volume (mL) × 1.73 m2/body surface area (m2) × plasma Cr (mg/dL) × 1,440.
Criteria for elimination delay
The plasma concentration of MTX at 24 h can predict efficacy, whereas the plasma concentrations of MTX at 48 and 96 h can reflect the excretion of MTX. Elimination delay was indicated by MTX concentrations >1.0 μmol/L at 48 h and >0.1 μmol/L at 96 h [16].
Statistical analysis
Generalized estimating equations (GEE) were used to estimate the relationship between children’s characteristics (MTX dose, alkalization, hydration, CrCl, and serum Cr) and plasma MTX concentrations because most children received more than two courses of MTX (hence, the data are related). An independence model criterion [quasi-likelihood information criterion (QIC)] was used to select the best working correlation structure arising from the GEE analyses. The smaller the QIC, the stronger the correlation.
To predict the probability of elimination delay based on clinical variables, a classification and regression tree (CART) model was used. Variables including age, gender, MTX dose, severity group, hydration on the first day of chemotherapy, hydration on the second day of chemotherapy, serum creatinine level before MTX infusion, serum creatinine level after 24-h MTX infusion, serum creatinine level after 48-h MTX infusion, creatinine clearance before MTX infusion, creatinine clearance 24 h after MTX infusion, and creatinine clearance 48 h after MTX infusion were included in the CART model.
All statistical assessments were two-tailed and considered statistically significant at the 0.05 level. Statistical analyses were performed using SPSS 15.0 statistical software (SPSS Inc., Chicago, IL).
Results
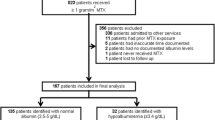
A total of 95 children with ALL and 10 children with NHL were included in the study (N = 105). The demographic and clinical characteristics of the children are summarized in Table 1. Most children were male (63.8 %) and had grade I disease (46.7 %). The children received a total of 291 courses of HDMTX.
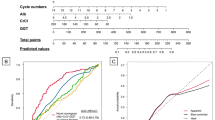
The correlations between the plasma MTX concentration at 24 h and the children’s characteristics are summarized in Fig. 1. There was a significant positive correlation between the MTX dose and the plasma MTX concentration at 24 h (p < 0.001, Fig. 1a). After adjusting for the MTX dose, there were significant positive correlations between alkalization plus hydration on the first day and second day of chemotherapy and plasma MTX concentrations at 24 h (both p < 0.001, Fig. 1b, c). There were significant negative correlations between the CrCl at both 24 and 48 h and the plasma MTX concentration at 24 h (both p < 0.001, Fig. 1d, f). In contrast, there were significant positive correlations between serum Cr concentrations at both 24 and 48 h and the plasma MTX concentration at 24 h (both p < 0.001, Fig. 1e, g). According to the QIC, the serum Cr concentration at 24 h had the strongest working positive correlation with the plasma MTX concentration at 24 h (QICserum Cr concentration at 24 h = 153,489 < QICserum Cr concentration at 48 h = 157,350).
Relationship between children’s characteristics [MTX dose (a), alkalization and hydration (b and c), creatinine clearance (d and f), and serum creatinine concentration (e and g)] and plasma methotrexate (MTX) concentrations 24 h after the start of high-dose MTX for acute lymphoblastic leukemia. Generalized estimating equations (GEE) were used to estimate the relationship between children’s characteristics and plasma MTX concentrations. An independence model criterion (QIC) was used to select the best working correlation structure arising from the GEE analyses. *Indicates statistical significance
The correlations between the plasma MTX concentration at 48 h and children’s characteristics are summarized in Fig. 2. There was no correlation between the MTX dose and the plasma MTX concentration at 48 h (p = 0.231, Fig. 2a). After adjusting for the MTX dose, there were significant negative correlations between alkalization plus hydration on the first day and second day of chemotherapy and the plasma MTX concentration at 48 h (p = 0.015 and 0.035, respectively, Fig. 2b, c). There were significant negative correlations between the CrCl at both 24 and 48 h and the plasma MTX concentration at 48 h (both p < 0.001, Fig. 2d, f). In contrast, there were significant positive correlations between the serum Cr concentrations at both 24 and 48 h and the plasma MTX concentration at 48 h (both p = 0.001, Fig. 2e, g). According to the QIC, the serum Cr concentration at 48 h had the strongest working positive correlation with the plasma MTX concentration at 48 h (QICserum Cr concentration at 48 h = 530 < QICserum Cr concentration at 24 h = 944).
Relationship between children’s characteristics [MTX dose (a), alkalization and hydration (b and c), creatinine clearance (d and f), and serum creatinine concentration (e and g)] and plasma methotrexate (MTX) concentrations 48 h after the start of high-dose MTX for acute lymphoblastic leukemia. Generalized estimating equations (GEE) were used to estimate the relationship between children’s characteristics and plasma MTX concentrations. An independence model criterion (QIC) was used to select the best working correlation structure arising from the GEE analyses. *Indicates statistical significance
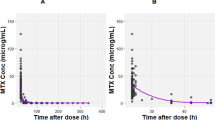
There were a total of 88 (30.2 %) instances of elimination delay. Children with elimination delay had significantly lower CrCl and significantly higher serum Cr concentrations at 24 and 48 h compared with children who did not have elimination delay (all p < 0.05, Fig. 3). There was no significant difference of Cr and CrCl between two groups at the 0 h, before the start of treatment.
Summary of the creatinine clearance rate (CrCl) and serum creatinine (Cr) concentrations over time for children with and without elimination delay of methotrexate (MTX) after high-dose MTX for acute lymphoblastic leukemia. Elimination delay was indicated by an MTX concentration >1.0 μmol/L at 48 h and >0.1 μmol/L at 96 h. *Indicates a statistically significant between-group difference (p < 0.05)
The CART model generated a tree containing three terminal nodes (Fig. 4). The percentage of treatments with elimination delay ranged from 11 to 75 % in these three nodes. The first variable selected for splitting was serum creatinine level >42.15 mmol/L at 48 h (Gini = 0.105). For the treatments which involved elimination delay, further splitting was based whether or not serum creatinine levels at 48 h were >29.40 mmol/L (Gini = 0.010).
Discussion
In this study, we tested the hypothesis that assessing renal function may be a suitable means of monitoring plasma MTX concentrations after HDMTX for childhood ALL. Of note, we found that the CrCl at both 24 and 48 h after the start of HDMTX was significantly correlated with plasma MTX concentrations at 24 and 48 h. Likewise, serum Cr concentrations were significantly correlated with plasma MTX concentrations at these times.
To achieve optimal efficacy and low toxicity in the clinical treatment of ALL, the plasma MTX concentration should be sufficiently high after 24 h and relatively low, indicating timely excretion, after 48 h. Therefore, we examined factors associated with plasma MTX concentrations at 24, 48, and 96 h after the start of HDMTX. Further, we focused on examining indicators of renal function because MTX is predominantly eliminated via the kidneys [13].
As already noted, we found that the 24- and 48-h CrCl and Cr concentrations were significantly correlated (negatively and positively, respectively) with plasma MTX concentrations at 24 and 48 h. Of note, the serum creatinine at 48 h had the strongest correlation with the plasma MTX concentration at 48 h and may therefore be a good predictor of elimination delay according to QIC. A number of previous studies have reported on the relationship between plasma MTX concentrations and CrCl. Like us, Hempel et al. [17] found that there was a negative correlation between plasma MTX concentrations and the CrCl in predominately pediatric patients with ALL, NHL, osteosarcoma, malignant brain tumor, or ALL relapse who received HDMTX. In contrast, Relling et al. [3], Evans et al. [18], and Joannon et al. [19] reported that plasma MTX concentrations were not associated with CrCl. The lack of agreement with our finding may be explained by the fact that lower-dose MTX regimens (0.9–3.7 g/m2) were used in these studies [3, 18, 19]. Our findings suggest that routine assessment of renal function may be suitable means of monitoring plasma MTX concentrations in settings where direct monitoring of plasma MTX concentrations is not possible. Clearly, further study is needed to examine this possibility with the requisite detail. Nevertheless, we feel that our findings are promising and may be clinically relevant.
We also found that both the CrCl and serum Cr concentrations were not different before chemotherapy between patients who had subsequent elimination delay and those who had non-delayed elimination. However, the CrCl was significantly lower and serum Cr concentrations were significantly higher at both 24 and 48 h in patients with delayed elimination compared with those who did not have delayed elimination. These findings indicate that HDMTX was the cause of renal excretion dysfunction, rather than pre-existing renal dysfunction being the cause of delayed MTX excretion after HDMTX chemotherapy.
In addition to examining the relationship between measures of renal function and plasma MTX concentrations, we also examined the relationship between MTX dose, alkalization, and hydration and plasma MTX concentrations. Of note, we found that the 24-h plasma MTX concentration had a strong correlation with MTX dose. This finding indicates that, for patients who do not achieve the target plasma MTX concentration at 24 h, increasing the MTX dose may improve efficacy. Further, we also found that there was a significant negative correlation between hydration plus alkalinization on the first and second day of chemotherapy and the plasma MTX concentration at 48 h. In contrast, hydration plus alkalinization on the first day of chemotherapy did not affect the plasma MTX concentration at 24 h. These results indicate that hydration and alkalinization on the first and second day of chemotherapy can be increased to promote the rate of MTX metabolism and at the same time reduce the occurrence of elimination delay without any reduction in treatment effect.
Our study has a number of limitations that warrant mention. First, the lack of homogeneity in the severity of disease may have affected our results. In our previous study [4], although we found that there was no significant difference in the elimination delay rates among patients with different risk levels, this may have been because all patients were in complete remission. Second, the follow-up was not long enough to observe the extramedullary infiltration rate for effect evaluation. Hence, further studies are needed with more homogenous cohorts with respect to the severity of disease. Finally, we acknowledge that our sample size was relatively modest. Further large-scale studies are needed to confirm our findings and to obtain data for more definitive analyses to determine whether measures of renal function may be used to monitor plasma MTX concentrations after HDMTX for ALL.
Conclusions
In summary, we have found that markers of renal function, namely CrCl and serum Cr concentration, correlate with plasma MTX concentrations after HDMTX for childhood ALL. These findings are encouraging and suggest that it may be possible to indirectly monitor plasma MTX concentrations during HDMTX by assessing renal function. Such indirect monitoring would be of clinical use in settings where direct monitoring of plasma MTX is not possible/feasible.
References
Pui CH (2010) Recent research advances in childhood acute lymphoblastic leukemia. J Formos Med Assoc 109:777–787
Rask C, Albertioni F, Bentzen SM, Schroeder H, Peterson C (1998) Clinical and pharmacokinetic risk factors for high-dose methotrexate-induced toxicity in children with acute lymphoblastic leukemia–a logistic regression analysis. Acta Oncol 37:277–284
Relling MV, Fairclough D, Ayers D, Crom WR, Rodman JH, Pui CH, Evans WE (1994) Patient characteristics associated with high-risk methotrexate concentrations and toxicity. J Clin Oncol 12:1667–1672
Xu W, Tang Y, Song H, Shi S, Yang S (2007) Retrospective study on elimination delay of methotrexate in high-dose therapy of childhood acute lymphoblastic leukemia in China. J Pediatr Hematol Oncol 29:688–693
Takami M, Kuniyoshi Y, Oomukai T, Ishida T, Yamano Y (1995) Severe complications after high-dose methotrexate treatment. Acta Oncol 34:611–612
Borsi JD, Revesz T, Schuler D (1987) Prognostic importance of systemic clearance of methotrexate in childhood acute lymphoblastic leukemia. Cancer Chemother Pharmacol 19:261–264
Camitta B, Leventhal B, Lauer S, Shuster JJ, Adair S, Casper J, Civin C, Graham M, Mahoney D, Munoz L et al (1989) Intermediate-dose intravenous methotrexate and mercaptopurine therapy for non-T, non-B acute lymphocytic leukemia of childhood: a Pediatric Oncology Group study. J Clin Oncol 7:1539–1544
Seidel H, Nygaard R, Moe PJ, Jacobsen G, Lindqvist B, Slordal L (1997) On the prognostic value of systemic methotrexate clearance in childhood acute lymphocytic leukemia. Leuk Res 21:429–434
Pauley JL, Panetta JC, Crews KR, Pei D, Cheng C, McCormick J, Howard SC, Sandlund JT, Jeha S, Ribeiro R, Rubnitz J, Pui CH, Evans WE, Relling MV (2013) Between-course targeting of methotrexate exposure using pharmacokinetically guided dosage adjustments. Cancer Chemother Pharmacol 72:369–378
Dombrowsky E, Jayaraman B, Narayan M, Barrett JS (2011) Evaluating performance of a decision support system to improve methotrexate pharmacotherapy in children and young adults with cancer. Ther Drug Monit 33:99–107
Kapoor G, Sinha R, Abedin S (2012) Experience with high dose methotrexate therapy in childhood acute lymphoblastic leukemia in a tertiary care cancer centre of a developing country. Pediatr Blood Cancer 59:448–453
Skarby T, Jonsson P, Hjorth L, Behrentz M, Bjork O, Forestier E, Jarfelt M, Lonnerholm G, Hoglund P (2003) High-dose methotrexate: on the relationship of methotrexate elimination time vs renal function and serum methotrexate levels in 1164 courses in 264 Swedish children with acute lymphoblastic leukaemia (ALL). Cancer Chemother Pharmacol 51:311–320
Pizzo PA, Poplack DG (2006) Principles and practice of pediatric oncology. Lippincott Williams & Wilkins, Philadelphia
Fukuhara K, Ikawa K, Morikawa N, Kumagai K (2008) Population pharmacokinetics of high-dose methotrexate in Japanese adult patients with malignancies: a concurrent analysis of the serum and urine concentration data. J Clin Pharm Ther 33:677–684
Tang Y, Xu X, Song H, Yang S, Shi S, Wei J (2008) Long-term outcome of childhood acute lymphoblastic leukemia treated in China. Pediatr Blood Cancer 51:380–386
Ye H, Gu L, Chen J (2001) High-dose methotrexate therapy in children with acute lymphoblastic leukemia. Chin J Hematol 22:385–386
Hempel L, Misselwitz J, Fleck C, Kentouche K, Leder C, Appenroth D, Rost M, Zintl F (2003) Influence of high-dose methotrexate therapy (HD-MTX) on glomerular and tubular kidney function. Med Pediatr Oncol 40:348–354
Evans WE, Crom WR, Stewart CF, Bowman WP, Chen CH, Abromowitch M, Simone JV (1984) Methotrexate systemic clearance influences probability of relapse in children with standard-risk acute lymphocytic leukaemia. Lancet 1:359–362
Joannon P, Oviedo I, Campbell M, Tordecilla J (2004) High-dose methotrexate therapy of childhood acute lymphoblastic leukemia: lack of relation between serum methotrexate concentration and creatinine clearance. Pediatr Blood Cancer 43:17–22
Acknowledgments
This work was supported in part by the grant from National Natural Science Foundation of China (81100338); Science Technology Department of Zhejian Province, Qianjiang project (2009R10037); and Zhejiang Provincial Natural Scientific Foundation (NoY2100070).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, Wq., Zhang, Ly., Chen, Xy. et al. Serum creatinine and creatinine clearance for predicting plasma methotrexate concentrations after high-dose methotrexate chemotherapy for the treatment for childhood lymphoblastic malignancies. Cancer Chemother Pharmacol 73, 79–86 (2014). https://doi.org/10.1007/s00280-013-2319-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2319-2