Abstract
Purpose
Little information is available about changes in renal function after cisplatin-based chemotherapy (CBCT) in patients with a solitary kidney. The authors evaluated the renal safety and efficacy of CBCT after nephroureterectomy for upper urinary tract-urothelial carcinoma (UUT-UC).
Methods
The data of patients who underwent nephroureterectomy for UUT-UC and received CBCT for adjuvant and/or palliative treatment were reviewed. Renal function changes and renal function–related adverse events (AEs) were analyzed, and objective tumor responses were assessed.
Results
Sixty patients were enrolled, and a median of 6 cycles (1–22) of CBCT were administered. After the 3rd cycle of CBCT, serum creatinine levels were significantly higher than at baseline, whereas mean creatinine clearances and estimated glomerular filtration rates were significantly lower. These renal function indicators also tended to be lower than baseline after the 6th–21st cycles, but these decreases were not significant. Significant AEs (≥grade 2) occurred in 10 patients (16.7%), and serious AEs (≥grade 3) developed in two that required temporary hemodialysis. Univariate analysis revealed that a low estimated glomerular filtration rate at baseline was related to the occurrence of a significant renal AE with borderline significance (Hazard ratio = 3.284, P = 0.100). The overall tumor response rate was 30.2%, and tumor response rates of 1st, 2nd, and 3rd line therapies were 36.4, 25.0, and 12.5%, respectively.
Conclusions
Cisplatin-based chemotherapy can be administered in the majority of patients with UUT-UC with a solitary kidney after nephroureterectomy without inducing a serious AE, and provides acceptable efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Upper urinary tract-urothelial carcinoma (UUT-UC) has high local and systemic failure rates, even after radical surgery, and 5-year survival rates in patients with a pT3 or greater lesion have been reported to be <50% [1–3]. These poorer results and the chemosensitivity of UC raise questions concerning adjuvant chemotherapy. Some oncologists have advocated the use of adjuvant chemotherapy in advanced stage UUT-UC, but adjuvant chemotherapy has not been widely used for two reasons; a lack of convincing data that supports the efficacy of adjuvant chemotherapy in UUT-UC, and the assumed risk of nephrotoxicity to the presence of a solitary anatomical or functional renal unit, which undoubtedly dissuades oncologists from administering cisplatin-based chemotherapy (CBCT) after nephroureterectomy [4].
Unfortunately, little information is available about changes in renal function after CBCT in patients with a solitary kidney. Accordingly, we evaluated the renal safety and efficacy of long-term CBCT in patients with a solitary kidney after nephroureterectomy for UUT-UC.
Patients and methods
Patients
This study was approved by the National Cancer Center institutional review board (NCCNCS-09-302). We reviewed the archived data maintained in a prospective upper urinary tract cancer database at the National Cancer Center of 119 consecutive patients treated between 2001 and 2008. This study included patients that underwent nephroureterectomy for UUT-UC and received adjuvant and/or palliative CBCT. Patients with a non-urothelial carcinoma histology, those that underwent neoadjuvant chemotherapy, and those that treated with a non-cisplatin-based chemotherapeutic regimen were excluded.
Radical nephroureterectomy was performed in 95 patients (79.8%) without a metastatic lesion at initial presentation. Adjuvant chemotherapy was recommended to patients with pT3, pT4, lymph node–positive disease, or multifocal lymphovascular invasion. Forty-seven patients (49.5%) were deemed potential candidates for adjuvant chemotherapy according to these criteria. Final decisions on chemotherapy were based on a combination of factors: the presence of a coexisting condition, presumed patient ability to withstand treatment, and willingness to comply. Written informed consent was obtained from all patients.
Thirty-eight patients received adjuvant CBCT, and of these patients, another cisplatin-based regimen was re-administered to 13 patients with palliative intent after disease recurrence. In addition, another 22 patients, who had not received adjuvant chemotherapy, also underwent palliative CBCT. Finally, 60 patients were enrolled in the present study. The median follow-up duration was 36 months (3–105) (Table 1).
Treatment dosage and schedule
Of the 38 patients that received adjuvant CBCT, a gemcitabine plus cisplatin (GC) regimen was administered to 31, and a methotrexate, vinblastin, adriamycin, plus cisplatin (M-VAC) regimen was administered to 7. In selected patients, if no disease recurrence was observed after the initial 3 cycles, 1–3 cycles of chemotherapy were added using the same regimen. However, if disease recurrence occurred, the above-mentioned two regimens were switched.
Regarding the 35 patients that received palliative CBCT, the GC and M-VAC regimens were used for 1st line chemotherapy in 19 and 16 patients, respectively. Objective response was evaluated after every three cycles, three repetitive cycles of the same regimen were provided to patients without disease progression. After the failure of 1st line therapy, the aforementioned regimens were switched, and 2nd line therapy was started. After 2nd line treatment failure, paclitaxel plus cisplatin (TP) regimen was administered as a 3rd line therapy in selected patients. These regimens were continued until the disease progressed or toxicity became intolerable. Treatment schedules and doses were as follows: gemcitabine 1,000 mg/m2 on days 1, 8, and 15 and cisplatin 70 mg/m2 on day 2 for the GC regimen; and methotrexate 30 mg/m2 on days 1, 15, and 22, vinblastine 3 mg/m2 on days 2, 15, and 22, adriamycin 30 mg/m2 on day 2, and cisplatin 70 mg/m2 on day 2 for the M-VAC regimen. The TP regimen involved paclitaxel at 175 mg/m2 on day 1 and cisplatin at 70 mg/m2 on day 2. The dose of cisplatin was adjusted according to creatinine clearance (CrCl), which was measured using 24-h urine samples during each treatment cycle. If CrCl was ≥50 ml/min but <70 ml/min, the cisplatin dose was reduced by 25%, but if CrCl was ≥30 ml/min but <50 ml/min, the cisplatin dose was reduced by 50%. Other clinical procedures not mentioned above were as previously reported [5–7].
Renal safety and efficacy assessments
Renal functions were compared to baseline values after every 3 cycles. Serum creatinine, CrCl, and estimated glomerular filtration rate (eGFR) were used as indicators of renal function. Estimated GFRs were calculated using the Modification of Diet in renal disease equation [8]. Renal function-related adverse events (AEs) are described using the Common Terminology Criteria for Adverse Events (version 3) [9]. Objective tumor response was assessed using the Response Evaluation Criteria in Solid Tumors [10].
Data and statistical analysis
Baseline to post-chemotherapy renal function differences were tested using the paired t test and Wilcoxon’s signed rank test. To identify risk factors for the development of significant AE, univariate Cox proportional hazards models were used, and CBCT cycles were used as a time variable. The Statistical Package for the Social Sciences (version 12.0) for Windows® was used for the statistical analysis, and two-sided P values of <0.05 were considered significant.
Results
The median number of CBCT cycles taken was 6 (1–22), 58 patients (96.7%) received ≥3 cycles of CBCT, only 1 cycle was administered to the other 2 patients due to patient unwillingness (Table 1). A reduced dose of cisplatin was administered to 57 patients (95.0%) during 1st cycle due to low CrCl levels.
Changes in renal function were followed using serum creatinine, CrCl, and eGFR results in those that underwent at least 3 cycles of CBCT. Baseline mean serum creatinine (mg/dl), CrCl (ml/min), and eGFR (ml/min/1.73 m2) values were 1.34 ± 0.21, 52.43 ± 8.08, and 54.41 ± 8.92, respectively. After 3rd cycle, serum creatinine, CrCl, and eGFR values were 1.39 ± 0.23, 51.03 ± 9.14, and 52.85 ± 10.02, respectively. After 3rd cycle, mean serum creatinine was significantly higher than baseline (P = 0.0051), and mean CrCl (P = 0.0242) and eGFR (P = 0.0243) were significantly lower than baseline. Even after the 6th–21st cycles, these renal function indicators showed a tendency to be lower than baseline, but no significant difference was observed between renal function indicators at baseline and post-chemotherapy (Table 2).
A significant AE (≥grade 2 AE) occurred in 10 patients (16.7%). Of these, 8 patients (5 on GC, 3 on TP) experienced a grade 2 AE (eGFR ≥ 18.5 ml/min/1.73 m2, <37.5 ml/min/1.73 m2) during the 2nd, 2nd, 6th, 6th, 7th, 10th, 16th, and 20th cycles of cisplatin-based chemotherapy. After conservative management, all grade 2 AEs remitted. Four patients continued chemotherapy after recovering renal function, but the other 4 refused further chemotherapy. A serious AE (grade 3 AE; eGFR < 18.5 ml/min/1.73 m2, chronic dialysis not indicated) developed in 2 patients during M-VAC treatment, and both required temporary hemodialysis. Univariate Cox proportional model analysis suggested that a low eGFR at baseline is a risk factor of time to the development of a significant AE with borderline significance (Hazard ratio = 3.284, P = 0.100). However, sex, age, a history of diabetes, a history of hypertension, serum creatinine, and CrCl were not found to be associated with the development of a significant AE (Table 3).
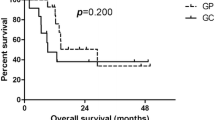
Palliative chemotherapy was provided to 35 patients, and the data of 33 of these patients were eligible for efficacy analysis. The overall response rate (ORR) to CBCT was 30.2% (16/53), and ORRs to 1st, 2nd, and 3rd line therapies were 36.4% (12/33), 25.0% (3/12), and 12.5% (1/8), respectively. In terms of the three regimens, the GC regimen achieved complete response (CR) in 2 (10.0%) and partial response (PR) in 7 (35.0%); the M-VAC regimen achieved CR in 1 (4.0%) and PR in 5 (20.0%), and the TP regimen achieved PR in 1 (12.5%) (Table 4).
Discussion
Given the established efficacy of CBCT, treating patients with advanced UUT-UC presents a substantial therapeutic dilemma because nephrectomized status is known to be an important risk factor of the development of new-onset chronic kidney disease [11, 12]. In this study, baseline CrCl was <60 ml/min in 50 patients (83.3%), and <50 ml/min in 22 patients (36.7%) after nephroureterectomy. In addition, patients with UUT-UC are usually elderly, and the probability of ineligibility for CBCT increases with age [13].
Our study shows that long-term CBCT tends to reduce renal function in patients with a solitary kidney, but differences between renal functions pre- and post-chemotherapy were not as obvious as expected. Our observations are in-line with those of Hellenthal et al. [4], who showed that serum creatinine levels in patients treated with M-VAC increased from an average of 1.2 mg/dl preoperatively to 1.3 mg/dl after surgery and chemotherapy. However, the use of CBCT in patients with a low creatinine clearance remains controversial. In the majority of clinical trials on CBCT, adequate renal function is a prerequisite and eligibility cutoffs of <2.0 mg/dl for serum creatinine, and/or of >60 ml/min for calculated CrCl are applied [14]. According to these criteria, >80% of the patients enrolled in the present study might have been considered ineligible for CBCT. Nevertheless, empiric guidelines suggest that cisplatin can be administered at lower doses to patients with renal impairment [15], but data supporting such recommendations are lacking. In the present study, a low eGFR at baseline tended to be related to a significant AE, but this was less informative with respect to the prediction of a serious AE, because eGFR values of the two patients (53.0 and 59.3 ml/min/1.73 m2) who experienced a serious AE were not much lower than those of the other patients. Nonetheless, split-dose administration of weekly cisplatin can helpfully sustain efficacy and reduce toxicity in patients with renal impairment.
Nephrotoxicity is the major dose-limiting side effect of cisplatin, but repeat cisplatin administration has been shown to reduce GFR chronically in a dose-dependent manner [16]. On the other hand, carboplatin is regarded as a promising alternative for patients with renal function impairment, because its action mechanism is similar to that of cisplatin, and at standard doses (up to 400 mg/m2), it does not cause nephrotoxicity or neurotoxicity. However, despite the considerable concerns about the renal toxicity of cisplatin in patients with an impaired renal function, we prefer reducing cisplatin dose rather than substituting carboplatin for the following reasons. Although small single institutional studies have reported similar response rates and a more favorable toxicity profile for carboplatin [17], it remains uncertain whether carboplatin can be substituted for cisplatin without comprising efficacy. During the M-VAC era, two single-institution randomized phase 2 studies showed lower levels of gastrointestinal, renal, neurologic, and otologic toxicities in the carboplatin arm. However, results suggested better efficacy for the cisplatin-based regimen when ORR and median survival were considered [18, 19]. Furthermore, a recent phase 2 randomized study showed that the ORR was 49.1% in the GC arm (CR = 14.5%; PR = 34.5%) and 40.0% in the gemcitabine plus carboplatin arm (CR = 1.8%; PR = 38.2%) [20]. Accordingly, the above results indicate that the substitution of cisplatin by carboplatin cannot be routinely recommended in patients able to tolerate CBCT [17, 21].
Although long-term CBCT is feasible in patients with a solitary kidney and renal functional impairment, some critical issues remain. In our study, serum creatinine, CrCl, and estimated glomerular filtration rate (eGFR) were used as indicators of renal function. However, they are considered to be relatively inaccurate when compared with measures of 51Cr-EDTA plasma clearance [22, 23], another problematic issue is whether reducing cisplatin dose according to CrCl maintains its efficacy. Our results suggest that cisplatin remains active at a reduced dose, but the ORR found in the present study seems to be somewhat lower than those reported in contemporary series. Furthermore, comparisons between our findings and those of clinical trials are difficult, because strict enrollment criteria are normally applied during clinical trials. In addition, some patients who received long-term CBCT experienced serious chemotherapy-induced peripheral neuropathy or ototoxicity in a total cumulative dose-dependent manner [24, 25]. Based on our experiences, peripheral nephropathy is a more debilitating problem than renal insufficiency, especially in long-term responders or survivors.
Finally, cisplatin resistance is an important obstacle to long-term CBCT, as is shown in the present study, the ORRs of CBCT decreased in the order 1st, 2nd, to 3rd line therapy. We previously reported that the efficacy of M-VAC was encouraging in patients with progressive disease after GC chemotherapy [26], and the present study also shows that another combination of CBCT after the failure of 1st line CBCT maintains some degree of efficacy. Accordingly, the failure of CBCT may not imply a cisplatin-refractory status, and cisplatin may still be active in some patients who failed prior CBCT. For this reason, we have used the TP regimen in selected patients as a 3rd line therapy. However, although no life-threatening complications were observed, its efficacy was limited and unsatisfactory. To date, no standard regimen has been agreed as a 2nd or 3rd line therapy, and therefore, new cytotoxic or targeted agents are urgently required to improve oncological outcomes and preserve quality of life.
Conclusions
The present study shows that long-term CBCT tended to reduce renal function in patients with a solitary kidney after nephroureterectomy for UUT-UC. However, it also shows that long-term CBCT can be administered to the majority of these patients without inducing a serious AE, and that in these patients it provides acceptable efficacy. Furthermore, our findings suggest that close monitoring for AE is needed in patients with a low eGFR.
References
Hall MC, Womack S, Sagalowsky AI, Carmody T, Erickstad MD, Roehrborn CG (1998) Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology 52:594–601
Langner C, Hutterer G, Chromecki T, Winkelmayer I, Rehak P, Zigeuner R (2006) pT classification, grade, and vascular invasion as prognostic indicators in urothelial carcinoma of the upper urinary tract. Mod Pathol 19:272–279
Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E et al (2009) Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 115:1224–1233
Hellenthal NJ, Shariat SF, Margulis V, Karakiewicz PI, Roscigno M, Bolenz C et al (2009) Adjuvant chemotherapy for high risk upper tract urothelial carcinoma: results from the Upper Tract Urothelial Carcinoma Collaboration. J Urol 182:900–906
Uhm JE, Lim HY, Kim WS, Choi HY, Lee HM, Park BB et al (2007) Paclitaxel with cisplatin as salvage treatment for patients with previously treated advanced transitional cell carcinoma of the urothelial tract. Neoplasia 9:18–22
von der Maase H, Hansen SW, Roberts JT, Dogliotti L, Oliver T, Moore MJ et al (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 18:3068–3077
Loehrer PJ Sr, Einhorn LH, Elson PJ, Crawford ED, Kuebler P, Tannock I et al (1992) A randomized comparison of cisplatin alone or in combination with methotrexate, vinblastine, and doxorubicin in patients with metastatic urothelial carcinoma: a cooperative group study. J Clin Oncol 10:1066–1073
Poggio ED, Wang X, Weinstein DM, Issa N, Dennis VW, Braun WE et al (2006) Assessing glomerular filtration rate by estimation equations in kidney transplant recipients. Am J Transplant 6:100–108
Cancer Therapy Evaluation Program: Common Terminology Criteria for Adverse Events (CTCAE) v. 3.0. http://ctep.info.nih.gov/reporting/ctc.html. http://ctep.info.nih.gov/reporting/ctc.html
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7:735–740
Lucas SM, Stern JM, Adibi M, Zeltser IS, Cadeddu JA, Raj GV (2008) Renal function outcomes in patients treated for renal masses smaller than 4 cm by ablative and extirpative techniques. J Urol 179:75–79 (discussion 79–80)
Dash A, Galsky MD, Vickers AJ, Serio AM, Koppie TM, Dalbagni G et al (2006) Impact of renal impairment on eligibility for adjuvant cisplatin-based chemotherapy in patients with urothelial carcinoma of the bladder. Cancer 107:506–513
Raj GV, Iasonos A, Herr H, Donat SM (2006) Formulas calculating creatinine clearance are inadequate for determining eligibility for cisplatin-based chemotherapy in bladder cancer. J Clin Oncol 24:3095–3100
Kintzel PE, Dorr RT (1995) Anticancer drug renal toxicity and elimination: dosing guidelines for altered renal function. Cancer Treat Rev 21:33–64
Arany I, Safirstein RL (2003) Cisplatin nephrotoxicity. Semin Nephrol 23:460–464
Garcia JA, Dreicer R (2006) Systemic chemotherapy for advanced bladder cancer: update and controversies. J Clin Oncol 24:5545–5551
Petrioli R, Frediani B, Manganelli A, Barbanti G, De Capua B, De Lauretis A et al (1996) Comparison between a cisplatin-containing regimen and a carboplatin-containing regimen for recurrent or metastatic bladder cancer patients. A randomized phase II study. Cancer 77:344–351
Bellmunt J, Ribas A, Eres N, Albanell J, Almanza C, Bermejo B et al (1997) Carboplatin-based versus cisplatin-based chemotherapy in the treatment of surgically incurable advanced bladder carcinoma. Cancer 80:1966–1972
Dogliotti L, Carteni G, Siena S, Bertetto O, Martoni A, Bono A et al (2007) Gemcitabine plus cisplatin versus gemcitabine plus carboplatin as first-line chemotherapy in advanced transitional cell carcinoma of the urothelium: results of a randomized phase 2 trial. Eur Urol 52:134–141
Culine S (2007) Chemotherapy for advanced transitional cell carcinoma of the urothelium: cisplatin or carboplatin? Eur Urol 52:9–10
Herget-Rosenthal S, Bokenkamp A, Hofmann W (2007) How to estimate GFR-serum creatinine, serum cystatin C or equations? Clin Biochem 40:153–161
Sambataro M, Thomaseth K, Pacini G, Robaudo C, Carraro A, Bruseghin M et al (1996) Plasma clearance rate of 51Cr-EDTA provides a precise and convenient technique for measurement of glomerular filtration rate in diabetic humans. J Am Soc Nephrol 7:118–127
Quasthoff S, Hartung HP (2002) Chemotherapy-induced peripheral neuropathy. J Neurol 249:9–17
Rybak LP (2007) Mechanisms of cisplatin ototoxicity and progress in otoprotection. Curr Opin Otolaryngol Head Neck Surg 15:364–369
Han KS, Joung JY, Kim TS, Jeong IG, Seo HK, Chung J et al (2008) Methotrexate, vinblastine, doxorubicin and cisplatin combination regimen as salvage chemotherapy for patients with advanced or metastatic transitional cell carcinoma after failure of gemcitabine and cisplatin chemotherapy. Br J Cancer 98:86–90
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cho, K.S., Joung, J.Y., Seo, H.K. et al. Renal safety and efficacy of cisplatin-based chemotherapy in patients with a solitary kidney after nephroureterectomy for urothelial carcinoma of the upper urinary tract. Cancer Chemother Pharmacol 67, 769–774 (2011). https://doi.org/10.1007/s00280-010-1349-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1349-2