Abstract
Purpose
Paclitaxel, a cytotoxic agent metabolized by cytochrome P450 hepatic enzymes, is active for the treatment of human immunodeficiency (HIV) associated Kaposi’s sarcoma. Protease inhibitors are commonly used to treat HIV infection and are known to inhibit cytochrome P450. We sought to determine whether protease inhibitors alter the pharmacokinetics of paclitaxel.
Methods
Patients with advanced HIV-associated KS received paclitaxel (100 mg/m2) by intravenous infusion over 3 h, and plasma samples were collected to measure paclitaxel concentration. The area under the curve (AUC) was calculated using a combination of the log and linear trapezoidal rule, and clearance was calculated as the dose/AUC. Pharmacokinetics were compared with respect to antiretroviral therapy and toxicity,
Results
Thirty-four patients received paclitaxel, of whom 20 had no prior paclitaxel therapy and were assessable for response. Twenty-seven had pharmacokinetic studies performed. Paclitaxel exposure was higher in patients taking protease inhibitors compared to those who were not taking protease inhibitors. The increased exposure did not correlate with efficacy or toxicity. Of the 20 patients assessable for response, 6 (30%) had an objective response and median progression-free survival was 7.8 months (95% confidence interval, 5.6, 21.0 months).
Conclusion
Despite higher exposure to paclitaxel, patients on protease inhibitors did not experience enhanced toxicity or efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risk of Kaposi’s sarcoma (KS) is markedly increased in individuals infected with the human immunodeficiency virus (HIV) compared with the general population [1]. KS requires infection with human herpes virus 8 (HHV-8), [2, 3] also known as the KS-associated herpesvirus (KSHV), and co-infection with HIV promotes KS development in HHV-8-infected individuals by impairing immune responses to HHV-8 and by inducing the production of cytokines and growth factors that promote vascular proliferation [4–8].
It became common clinical practice beginning in the 1990s to use potent antiretroviral agents in combination in order to maximally suppress HIV viral load, a strategy widely known as “highly active antiretroviral therapy” (HAART) [9]. This strategy led to marked reduction in morbidity and mortality for patients with advanced HIV infection, [10] and to a marked decrease in the incidence of KS where HAART was widely available [11]. Nevertheless, KS still occurs in up to 15% of patients with HIV infection and can produce substantial morbidity due to disfiguring skin lesions, edema, or visceral involvement that may require palliation with cytotoxic chemotherapeutic agents.
Of the commonly used antiretroviral agents, the protease inhibitors are among the most potent and are often an integral component HAART [12, 13]. There are currently 10 commercially available protease inhibitors, which include agents such as saquinavir, indinavir, ritonavir, and nelfinavir that have been available for over a decade. All protease inhibitors are metabolized by enzymes that are part of the cytochrome P450 system. Protease inhibitors may either inhibit or induce certain of these enzymes and alter metabolism of other drugs that are metabolized by this pathway [14]. Thus, the potential exists for interactions between protease inhibitors and many other drugs, including paclitaxel [15, 16].
Paclitaxel is a cytotoxic agent that is approved for the treatment of advanced, KS [17–20]. Paclitaxel is extensively metabolized, predominantly by the cytochrome P450 CYP2C8, CYP3A4, and CYP3A5, to inactive metabolites [21] and is a substrate for ABCB1 [22]. The pharmacokinetics of paclitaxel are non-linear with saturable elimination [23, 24]. Pharmacodynamic analyses have shown hematologic and non-hematologic toxicity, response, and survival to each correlate better with parameters of paclitaxel exposure (e.g., duration of plasma concentrations exceeding 0.05 or 0.1 μM) than with the administered dosage [23, 25–29]. Limited data are available regarding the drug interaction potential with protease inhibitors and chemotherapy and have been mixed [30, 31].
The Eastern Cooperative Oncology Group (ECOG) and the AIDS Malignancy Consortium (AMC) jointly performed a pilot trial to determine whether commonly used protease inhibitors could alter the pharmacokinetics of paclitaxel. We designed the trial to determine whether concurrent use of protease inhibitors would substantially increase the paclitaxel AUC, which has been linked with pharmacodynamic outcomes, compared with historical data evaluating paclitaxel in other cancer types.
Methods
Eligibility criteria
All patients were required to have a serologic diagnosis of HIV infection and biopsy-proven, measurable, symptomatic KS with one of the following indications for chemotherapy: progressive cutaneous disease, symptomatic oropharyngeal or conjunctival lesions, visceral involvement, or symptomatic lymphedema. Other requirements included age ≥18 years, an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0, 1, or 2, and adequate hematologic (absolute neutrophil count [ANC] of ≥1,000/mm3, and platelet count ≥50,000/mm3), renal (creatinine <1.5 mg or creatinine clearance >60 cc/min), and hepatic function (SGOT <2.5× the upper limit of normal [ULN] and bilirubin <1.5× the ULN). Other requirements included no grade 2 or greater peripheral neuropathy, active untreated infection, prior or concomitant malignancy (other than curatively treated in situ carcinoma of the cervix or basal/squamous cell skin carcinoma) or sensitivity to E.coli derived proteins. Prior radiation therapy could not have been delivered to marker lesions used to assess response and had to be discontinued ≥7 days prior to registration. All patients provided written informed consent. The protocol and consent were reviewed and approved by the institutional review boards at each participating institution.
When the trial was initiated, patients were required to have had no prior paclitaxel treatment prior to registration. Because of slow accrual, the trial was amended to allow patients who were already receiving paclitaxel to enroll and to receive one cycle of paclitaxel therapy with pharmacokinetic analysis. Patients who had received prior paclitaxel were eligible if they had stable or responding disease on paclitaxel, had satisfactorily recovered from the toxic effects of the previous treatment cycle (or a minimum 2 week interval had passed, whichever was longer); all other eligibility criteria were met, and the treating physician agreed to prescribe the dose of paclitaxel specified in the trial. Only patients who had no prior paclitaxel therapy were assessable for efficacy.
Pretreatment and on treatment evaluation
Before study entry, all patients underwent an evaluation consisting of a complete history and physical examination, CD4 and CD8 lymphocyte counts, chest X-ray (CXR), and measurement of KS lesions by physical examination. KS tumor assessments were performed as described previously [32]. Lesion counts and measurements were repeated after every two cycles of therapy (4 weeks), CD4 and CD8 counts were repeated every 3 months, and chest X-ray was repeated every 6 months if initially normal, or every 3 months if there was evidence of pulmonary KS.
Treatment
Patients were permitted to be on any of the commercially available antiretroviral agents; zidovudine treatment was allowed if patients were on a stable dose and schedule for at least 1 month. Paclitaxel was administered at a dose of 100 mg/m2 infused intravenously (IV) over 3 h every 14 days. No dose escalation was allowed. The patient’s actual weight was used to calculate body surface area. All patients were premedicated with diphenhydramine 50 mg and cimetidine 300 mg IV (or other H2 receptor antagonist) given IV 30–60 min prior to the infusion and dexamethasone 20 mg IV or orally immediately prior to the infusion. Treatment was repeated every 2 weeks if the neutrophil count was at least 1,000/mm3, platelets at least 100,000/mm3, and the patient had adequately recovered from toxicity. Treatment continued until the development of progressive disease or prohibitive toxicity. Dose and schedule modifications were specified for hematologic and hepatic toxicity and other ≥grade 3 toxicity. Patients who had received prior paclitaxel received only one cycle of paclitaxel as part of the study and were then removed from the protocol.
Supportive care
Granulocyte colony stimulating factor (G-CSF) was used if there was persistent ≥grade 3–4 neutropenia on day 14 preventing the administration of paclitaxel on schedule or a neutrophil count of <500/mm3 and fever or localized infection requiring antibiotic use. Erythropoietin could be used at the discretion of the treating physician in patients with anemia. All patients with CD4 count <200 cells/microliter or <15% CD4 lymphocytes were required to receive Pneumocystis jiroveci pneumonia (PCP) prophylaxis.
No medications were excluded due to their drug interaction potential.
Pharmacokinetic sampling and evaluation
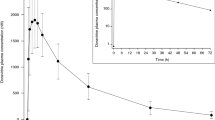
Plasma samples were collected for pharmacokinetic analysis during cycle 1 at the following time points: prior to administration of the first dose of paclitaxel, at 0.5, 1, 2, 2.5, and 2.8 h during the infusion, and at 0.08, 0.5, 1, 2, 5 and 21 h after the end of the infusion. Paclitaxel was quantitated over the range of 0.02 to 10 μM by HPLC with ultraviolet detection [33].
Individual plasma concentrations of paclitaxel were analyzed using non-compartmental methods as implemented in the computer software program WinNonlin version 5.2 (Pharsight, Inc., Mountain View, CA, USA). The maximum plasma concentration (C max) was the observed value. The area under the plasma concentration–time curve (AUC) value was calculated to the last quantifiable sample (AUClast) by use of the linear trapezoidal rule. The AUC values were extrapolated to infinity (AUCinf) by dividing the last quantifiable concentration by the terminal disposition rate constant (λ z ), which was determined from the slope of the terminal phase of the concentration–time profile. The clearance (Cl) was calculated by dividing the dose administered by AUCinf. The duration spent at a paclitaxel concentration >0.05 μM was calculated. If the percent AUC extrapolated was >25% or the r 2 on the λ z was <0.9, the AUCinf, Cl, and duration spent at a paclitaxel concentration >0.05 μM were not reported.
Response criteria
Response was assessed only in patients who had no prior paclitaxel before enrollment and coded as complete response, partial response, stable disease, and progressive disease using criteria that have been previously described [34]. Tumor measurements and lesion counts were performed by the treating physician, and the measurements and response as coded by the treating physician were recorded in the case report form. Case report forms were reviewed centrally by ECOG data management staff to assure that the coded response was consistent with the protocol-defined response definitions.
Statistical analysis
Paclitaxel pharmacokinetic variables were summarized using descriptive statistics. Pharmacokinetic measurements were compared with respect to antiretroviral therapy (no protease inhibitor vs. protease inhibitor) and toxicity grade (grade 3–4 granulocytopenia toxicity yes vs. no) using the Wilcoxon rank-sum test. Two-sided tests were used for significance testing with the a priori level of significance set at P < 0.05. The Kaplan–Meier method was used to estimate the distribution of overall survival and progression-free survival.
Results
Patient characteristics
A total of 34 patients were accrued and treated between June 19, 1997 and April 1, 2002. Of these, 27 had evaluable pharmacokinetic data (Group A), and 20 eligible patients had no prior paclitaxel therapy and were assessable for both efficacy and toxicity (Group B). Of the 34 patients enrolled and treated, seven did not meet all eligibility criteria because of missing data: baseline tumor measurements (n = 1), documentation of KS diagnosis (n = 2), documentation of HIV infection (n = 3), or baseline measurements and documentation of HIV infection (n = 1). The characteristics of these two groups are shown in Table 1. The median age was approximately 39 years, most were male, the median ECOG PS was 1, and the median CD4 count was 122/uL in Group A.
Treatment information
For the 20 patients who received paclitaxel as first-line therapy (Group B), a total of 179 treatment cycles were administered, and the median number of completed cycles was 5 (range 1–43). Reasons for discontinuation of therapy included progressive disease in 4 patients (20%), patient withdrawal in 4 patients (20%), toxicity in 3 patients (15%), treatment completion in 2 patients (10%), and a variety of other reasons in 7 patients (35%).
Pharmacokinetic analysis
Pharmacokinetic studies were performed in 27 patients. Sixteen patients were taking protease inhibitors [nelfinavir (n = 6), indinavir (n = 3), or multiple inhibitors (n = 7)] and 11 patients were not taking protease inhibitors. Pharmacokinetic variables are listed in Table 2. There was a trend for paclitaxel maximum concentration (C max) to be elevated in the 16 patients taking one or more protease inhibitors compared to the 11 patients not taking protease inhibitors (1.47 ± 0.68 μM vs. 1.01 ± 0.34 μM; P = 0.11; Wilcoxon t test). However, the paclitaxel area under the curve (AUCinf), which was evaluable in 21 patients, was significantly higher in the 15 patients taking protease inhibitors compared to the 6 patients not taking protease inhibitors (5.5 ± 2.2 μM h vs. 2.9 ± 0.7 μM h; P = 0.016; Wilcoxon t test). Yet, there was no difference in the duration spent at a paclitaxel concentration >0.05 μM (19.0 (3.0–27.8) h vs 6.7 (3.0–22.7) h; P = 0.97). Patients with higher paclitaxel exposure did not experience more significant granulocytopenia (C max P = 0.96; AUCinf P = 0.83; Time > C0.5 μM P = 0.09; Wilcoxon t test).
Objective response, progression-free survival, and survival
Of the 20 evaluable patients who received paclitaxel for the first time, the best response to therapy was a partial response in 6 patients (30, 95% confidence intervals 12, 54%), stable disease (SD) in 10 patients (50%), and progressive disease in 2 patients (10%). Two patients (10%) could not be evaluated because they lacked baseline tumor measurements. Median progression-free survival was 7.8 months (95% CI 5.6, 21.0 months), and median overall survival had not been reached after a median follow-up of 50 months in the 13 surviving patients; the 3-year survival rate was 67% (95% CI 45, 89%).
Toxicity
Toxicity data for 20 patients who received paclitaxel as first-line therapy is shown in Table 3. The toxicity profile for the 27 patients who underwent pharmacokinetic studies was similar (data not shown). The most common treatment-related toxicities of grade 3 or higher occurring in more than 10% of patients included granulocytopenia (40%), infection (15%), and anemia (15%).
Discussion
We evaluated the pharmacokinetics and pharmacodynamics of paclitaxel when used in combination with one or more protease inhibitors in 16 patients with HIV-associated KS and compared this to 11 patients who were not on a protease inhibitor. Paclitaxel was given at a dose of 100 mg/m2 as a 3-hour intravenous infusion. The protease inhibitors used included indinavir, nelfinavir, or combinations of these agents at recommended doses and schedules. There was an increase in paclitaxel total exposure (AUCinf) in patients on the protease inhibitors but no significant changes in maximal exposure or duration above a concentration threshold (Time > C0.5 μM). However, other drugs that alter CYP3A4 or CYP2C9 activity were not controlled for and therefore could limit our findings. In this study, the alterations in pharmacokinetics were not associated with increased toxicity. In addition, the efficacy and toxicity profile of paclitaxel in patients with HIV-associated KS was similar to previous studies performed in the pre-HAART era [17–19]. As HIV-infected individuals are living longer in the HAART era, non-AIDS defining cancers are being diagnosed more commonly [35]. For many of these cancers, such as lung and head/neck cancer that are common in HIV-infected patients, paclitaxel is frequently used. Thus, the relevance of understanding the potential pharmacokinetic interactions between paclitaxel and protease inhibitors extends beyond the treatment of KS.
Although regression of HIV-associated KS has been reported after initiation of HAART without additional cytotoxic therapy, and HAART is an essential component of therapy for such patients, chemotherapy has an important and independent palliative role. For example, Martin-Carbonero and colleagues randomly assigned 28 patients with HIV-associated KS to receive HAART alone or in combination with liposomal doxorubicin; after 48 weeks of therapy, patients receiving liposomal doxorubicin had a significantly better response rate (76% vs. 20%) [36]. Clearly, systemic chemotherapy still plays a major role in the treatment of advanced, symptomatic KS.
The interaction between antiretroviral agents and cytotoxic agents has been evaluated in a number of trials. Tulpule and colleagues reported a phase II trial of 107 male patients with advanced HIV-related KS treated with paclitaxel (100 mg/m2 intravenously over 3 h every 2 weeks), of whom 77% received protease inhibitors. No differences in the incidence or severity of toxicity in the patients receiving protease inhibitors compared to those who did not were identified. No pharmacokinetic studies were performed; however, [17] Fumagilli and colleagues reported no effect of protease inhibitors on the pharmacokinetics of liposomal daunorubicin [37]. Kappelhoff and colleagues reported no difference in the pharmacokinetics of a single patient treated with paclitaxel and nevirapine, a non-nucleoside reverse transcriptase inhibitor, compared with historical data [38]. Nanan Panday and colleagues evaluated the pharmacokinetics of paclitaxel given for several cycles with different antiretrovirals (indinavir, ritonavir, saquinavir, and nevirapine) given in each cycle in a single patient, and found no difference in the pharmacokinetics of paclitaxel or the antiretroviral drugs in this individual compared with historical pharmacokinetic data [30]. Ratner and colleagues evaluated the pharmacokinetics of 29 patients receiving cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) chemotherapy with HAART [39]. Although clearance of cyclophosphamide was reduced 1.5-fold compared to historical controls, excessive hematologic toxicity was not observed. No significant effects on doxorubicin clearance were seen. Although these studies point out the paucity of data on the pharmacokinetic interaction between antiretroviral drugs and cytotoxic agents, they are also consistent with our finding that there was no clinically significant drug–drug interaction.
In conclusion, there appeared to be a detectable pharmacokinetic interaction between paclitaxel and protease inhibitors in this trial. However, there was no evidence for increased toxicity. There is therefore no justification for empiric dose adjustment of paclitaxel in patients with HIV-related KS who are receiving the protease inhibitor therapy utilized by patients treated in this trial.
References
Biggar RJ, Rosenberg PS, Cote T (1996) Kaposi’s sarcoma, non-Hodgkin’s lymphoma following the diagnosis of AIDS. Multistate AIDS/cancer match study group. Int J Cancer 68:754–758
Moore PS, Chang Y (1995) Detection of herpesvirus-like DNA sequences in Kaposi’s sarcoma in patients with and without HIV infection. N Engl J Med 332:1181–1185
Chang Y, Cesarman E, Pessin MS et al (1994) Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science 266:1865–1869
Masood R, Cai J, Zheng T, Smith DL, Naidu Y, Gill PS (1997) Vascular endothelial growth factor/vascular permeability factor is an autocrine growth factor for AIDS-Kaposi sarcoma. Proc Natl Acad Sci USA 94:979–984
Montaner S (2007) Akt/TSC/mTOR activation by the KSHV G protein-coupled receptor: emerging insights into the molecular oncogenesis and treatment of Kaposi’s sarcoma. Cell Cycle 6:438–443
Zeng Y, Zhang X, Huang Z et al (2007) Intracellular Tat of human immunodeficiency virus type 1 activates lytic cycle replication of Kaposi’s sarcoma-associated herpesvirus: role of JAK/STAT signaling. J Virol 81:2401–2417
Aoki Y, Tosato G (2004) HIV-1 Tat enhances Kaposi sarcoma-associated herpesvirus (KSHV) infectivity. Blood 104:810–814
Deregibus MC, Cantaluppi V, Doublier S et al (2002) HIV-1-Tat protein activates phosphatidylinositol 3-kinase/AKT-dependent survival pathways in Kaposi’s sarcoma cells. J Biol Chem 277:25195–25202
Ho DD (1995) Time to hit HIV, early and hard. N Engl J Med 333:450–451
Palella FJ Jr, Delaney KM, Moorman AC et al (1998) Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med 338:853–860
Jacobson LP, Yamashita TE, Detels R et al (1999) Impact of potent antiretroviral therapy on the incidence of Kaposi’s sarcoma and non-Hodgkin’s lymphomas among HIV-1-infected individuals. Multicenter AIDS cohort study. J Acquir Immune Defic Syndr 21(Suppl 1):S34–S41
Flexner C (1998) HIV-protease inhibitors. N Engl J Med 338:1281–1292
Mastrolorenzo A, Rusconi S, Scozzafava A, Barbaro G, Supuran CT (2007) Inhibitors of HIV-1 protease: current state of the art 10 years after their introduction. From antiretroviral drugs to antifungal, antibacterial and antitumor agents based on aspartic protease inhibitors. Curr Med Chem 14:2734–2748
Dixit V, Hariparsad N, Li F, Desai P, Thummel KE, Unadkat JD (2007) Cytochrome P450 enzymes and transporters induced by anti-human immunodeficiency virus protease inhibitors in human hepatocytes: implications for predicting clinical drug interactions. Drug Metab Dispos 35:1853–1859
Jackson A, Taylor S, Boffito M (2004) Pharmacokinetics and pharmacodynamics of drug interactions involving HIV-1 protease inhibitors. AIDS Rev 6:208–217
Malaty LI, Kuper JJ (1999) Drug interactions of HIV protease inhibitors. Drug Saf 20:147–169
Tulpule A, Groopman J, Saville MW et al (2002) Multicenter trial of low-dose paclitaxel in patients with advanced AIDS-related Kaposi sarcoma. Cancer 95:147–154
Gill PS, Tulpule A, Espina BM et al (1999) Paclitaxel is safe and effective in the treatment of advanced AIDS-related Kaposi’s sarcoma. J Clin Oncol 17:1876–1883
Welles L, Saville MW, Lietzau J et al (1998) Phase II trial with dose titration of paclitaxel for the therapy of human immunodeficiency virus-associated Kaposi’s sarcoma. J Clin Oncol 16:1112–1121
Saville MW, Lietzau J, Pluda JM et al (1995) Treatment of HIV-associated Kaposi’s sarcoma with paclitaxel. Lancet 346:26–28
Harris JW, Rahman A, Kim BR, Guengerich FP, Collins JM (1994) Metabolism of taxol by human hepatic microsomes and liver slices: participation of cytochrome P450 3A4 and an unknown P450 enzyme. Cancer Res 54:4026–4035
Sparreboom A, van Asperen J, Mayer U et al (1997) Limited oral bioavailability and active epithelial excretion of paclitaxel (Taxol) caused by P-glycoprotein in the intestine. Proc Natl Acad Sci USA 94:2031–2035
Sonnichsen DS, Relling MV (1994) Clinical pharmacokinetics of paclitaxel. Clin Pharmacokinet 27:256–269
Sonnichsen DS, Hurwitz CA, Pratt CB, Shuster JJ, Relling MV (1994) Saturable pharmacokinetics and paclitaxel pharmacodynamics in children with solid tumors. J Clin Oncol 12:532–538
Mielke S, Sparreboom A, Steinberg SM et al (2005) Association of Paclitaxel pharmacokinetics with the development of peripheral neuropathy in patients with advanced cancer. Clin Cancer Res 11:4843–4850
Gianni L, Kearns CM, Giani A et al (1995) Nonlinear pharmacokinetics and metabolism of paclitaxel and its pharmacokinetic/pharmacodynamic relationships in humans. J Clin Oncol 13:180–190
Mielke S, Sparreboom A, Behringer D, Mross K (2005) Paclitaxel pharmacokinetics and response to chemotherapy in patients with advanced cancer treated with a weekly regimen. Anticancer Res 25:4423–4427
Huizing MT, Giaccone G, van Warmerdam LJ et al (1997) Pharmacokinetics of paclitaxel and carboplatin in a dose-escalating and dose-sequencing study in patients with non-small-cell lung cancer. The European cancer centre. J Clin Oncol 15:317–329
Sparreboom A, Verweij J (2003) Paclitaxel pharmacokinetics, threshold models, and dosing strategies. J Clin Oncol 21:2803–2804 author reply 2805-6
Nannan Panday VR, Hoetelmans RM, van Heeswijk RP et al (1999) Paclitaxel in the treatment of human immunodeficiency virus 1-associated Kaposi’s sarcoma–drug-drug interactions with protease inhibitors and a nonnucleoside reverse transcriptase inhibitor: a case report study. Cancer Chemother Pharmacol 43:516–519
Duchin K, Sun J, Tan M, Ilaw M, Cabriales S, Espina BM, East D, Tulpule A, Gill PS 1997 Pharmacokinetics of low-dose Paxene (paclitaxel) in patients with refractory or relapsed AIDS-related Kaposi’s sarcoma. Proc Am Soc Clin. 15 Abstract 235
Cianfrocca M, Cooley TP, Lee JY et al (2002) Matrix metalloproteinase inhibitor COL-3 in the treatment of AIDS-related Kaposi’s sarcoma: a phase I AIDS malignancy consortium study. J Clin Oncol 20:153–159
Sparreboom A, de Bruijn P, Nooter K, Loos WJ, Stoter G, Verweij J (1998) Determination of paclitaxel in human plasma using single solvent extraction prior to isocratic reversed-phase high-performance liquid chromatography with ultraviolet detection. J Chromatogr B Biomed Sci Appl 705:159–164
Krown SE, Metroka C, Wernz JC (1989) Kaposi’s sarcoma in the acquired immune deficiency syndrome: a proposal for uniform evaluation, response, and staging criteria. AIDS clinical trials group oncology committee. J Clin Oncol 7:1201–1207
Pantanowitz L, Schlecht HP, Dezube BJ (2006) The growing problem of non-AIDS-defining malignancies in HIV. Curr Opin Oncol 18:469–478
Martin-Carbonero L, Barrios A, Saballs P et al (2004) Pegylated liposomal doxorubicin plus highly active antiretroviral therapy versus highly active antiretroviral therapy alone in HIV patients with Kaposi’s sarcoma. Aids 18:1737–1740
Fumagalli L, Zucchetti M, Parisi I et al (2000) The pharmacokinetics of liposomal encapsulated daunorubicin are not modified by HAART in patients with HIV-associated Kaposi’s sarcoma. Cancer Chemother Pharmacol 45:495–501
Kappelhoff BS, Huitema AD, Mairuhu AT, Schellens JH, Beijnen JH (2005) No pharmacokinetic drug-drug interaction between nevirapine and paclitaxel. Anticancer Drugs 16:627–630
Ratner L, Lee J, Tang S et al (2001) Chemotherapy for human immunodeficiency virus-associated non-hodgkin’s lymphoma in combination with highly active antiretroviral therapy. J Clin Oncol 19:2171–2178
Acknowledgments
The authors thank Dr. Fayez Hamzeh for performing the pharmacokinetic analysis when he was a faculty member at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins (Baltimore, MD), Dr. Michelle Till for her scientific contributions leading to the design of the study and Dr. David Scadden for contributing patients to the study. Supported in part by grants from the Department of Health and Human Services and the National Institutes of Health CA23318 to the Eastern Cooperative Oncology Group (ECOG) statistical center, CA66636 to the ECOG data management center, CA21115 to the ECOG coordinating center and chairman’s office, U01 CA121947 to the AIDS Malignancy Consortium.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cianfrocca, M., Lee, S., Von Roenn, J. et al. Pilot study evaluating the interaction between paclitaxel and protease inhibitors in patients with human immunodeficiency virus-associated Kaposi’s sarcoma: an Eastern Cooperative Oncology Group (ECOG) and AIDS Malignancy Consortium (AMC) trial. Cancer Chemother Pharmacol 68, 827–833 (2011). https://doi.org/10.1007/s00280-010-1509-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1509-4