Abstract
Purpose
Everolimus, an oral inhibitor of mammalian target of rapamycin, can augment the efficacy of HER inhibitors in preclinical studies. This study was conducted to determine the safety and pharmacokinetics (PK) of the combination of lapatinib, a Her1 and 2 inhibitor, and everolimus and to describe its anti-tumor activity in the Phase I setting.
Methods
In Part I, dose escalation to define the maximum tolerated dose (MTD) was performed. In Part II, PK of both drugs were analyzed to assess drug–drug interaction.
Results
Twenty-three evaluable patients with advanced cancers were treated on six different dose levels in Part I of the study. The dose-limiting toxicities were diarrhea, rash, mucositis, and fatigue. The MTD of the combination was 1,250 mg of lapatinib and 5 mg of everolimus once daily. In Part II of the study, 54 patients were treated with the combination at the MTD. The mean everolimus time to maximum concentration was increased by 44 %, and mean clearance was decreased by 25 % when co-administered with lapatinib, though these differences were not statistically significant. There was no significant influence on the PK of lapatinib by everolimus. Two patients achieved a partial response [thymic cancer (45+ months) and breast cancer (unconfirmed PR; 7 months)]; 11 patients attained stable disease of at least 4 months.
Conclusions
Lapatinib and everolimus are well tolerated at doses of 1,250 and 5 mg po daily, respectively. Stable disease ≥4 months/PR was achieved in 13 of 78 patients (17 %).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The epidermal growth factor family of receptors has been shown to be crucial to the development of many cancers [1]. Drugs targeting members of this family have lead to clinical benefit in various malignancies, including non-small-cell lung and breast cancer. Lapatinib is an orally available small molecule reversible inhibitor of both Her2 and Her1 tyrosine kinases [2] and is currently approved for the treatment of Her2-amplified breast cancer in combination with capecitabine [3].
The downstream pathways activated by these receptors include the PI3K/Akt and the Ras/Raf/Erk/MAPK signals. These signals activate many cellular events, including proliferation, anti-apoptosis, and metastatic invasion. One of the downstream effectors of the PI3K/Akt pathway is mammalian target of rapamycin (mTOR) [4], a Ser/Thr protein kinase, that is a key factor in cellular growth and homeostasis. Rapamycin binds to the cytosolic protein FKBP12 inhibiting mTOR. Everolimus is an oral rapamycin analogue approved for the treatment of advanced renal cell carcinoma patients, neuroendocrine tumors, and estrogen receptor (ER)-positive breast cancers in combination with exemestane [5–7].
Persistent PI3K/Akt pathway activity is an important mechanism of resistance to Her inhibitors. Since mTOR is an effector protein of the PI3K/Akt pathway, there is interest in evaluating the ability of mTOR inhibitors to enhance the activity of Her inhibitors [8–10]. Further, since both these drugs are used in breast cancer, information on their safety profile in combination may be useful. We conducted a Phase I study to determine the maximum tolerated dose (MTD) of the combination of lapatinib and everolimus and to evaluate the potential pharmacokinetic (PK) interactions during co-administration, as well as to describe any anti-tumor activity observed.
Methods
This study was conducted by the Early Therapeutics Committee of Southwest Oncology Group (SWOG). All patients were informed of the investigational nature of this study and signed a written informed consent in accordance with local institutional review board and federal guidelines. The study was conducted in two parts. Part I was performed in order to determine the MTD of the combination. In Part II, PK interactions were assessed. For Part II of the study, patients were randomly assigned to two cohorts. In Cohort A, the PK of everolimus alone, and with lapatinib, were assessed; in Cohort B, the PK of lapatinib alone, and with everolimus, were assessed.
Eligibility
Patients with advanced solid tumors for whom there was no effective therapy were eligible. Patients were required to have a Zubrod performance status of 0–2 (similar to ECOG performance status 0–2) and adequate hematologic, renal and hepatic function. Patients were also required to have a normal cardiac ejection fraction, assessed either with multi-gated acquisition (MUGA) scan or echocardiography.
Study evaluation and follow-up
Patients underwent a complete history and physical examination and laboratory analysis within 14 days prior to study registration and scans to assess the status of the cancer within 42 days prior to study registration. Cardiac ejection fraction assessment had to occur within 4 weeks prior to enrollment. All women of child-bearing potential underwent serum pregnancy test within 1 week of study registration. Patients while on study underwent history and physical examinations and laboratory assessment on a weekly basis for the first two cycles of therapy (each cycle was 28 days), then every other week for Cycles 3 and 4 and then once a cycle. Assessment of disease status was performed after every two cycles for the first four cycles, and thereafter, the frequency of disease assessment was left to the discretion of the treating physician. Patients underwent assessment of cardiac ejection fraction after every cycle for the first three cycles.
Treatment
In Part I of the study, starting on Day 1 of the first cycle, patients received the two drugs once a day, at escalating dose levels as shown in Table 1. In Part II of the study, in order to assess PK interactions, patients in Cohort A started on everolimus on Day 1 of the first cycle and lapatinib was added on Day 8 of the first cycle. Patients enrolled on Cohort B started on lapatinib on Day 1 of the first cycle and everolimus was added on Day 8 of the first cycle. To avoid the confounding effect of food intake on lapatinib PK, patients were instructed to take their pills on an empty stomach, either 1 h before or 1 h after meals [11, 12].
Treatment modifications
This study used the National Cancer Institute Common Toxicity Criteria version 3.0 for toxicity and adverse event reporting. Both drugs were held for Grade 3/4 non-hematologic toxicities and for Grade 3/4 neutropenia and thrombocytopenia. If the toxicity improved to ≤Grade 1 by 14 days of discontinuation, then the patients could restart both drugs at the next lower dose. In the event of a Grade 2 non-hematologic or hematologic toxicity, both drugs were continued at the same dose or if the toxicity was unacceptable to the patient or was considered medically significant, both drugs were held for up to 14 days and once the toxicity recovered to ≤Grade 1 patients could restart both drugs at the next lower dose.
Definition of dose-limiting toxicity (DLT) and maximum tolerated dose (MTD)
Drug-related toxicities were considered DLTs if patients developed one of the following during the first cycle—Grade 3 non-hematologic toxicity, Grade 4 neutropenia lasting more than 7 days or Grade 3/4 febrile neutropenia, Grade 4 thrombocytopenia, or Grade 3 thrombocytopenia with hemorrhage. Patient missing everolimus or lapatinib for 7 days or more, due to drug-related toxicities during the first cycle, was also considered DLT.
Pharmacokinetic (PK) assessment
For determination of steady-state everolimus and lapatinib PK alone and in combination, serial blood samples were collected following the drug doses administered in the morning on Days 7 (everolimus or lapatinib alone) and 19 (everolimus + lapatinib) of Cycle 1. Patients were instructed to take their drugs on Day 7 and on Day 19 in the presence of the clinic personnel. On both Days 7 and 19, the exact time of drug administration was recorded. Separate 5-mL blood draws for everolimus and lapatinib (see below for details) were collected at the following times: at predose and 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, and 24 h post-dose. The Day 7, 24 h post-dose blood draw was to be performed before Day 8 dosing. For lapatinib sampling at each of the timepoints listed above, 5-mL venous blood was collected into a tube containing EDTA for isolation of plasma. For everolimus sampling, a separate 5-mL venous blood was collected into a tube containing EDTA and whole blood was frozen for subsequent analysis.
Pharmacokinetic (PK) analytical methods
Everolimus blood concentrations were determined in all samples in the Analytical Pharmacology Core Facility (APCF) at the City of Hope using a validated LC/MS/MS assay based on a published method [13]. Lapatinib concentrations were determined in all samples by GlaxoSmithKline (GSK) using a previously reported LC/MS/MS assay [14]. Assay methodologies for both agents are based on previously reported methods, and the limits of detection for everolimus and lapatinib are 0.25 and 1 ng/mL, respectively.
Standard non-compartmental PK analyses of everolimus and lapatinib were performed using the rule of linear trapezoids. Secondary PK parameters (C max, T max, CL/F, and AUC) were determined for each drug and in each patient, and the steady-state PK parameters on Day 7 were compared to those on Day 19.
Statistical methods
Part I of the study used a traditional “3 + 3” dosing scheme for dose escalation to determine the MTD of the combination of lapatinib and everolimus. If one of the first three patients experienced a DLT at any dose level, an additional three patients were accrued to that dose level for DLT evaluation. Dose escalation was halted when two or more out of six patients experienced DLTs at a dose level.
Upon MTD determination and completion of Part I, additional patients were enrolled in Part II of the study. Twelve patients were to be enrolled to each of the two Part II cohorts. The primary goals for Part II of the study were to evaluate (a) the steady-state pharmacokinetics (PK) of each agent when administered alone, (b) the steady-state PK of everolimus and lapatinib when given in combination, and (c) the effect of adding either lapatinib or everolimus on the steady-state PK of the other agent. For (c), the assumption was normal distributions for single-agent C max and AUC with coefficients of variation of 50 % and a two-sided 0.05 significance level t test for comparing within-patient differences with and without the other agent for either PK parameter. A sample size of 12 patients had a power of 0.93 (0.81) to detect a 50 % increase when the within-patient correlation is 0.50 (0.25). The power to detect a 100 % increase (i.e., twofold) was ample.
Results
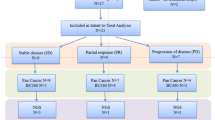
Part I
Twenty-six patients were enrolled from December 2006 to July 2008 (Table 2), and 23 were evaluable for DLTs. One patient experienced Grade 4 pneumonitis at the first dose level of 750/2.5 (lapatinib/everolimus). One out of 6 patients developed Grade 2 rash and mucositis during the first cycle at the dose level of 1,250/5 leading to both drugs being held for >7 days. Two out of 5 patients developed DLTs of diarrhea and fatigue at the dose level of 1,500/5, and both patients enrolled at the 1,250/10 dose level experienced DLT of mucositis and rash. The MTD therefore was determined to be 1,250 mg of lapatinib and 5 mg of everolimus. The most common toxicities were diarrhea, fatigue, rash, anorexia, and mucositis.
Seventeen patients stopped therapy because of progression of disease and seven for adverse events. Eleven patients had stable disease as their best response. The median number of cycles administered was 2.
Part II
Fifty-eight patients were enrolled on Part II of the study from August 2008 to July 2009 (Table 2). Twenty-nine patients were enrolled on each of the cohorts, but 4 (1 in Cohort A and 3 in Cohort B) were deemed ineligible due to poor performance status, lack of complete laboratory profile or lack of appropriate scans within specified time period prior to enrollment. One patient with thymic carcinoma is still on therapy and has received 45 cycles. Thirty-five patients stopped therapy because of progression of disease, and 12 patients stopped therapy for adverse events. Other patients stopped therapy either due to patient or physician decision or worsening symptoms without evidence of progression. A patient with thymic carcinoma achieved a PR (duration = 45+ months). A patient with breast cancer achieved an unconfirmed PR (ER+ve, PR−ve, Her2 unknown). The latter patient was on study for 7 months. Fourteen patients in Part II of the study had stable disease as their best response. The median number of cycles in all patients was 2. The common toxicities across all grades were diarrhea, hyperglycemia, rash, AST/ALT elevation, and fatigue (Table 3).
We also analyzed the number and type of patients who received more than 4 cycles of therapy as a possible indicator of clinical benefit. Thirteen patients received more than 4 cycles of therapy varying from 5 to 45+ cycles. Among these 13 patients, 2 patients had breast cancer (1 patient’s tumor ER+, Her2 unknown; 1 patient’s tumor was negative for ER, PR, Her2), 2 patients had soft tissue sarcomas, 2 patients had small bowel cancer, 2 patients with renal carcinomas, and 1 each of endometrial cancer, non-small-cell lung cancer (NSCLC), thymic carcinoma, hepatocellular carcinoma, and ovarian cancer.
Pharmacokinetics
Steady-state everolimus PK data, both alone and in combination with lapatinib, were available from 17 patients enrolled on Cohort A. Steady-state lapatinib PK data, alone and in combination with everolimus, were available in 20 patients enrolled on Cohort B. Pharmacokinetic assessment could not be performed in 21 patients because patients took the pills before coming for the PK blood draw, did not take the study pills for all of the days before the planned blood collection for PK, missed some of the PK blood draws, or came off treatment before all the planned blood draws. PK data for everolimus in whole blood and lapatinib in plasma are depicted in Figs. 1 and 2, respectively and in Table 4.
The average everolimus AUC at steady-state alone and in combination with lapatinib was 348 (95 % CI 257–438) and 427 (95 % CI 333–540) μg/L h, respectively, and the mean everolimus CL/F at steady-state was 19 (95 % CI 14–24) and 14 (95 % CI 11–18) L/h, respectively. The mean everolimus C max with and without lapatinib was 39 (95 % CI 30–48) and 37 (95 % CI 31–43) μg/L, respectively, and the average T max with and without lapatinib was 1.6 (95 % CI 1.2–2.1) and 2.3 (95 % CI 1.8–2.8) h. The mean everolimus T max was increased 44 % (p = 0.06), and the mean CL/F was decreased 25 % (p = 0.08) when the drug was given in combination with lapatinib.
The mean steady-state lapatinib C max alone and in combination with everolimus was 2,350 (95 % CI 1,890–2,930) and 2,520 (95 % CI 2,020–3,130) μg/L, respectively, and the mean lapatinib Ctrough at steady-state was 800 (95 % CI 600–1,120) and 1,060 (95 % CI 760–1,470) μg/L, respectively. The mean lapatinib AUC with and without everolimus was 3,390 (95 % CI 2,660–4,330) and 3,740 (95 % CI 2,990–4,670) μg/L h. The average lapatinib T max with and without everolimus was 3 (95 % CI 0.5–8) and 4 (95 % CI 0–24) h. Differences in steady-state lapatinib PK determined with or without everolimus co-administration were not statistically significant.
Discussion
Many preclinical studies have suggested that the PI3K/Akt/mTOR pathway plays a role in both primary and secondary resistance to Her pathway inhibitors [8–10, 15]. However, it is important to recognize that other mechanisms, such as activation of the IGFR pathway, may also lead to resistance to these agents, and therefore, addition of mTOR inhibitors to Her inhibitors may benefit only select patients [16]. Nonetheless, the interest generated by preclinical studies of dual Her and mTOR inhibition formed the basis of the current Phase I study. Our study demonstrates that lapatinib and everolimus can be combined safely, but the dose of everolimus, when combined with lapatinib, has to be reduced to 5 mg daily from its single-agent dose of 10 mg daily. The dose of lapatinib is the same (1,250 mg po daily) as that approved for the combination of lapatinib and capecitabine in Her2-positive breast cancer patients. The main dose-limiting toxicities encountered were gastrointestinal (diarrhea and mucositis) and skin (rash) as well as fatigue.
Prior to the conduct of this study, there were some concerns regarding the potential side effects of the combination, particularly since both drugs are metabolized through the P450 enzyme system, particularly CYP3A4, and are P-glycoprotein substrates. In this regard, a Phase I/II trial of everolimus and imatinib revealed that imatinib increased levels of everolimus (mean AUC by 3.7-fold, C max by 2.2-fold), but everolimus did not affect levels of imatinib [17]. In addition, there are certain adverse effects, such as diarrhea and rash, which are common to both drugs. Despite these concerns, the combination was found to be well tolerated. No episode of cardiac dysfunction occurred in any of the treated patients. The adverse effects observed are similar to those expected from each of these two drugs individually. However, only nine patients in this study received the combination for more than 4 cycles at MTD, and some required dose reduction in one or both drugs. Therefore, patients who attain a response and are on the drugs for prolonged periods of time will need to be watched for cumulative side effects and may need further dose reductions.
The current study also included a comprehensive evaluation of the effects of each drug on the other drug’s PK, including the possible inductive and inhibitive effects. To that end, a clinical trial design was selected that allowed us to evaluate the steady-state PK of the two drugs as single agents and in combination, using each patient as their own control. Patients were required to be fasting when they arrived on days of PK blood draws, could not have missed any dose during the first week of the first cycle, and required complete sample collections. The systemic exposure of lapatinib, as measured by AUC (0–infinity), when given in combination with everolimus, was essentially unchanged compared to the single-agent results. However, the exposure of everolimus was increased by an average of 25 % when co-administered with lapatinib. Interestingly, the effect of lapatinib on everolimus disposition may be related to an effect on the kinetics of drug absorption, as demonstrated by a 44 % increase in the T max. However, interference with everolimus elimination can also not be ruled out as a mechanism of a possible drug–drug interaction. Regardless, the PK differences observed when everolimus was given in combination with lapatinib did not reach statistical significance, possibly due to the high degree of inter- and intra-subject variability. Our study suggests that a 50 % difference in PK of either drug is unlikely. To detect a smaller difference of 25 %, approximately 43 patients per cohort would be necessary. A larger study would be required to determine the precise magnitude and mechanism of the effect of lapatinib on the PK of everolimus.
In a Phase I/II study of everolimus and trastuzumab in patients with breast cancer, the starting dose of everolimus was 10 mg daily [18]. At this dose, the incidences of common toxicities were similar to those in the current trial. However, the incidence of rash was higher in the current study, probably because of the concomitant use of everolimus. It is possible that a higher dose of everolimus can be delivered when combined with a monoclonal antibody as compared to a combination with another tyrosine kinase inhibitor. When everolimus has been combined with epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors, it has been used at the dose of 5 mg daily [19–21]. In the Phase I trial with gefitinib and everolimus, there was heterogeneity in both everolimus and gefitinib pharmacokinetics [19]. However, the number of patients who underwent pharmacokinetic analyses was small. In a Phase I study of erlotinib and everolimus, the pharmacokinetics of erlotinib with or without everolimus were similar [20]. However, systemic exposure to everolimus was 17 % higher with erlotinib than without.
Stable disease of at least 4 months and PRs (total = 17 %) were observed with this combination. The longest progression-free interval—45+ months—was seen in the only patient with thymic carcinoma enrolled on the trial. There is another case report of clinical benefit with erlotinib in a thymic carcinoma patient [22]. In addition, in a Phase I study of the mTOR inhibitor temsirolimus with bevacizumab and liposomal doxorubicin, 4 of 7 patients with thymic carcinoma had prolonged stable disease or partial response [23]. Furthermore, a recent study suggests that six of 10 patients with this type of tumor treated with an mTOR inhibitor-based combination regimen achieved stable disease ≥12 months or a PR [24].
One of our patients who attained an unconfirmed PR (duration = 7 months) had ER-positive breast cancer (Her2 status of the tumor was not known). Recently, everolimus combined with exemestane prolonged progression-free survival in ER-positive patients with breast cancer compared to exemestane alone (6.9 vs. 2.8 months) [7]. In our study, a second patient who had triple-negative tumor also remained stable for 6 months. Preclinical studies suggest that triple-negative breast cancer may be susceptible to mTOR inhibition [24]. Interestingly, the triple-negative breast cancer cell lines sensitive to everolimus express EGFR, suggesting that the addition of an EGFR inhibitor to everolimus in this patient population maybe beneficial [25]. An ongoing study, NCT01272141, is evaluating the combination of everolimus and lapatinib in triple-negative breast cancer. Altogether, 11 patients with diverse tumors showed stable disease of at least 4 months, in addition to two patients mentioned above who showed over 30 % regression.
In conclusion, lapatinib and everolimus can be combined safely at doses of 1,250 mg daily and 5 mg daily, respectively. The common dose-limiting toxicities from the combination are diarrhea, rash, mucositis, and fatigue. The clinical utility of this combination will be defined by ongoing clinical trials (NCT01272141 (triple-negative breast cancer), NCT01283789 (her2-positive breast cancer), and NCT01499160 (endocrine-resistant breast cancer)). Additional trials may benefit from selecting patients who are her2+ and analyzing tumors for aberrations in the PIK3CA/Akt/mTOR pathways [26, 27] since correlation of pathway abnormalities with response remains to be established.
References
Citri A, Yarden Y (2006) EGF-ERBB signalling: towards the systems level. Nat Rev Mol Cell Biol 7(7):505–516
Cameron DA, Stein S (2008) Drug insight: intracellular inhibitors of HER2—clinical development of lapatinib in breast cancer. Nat Clin Pract Oncol 5(9):512–520
Geyer CE, Forster J, Lindquist D et al (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355(26):2733–2743
Liu P, Cheng H, Roberts TM, Zhao JJ (2009) Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov 8(8):627–644
Motzer RJ, Escudier B, Oudard S et al (2008) Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet 372(9637):449–456
Yao JC, Shah MH, Ito T et al (2011) Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 364(6):514–523
Baselga J, Campone M, Piccart M et al (2012) Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366(6):520–529
La MS, Galetti M, Alfieri RR et al (2009) Everolimus restores gefitinib sensitivity in resistant non-small cell lung cancer cell lines. Biochem Pharmacol 78(5):460–468
Miller TW, Forbes JT, Shah C et al (2009) Inhibition of mammalian target of rapamycin is required for optimal antitumor effect of HER2 inhibitors against HER2-overexpressing cancer cells. Clin Cancer Res 15(23):7266–7276
Buck E, Eyzaguirre A, Brown E et al (2006) Rapamycin synergizes with the epidermal growth factor receptor inhibitor erlotinib in non-small-cell lung, pancreatic, colon, and breast tumors. Mol Cancer Ther 5(11):2676–2684
Koch KM, Reddy NJ, Cohen RB et al (2009) Effects of food on the relative bioavailability of lapatinib in cancer patients. J Clin Oncol 27(8):1191–1196
Ratain MJ, Cohen EE (2007) The value meal: how to save $1,700 per month or more on lapatinib. J Clin Oncol 25(23):3397–3398
Streit F, Armstrong VW, Oellerich M (2002) Rapid liquid chromatography-tandem mass spectrometry routine method for simultaneous determination of sirolimus, everolimus, tacrolimus, and cyclosporin A in whole blood. Clin Chem 48(6 Pt 1):955–958
Hsieh S, Tobien T, Koch K, Dunn J (2004) Increasing throughput of parallel on-line extraction liquid chromatography/electrospray ionization tandem mass spectrometry system for GLP quantitative bioanalysis in drug development. Rapid Commun Mass Spectrom 18(3):285–292
Goudar RK, Shi Q, Hjelmeland MD et al (2005) Combination therapy of inhibitors of epidermal growth factor receptor/vascular endothelial growth factor receptor 2 (AEE788) and the mammalian target of rapamycin (RAD001) offers improved glioblastoma tumor growth inhibition. Mol Cancer Ther 4(1):101–112
Morgillo F, Kim WY, Kim ES, Ciardiello F, Hong WK, Lee HY (2007) Implication of the insulin-like growth factor-IR pathway in the resistance of non-small cell lung cancer cells to treatment with gefitinib. Clin Cancer Res 13(9):2795–2803
Schoffski P, Reichardt P, Blay JY et al (2010) A phase I–II study of everolimus (RAD001) in combination with imatinib in patients with imatinib-resistant gastrointestinal stromal tumors. Ann Oncol 21(10):1990–1998
Morrow PK, Wulf GM, Ensor J et al (2011) Phase I/II study of trastuzumab in combination with everolimus (RAD001) in patients with HER2-overexpressing metastatic breast cancer who progressed on trastuzumab-based therapy. J Clin Oncol 29(23):3126–3132
Milton DT, Riely GJ, Azzoli CG et al (2007) Phase 1 trial of everolimus and gefitinib in patients with advanced nonsmall-cell lung cancer. Cancer 110(3):599–605
Bullock KE, Petros WP, Younis I et al (2011) A phase I study of bevacizumab (B) in combination with everolimus (E) and erlotinib (E) in advanced cancer (BEE). Cancer Chemother Pharmacol 67(2):465–474
Riely GJ, Kris MG, Zhao B et al (2007) Prospective assessment of discontinuation and reinitiation of erlotinib or gefitinib in patients with acquired resistance to erlotinib or gefitinib followed by the addition of everolimus. Clin Cancer Res 13(17):5150–5155
Christodoulou C, Murray S, Dahabreh J et al (2008) Response of malignant thymoma to erlotinib. Ann Oncol 19(7):1361–1362
Moroney J, Fu S, Moulder S et al (2012) Phase I study of antiangiogenic antibody bevacizumab and the mTOR/hypoxia-inducible factor inhibitor temsirolimus combined with liposomal doxorubicin. Clin Cancer Res 18(20):5796–5805
Wheeler J, Hong D, Swisher SG et al (2013) Thymoma patients treated in a phase I clinic at MD Anderson Cancer Center: responses to mTOR inhibitors and molecular analyses. Oncotarget 4(6):890–898
Yunokawa M, Koizumi F, Kitamura Y et al (2012) Efficacy of everolimus, a novel mTOR inhibitor, against basal-like triple-negative breast cancer cells. Cancer Sci 103(9):1665–1671
Janku F, Wheler JJ, Westin SN et al (2012) Pi3K/AKT/mTOR inhibitors in patients with breast and gynecologic malignancies harboring PIK3CA mutations. J Clin Oncol 30:777–782
Janku F, Wheler JJ, Naing A et al (2013) PIK3CA mutation H1047R is associated with response to PI3K/AKT/mTOR signaling pathway inhibitors in early-phase clinical trials. Cancer Res 73:276–284
Acknowledgments
This work was supported in part by the following Public Health Service Cooperative Agreement grant numbers awarded by the National Cancer Institute, National Institutes of Health, Department of Health and Human Services: CA32102, CA38926, CA46368, CA14028, CA27057, CA46441, CA46136, CA58882, CA20319, CA42777, and in part by GlaxoSmithKline and Novartis. It was also supported in part by the Cancer Clinical Investigator Team Leadership Award awarded by the National Cancer Institute through a supplement to P30CA022453-30S1.
Conflict of interest
Shirish M. Gadgeel: Research Funding from GlaxoSmithKline and Novartis. Razelle Kurzrock: Honorarium received from Pfizer. Research Funding from: GlaxoSmithKline, Novartis, Roche and Pfizer. Patricia LoRusso: Research funding from GlaxoSmithKline and Novartis. None of the other authors have any financial relationship.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical Trials.gov Identifier—NCT00352443.
Rights and permissions
About this article
Cite this article
Gadgeel, S.M., Lew, D.L., Synold, T.W. et al. Phase I study evaluating the combination of lapatinib (a Her2/Neu and EGFR inhibitor) and everolimus (an mTOR inhibitor) in patients with advanced cancers: South West Oncology Group (SWOG) Study S0528. Cancer Chemother Pharmacol 72, 1089–1096 (2013). https://doi.org/10.1007/s00280-013-2297-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2297-4