Abstract
Background
Fluoropyrimidine drugs are widely used in head and neck cancer (HNC). DPD deficiency is a pharmacogenetics syndrome associated with severe/lethal toxicities upon 5-FU or capecitabine intake. We have developed a simple, rapid, and inexpensive functional testing for DPD activity, as a means to identify deficient patients and to anticipate subsequent 5-FU-related toxicities. We present here the impact of fluoropyrimidine dose tailoring based on DPD functional screening in a prospective, open, non-controlled study, both in term of reduction in severe toxicities and of treatment efficacy.
Methods
About 65 patients with HNC (59 ± 9 years, 52M/13F, Prospective Group) were entered into the study. Screening for DPD deficiency was performed prior to the beginning of the chemotherapy or radiochemotherapy. DPD status was evaluated by monitoring U/UH2 ratio levels in plasma as a surrogate marker for enzymatic functionality. 5-FU doses were reduced according to the extent of the detected DPD impairment, and adjusted on the basis of age, general condition, and other clinical/paraclinical covariates, if required. Treatment-related toxicities and subsequent impact on treatment delay were carefully monitored next for comparison with a retrospective, Reference subset of 74 other patients with HNC (mean age: 59 ± 10, 58M/16F, Reference Group), previously treated in the same institute with similar schedule but using standard 5-FU dosage.
Results
Thirty-one out of 65 patients (48%) were identified as mildly (28%) to markedly (20%) DPD deficient. Subsequently, dose reductions ranging from 10 to 100% with 5-FU were applied in those patients. In this group, six patients (9%) experienced severe toxicities, none of them being life threatening, and no toxic death was encountered. In comparison, 16 out of 74 patients (22%) of the Reference Group displayed severe side effects after standard 5-FU administration, 13% being life-threatening toxicities (e.g., G4 neutropenia + sepsis). Moreover, one toxic death was observed in this Reference Group. No postponement or cancelation of forthcoming chemoradiotherapy courses occurred in the Prospective Group, whereas treatment had to be disrupted in six patients (8%) from the Reference Group. No difference in first-line therapy efficacy was evidenced between the two subsets (78 vs. 79% response, P = 0.790).
Conclusions
Although non-randomized, this study strongly suggests that prospective determination of DPD status has an immediate clinical benefit by reducing the drug-induced toxicities incidence in patients treated with 5-FU, allowing an optimal administration of several courses in a row, while maintaining efficacy. Our preliminary results thus advocate for systematic DPD screening in patients eligible for treatment with fluoropyrimidine drugs in HNC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 650,000 new cases of head and neck cancer (HNC) are reported worldwide every year, accounting for 6% of all new cancer cases. About 2/3 of these cases occur in developing countries, and HNC claims more than 350,000 lives a year. Men are more likely to be affected than women by this disease, probably due to gender differences in life-smoking habits [19].
At the time of diagnostic, usually, more than 2/3 of patients with HNC are at an advanced stage, which limits the efficacy of surgery and radiotherapy. In the last three decades, various chemotherapy options, such as concomitant chemoradiotherapy, induction chemotherapy, adjuvant chemoradiotherapy, and palliative chemotherapy, have been widely used to help organ preservation and treat metastasis patients to improve locoregional disease control, to prolong disease-free survival and overall survival.
Although CDDP is a mainstay in the therapy of head and neck cancer, over the past 40 years, antimetabolite drug 5-FU has been widely used in combination with platinum derivatives, or associated with radiotherapy. On the basis of a review of 32 studies involving 10,225 patients, Budach W. et al. showed that concomitant chemoradiotherapy including 5-FU either given alone or as part of combination with CDDP, CBDCA, or MMC yields to an improved clinical outcome [2]. Besides, the latest TPF (platinum + 5-FU + Docetaxel) or PPF (platinum + 5-FU + Paclitaxel) protocols have demonstrated a better organ preservation and survival benefit than the standard platinum + 5-FU schedule as induction chemotherapy [9, 10, 21, 31, 35]. Capecitabine, the oral pro-drug of 5-FU, is also given now [4], and overall, the use of fluoropyrimidine drugs is constantly increasing now for treating head and neck cancers.
Dihydropyrimidine dehydrogenase (DPD) is the initial and rate-limiting enzyme that detoxifies 5-FU in the liver [14, 18]. DPD deficiency is a condition that can lead to dramatic alteration in the 5-Fu pharmacokinetic profile, more than 85% of the drug being catabolized by DPD [15]. Admittedly, 30–40% of the severe toxicities upon 5-FU exposure could be attributed to some kind of DPD impaired activity, a figure that can rise to 60–70% in some recent studies [6]. In the most extreme cases, total DPD deficiency can even lead to toxic death upon 5-FU administration [5, 13]. Detecting DPD deficiency is therefore a major issue in clinical oncology, although the best strategies to achieve DPD screening at the bedside remain to be identify [11]. Because this enzyme is responsible for the reduction in uracil (U) to dihydrouracil (UH2), monitoring physiological U/UH2 ratios in plasma could provide a quick insight into DPD activity status. We have developed such [16] over a 3-year period at our institute [16]. Abnormal ratios suggesting 5-FU deficiency was evidenced in more than 70% of the patients presenting with severe toxicity and 80% of those with fatal outcome, thus strongly suggesting that this test could be a convenient market in a prospective setting by detecting patients likely to experience severe/lethal toxicities upon 5-FU intake. Here, we present the clinical results (related toxicities and response) of the prospective use of this test in patients with HNC.
Patients and methods
Eligibility criteria
Patients included in this study were scheduled for 5-FU-based treatment for histologically proven head and neck cancer. All patients were hospitalized at La Timone University hospital of Marseille. Written informed consent and local ethical committee approval were obtained before starting the study. Eligibility required a histologically confirmed diagnosis of head and neck cancer, being either primarily diagnosed or relapse. Patients may have been treated with 5-Fu before. In addition, all of them, more than 18-years-old, were not on drugs known to interfere with DPD, such as raltitrexed or other uridine derivatives such as antiviral Sorivudine. Patients were required to have adequate absolute neutrophil count >2,000/mm3 and platelets count >100,000/mm3. Their performance status should be from 0 to 2 (WHO). Patients with no indication of 5-Fu, displaying abnormal liver or renal functions and pregnancy/lactation periods, were excluded from the study. In addition, patients whose venous condition was not suitable for proper blood sampling were also excluded.
DPD functional testing
DPD testing was performed prospectively in all patients from Prospective Group and retrospectively in patients from Reference Group, when possible. Five milliliters of blood was withdrawn on heparinized tubes limited between 8 and 9 am in order to limit the impact of circadian rhythm on DPD activity [17]. Plasma fraction was isolated by centrifugation and kept frozen at −80°C until analyzed. Functional DPD testing was performed by monitoring U/UH2 plasma ratio as first theorized by Sumi et al. [27]. U/UH2 ratios were generated by UV-HPLC analysis after liquid–liquid extraction as described previously, with minor modifications [6]. Patients were identified as non-deficient, mildly deficient, severely deficient, or totally deficient according to their U/UH2 ratio. DPD status was given within a 3–10 days range after sample collection, so as to not delay start of the treatment.
Fluoropyrimidine administration and dose tailoring
Patients with no suspected DPD deficiency were treated with standard dosage. Patients identified as mild- to severe-deficient had their 5-FU dose reduced by 10–50%, as shown in Table 1. Total deficiency led to selection for other treatment modalities without 5-FU. Dose reduction could be further personalized on the basis of age and general condition of the patients, if required. Consequently, a similar level of DPD deficiency in two different patients could lead to different range of dose reductions (i.e., in the severely DPD-deficient subset, doses were cut by 20, 30, or 50% according to each patient’s medical record).
Concomitant drugs and radiotherapy
CDDP, CBDCA, and Paclitaxel co-administered with 5-FU were given standard dose. Radiotherapy dose was 70 Gy (2Gy/35F/7W) for local tumor, and 50 Gy (2Gy/25F/5W) for lymph nodes.
Toxicity monitoring
After the first course, acute and subacute toxic reactions were assessed and graded according to standard CTC-NCI criteria. In first-line chemoradiotherapy, toxicity was assessed after each course. All grade 3–4 toxicities and unusually delayed G2 toxicities (e.g., G2 thrombocytopenia lasting more than 3 weeks) were analyzed. Considering that it is difficult to distinguish the mucositis lasting from a previous course from the one repeatedly occurring each new course, this side effect was counted only once for each patient.
Response monitoring
Treatment efficacy was studied only in patients treated as first-line therapy after completion of scheduled therapy. Therapeutic efficacy was evaluated 8 weeks after the treatment was completed (Recist WHO, 1979). The disappearance of all lesions was defined as complete response (CR). Partial response (PR) was associated with a decrease of more than 50% of the disease evidence. Reduction less than 50% with no new lesions was identified as stable disease (SD). Increase in disease by more than 25%, or appearance of new lesion would be described as progression disease (PD).
Statistical analysis
Differences in measured values were analyzed with t-test, whereas enumeration data were compared with chi square test. When the number of patients was too small in some subsets (e.g., <5), fisher test was used. Wilcoxon Mann–Whitney test was adopted to rank data. Normality was assessed with Kolmogorov–Smirnov. The statistic analysis was performed using SPSS 17.0 software.
Results
Patients
From February 2006 to July 2007, 67 patients were included in the Prospective Group with adjusted doses. In this later group, two patients were found ineligible and excluded from the analysis. We reviewed 74 historical patients with HNC who have received a treatment with standard dose of 5-FU from June 2005 to February 2006 (Reference Group). Patients’ and treatment’s characteristics are given in Table 2.
DPD status evaluation and 5-FU and capecitabine dose adjustment
In the Prospective Group, U/UH2 ratio’s distribution followed a normal distribution (Kolmogorov–Smirnov test, P < 0.01), with a median of 2, and a mean value of 2.23 ± 1.26. Thirty-one out of 65 (48%) patients were identified with mild (28%) and severe (20%) DPD deficiency (U/UH2 ratio >2 and >3, respectively, following the cutoff defined previously [6]. 5-FU dosage was reduced in 26 patients (47%), and the remaining 39 patients (63%) were treated with the standard dose as initially scheduled (Table 1). Difference in 5-FU dosage between Reference Group and Prospective Group was significant (3,765 ± 1,022 vs. 3,295 ± 1,078 mg/m², P = 0.01). Capecitabine was administered in two patients, one of them being identified as deficient with subsequent 20% dosage reduction.
Toxicities and treatment delay
Comparison between toxicity types and frequencies observed in Reference Group and Prospective Group according to treatment type (e.g., chemotherapy or chemotherapy + radiotherapy) is displayed in Table 3. Overall, 16 of the 74 patients (22%) from the Reference Group presented with severe toxicities, whereas 6 of 65 patients (9%) in Prospective Group experienced such severe side effects. The difference between Reference Group and Prospective Group was significant (P = 0.046).
Six patients from the Reference Group have their treatment delayed or canceled. Toxicities observed in the Reference Group led to postponing forthcoming radiotherapy course in one patient, cancelation of radiotherapy in one patient, and stopping forthcoming chemotherapy courses in four other patients. There was neither cancelation nor course postponement in patients from the Prospective Group, and all chemotherapeutic or radiochemotherapeutic courses were performed as initially scheduled.
Treatment efficacy in patients treated as first-line chemoradiotherapy
Sixty patients from the Reference Group and 34 patients from the Prospective Group were administrated first-line chemoradiotherapy and were evaluated for response. Five patients in the Reference Group and two from the Prospective Group died of complications or cancer progression after three cycles of chemoradiotherapy. Two patients were lost to follow-up in the Reference Group, and one patient was similarly lost in the Prospective Group. One patient in the Reference Group experienced toxic death. Two patients from the Prospective Group could not be monitored for response, because their treatment for coexisting breast cancer and esophagus was still ongoing. Response rates (CR + PR) were 78 and 79%, respectively, in the Reference Group and the Prospective Group, and progressive disease rates (PD) were 21% in both groups (P = 0.790) (Table 4).
Discussion
Depending on schedule (chemotherapy alone or chemoradiotherapy), the inherent toxicity of fluoropyrimidine drugs such as 5-fluorouracil (5-FU) and capecitabine often leads to myelosuppression, mucositis, diarrhea, hand and foot syndrome, in about 16–43% of patients [1, 12]. In the most extreme case, toxicity can become life threatening. In patients with HNC, when concomitant chemoradiotherapy is scheduled, radiotherapy may be canceled or postponed because of the toxicity encountered with 5-FU. This disruption in the protocol subsequently increases the risk of treatment failure [8, 20]. Plasma concentrations of 5-FU are associated with both side effects and responses in patients with HNC [24, 28, 29, 32]. More than two decades ago, it has been shown that pharmacokinetically guided dosage adjustment of 5-FU applied to the treatment of head and neck cancers can minimize the drug-related toxicity and enhance therapeutic index [23]. Following this, Wilhm et al. confirmed that dose tailoring could greatly minimize toxicity without compromising efficacy [34]. A multicentric randomized trial in France confirmed that conclusion in 1998 [7].
Although dosage adjustment can significantly reduce side effect and avoid toxic death in some cases, this strategy is not a common practice in medical oncology, despite the narrow therapeutic indices of most anticancer agents [33]. Application of dose-tailoring methods is hampered by the frequent blood sample collection required during treatment, relatively complex calculations, and the rigorous control of infusion rates in order to prevent erratic fluctuations of drug concentration in plasma. In this case, it becomes necessary to develop simpler approaches that meet the requirements of daily clinical practice. Here, we present a DPD-based strategy for tailoring 5-FU dosage in patients with HNC. Here, our method required only one blood sample before the treatment and needed no complex calculation. In the present study, we confirmed the pivotal role DPD deficiency had in the severe toxicities reported with 5-FU, because 64% of patients with such side effects in the historical Reference Group were retrospectively identified as DPD deficient.
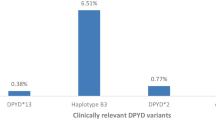
Surprisingly, DPD deficiency was evidenced in about 40% of the patients included in this study, an observation by far higher than the score usually expected with DPYD genetic polymorphism [30] but consistent with other recent clinical reports [36]. This higher figure can come from the strategy we used to evaluate DPD status. Here, DPD issue was addressed primarily following a functional testing, and not some kind of genetic studies that proved over the past to generate false-negative results [15]. However, intriguingly, the present figures were still much higher than the frequency of deficient patients we previously observed in another study using the same phenotypic method, in which about 10–15% of the patients displayed DPD deficiency [6]. This discrepancy could come from the medical history of the patients we included. Patients with HNC frequently have a record of tobacco-alcohol history, and little is known on the impact these characteristics might have on DPD functionality in the liver. Similarly, pancreatitis and hepatitis along with other hepatic disorders frequently observed in this very population could have impacted as well on the DPD status. Further experiments will have to be conducted to elucidate whether alcohol-tobacco dependence can lead to DPD dysfunction, as it does for other liver enzymes such as cytochromes P450 [22]. Additionally, patients with HNC are more frequently co-administered than other patients with a variety of drugs for supportive care (e.g., local antibiotics and artificial nutrition) likely to interact with DPD activity, on a classical drug–drug interaction basis.
5-FU dosage was empirically tailored according to the DPD status, and mean final doses were found to be lower when compared with standard doses required for treating HNC. As a result, a marked reduction in treatment-related toxicities was achieved. In the control group undergoing standard therapy, 22% of the patients experienced severe toxicities, one ending with fatal outcome. This figure is fully consistent with the usual adverse drug reactions reported with fluoropyrimidine drugs [1, 12]. Incidence of severe toxicities was reduced by more than the half (9%) in the Prospective Group, and no toxic death was encountered anymore, an observation in line with the dose reduction performed before administrating the drug in the patients identified as possibly DPD deficient. Because a major concern of such dose reduction is a negative impact on treatment efficacy, we monitored response rates as a clinical endpoint. To this end, responses were compared between Reference and Prospective subsets of patients fully comparable clinically (e.g., first-line radiochemotherapy) and compared with historical response rates usually found in the literature with patients with HNC. Similar response rates were achieved in the Reference and Prospective Groups, thus suggesting that our strategy helped to secure the administration of 5-FU, without impacting negatively on the treatment efficacy. Besides, the overall 60% response rates found in our patients is consistent with efficacy usually reported in others study [3, 25, 26]. Overall treatment time (OTT) of radiotherapy was improved in the Prospective Group (P = 0.084), whereas several patients had to have their protocol postponed or canceled in the Reference Group. Because it is fully acknowledged that any delay >1 week in radiotherapy unfavorably impact on survival [8, 20], our strategy should improve clinical outcome in patients scheduled for 5-FU-based radiochemotherapy. This DPD-based dose-tailoring strategy is now routinely used in our institute for any patient eligible for 5-FU or oral 5-FU therapy.
Conclusions
Here, DPD issue was addressed using a simple functional test that met the requirements of routine clinical practice. Subsequent 5-FU dosage adjustment greatly minimized the toxicity arisen from using fluoropyrimidine drugs, without compromising their efficacy. Our data showed as well that patients with HNC presenting with some DPD deficiency are more frequent than initially expected. Further investigations will have to be performed to understand this elevated rate of deficiency.
Although non-randomized, this study suggests that prospective use of DPD status has an immediate clinical benefit by reducing the drug-induced toxicities incidence found in patients treated with 5-FU and by allowing an optimal administration of several courses in a row. Our preliminary results advocate systematic DPD status screening in patients eligible for treatment with fluoropyrimidine drugs for HNC.
References
Browman GP, Cripps C, Hodson DI, Eapen L, Sathya J, Levine MN (1994) Placebo-controlled randomized trial of infusional fluorouracil during standard radiotherapy in locally advanced head and neck cancer. J Clin Oncol 12:2648–2653
Budach W, Hehr T, Budach V, Belka C, Dietz K (2006) A meta-analysis of hyperfractionated and accelerated radiotherapy and combined chemotherapy and radiotherapy regimens in unresected locally advanced squamous cell carcinoma of the head and neck. BMC Cancer 6:28
Choong N, Vokes E (2008) Expanding role of the medical oncologist in the management of head and neck cancer. CA Cancer J Clin 58:32–53
Chua D, Wei WI, Sham JS, Au GK (2008) Capecitabine monotherapy for recurrent and metastatic nasopharyngeal cancer. Jpn J Clin Oncol 38:244–249
Ciccolini J, Mercier C, Dahan L, Evrard A, Boyer JC, Richard K, Dales JP, Durand A, Milano G, Seitz JF, Lacarelle B (2006) Toxic death-case after capecitabine + oxaliplatin (XELOX) administration: probable implication of dihydropyrimidine dehydrogenase deficiency. Cancer Chemother Pharmacol 58:272–275
Ciccolini J, Mercier C, Evrard A, Dahan L, Boyer JC, Duffaud F, Richard K, Blanquicett C, Milano G, Blesius A, Durand A, Seitz JF, Favre R, Lacarelle B (2006) A rapid and inexpensive method for anticipating severe toxicity to fluorouracil and fluorouracil-based chemotherapy. Ther Drug Monit 28:678–685
Fety R, Rolland F, Barberi-Heyob M, Hardouin A, Campion L, Conroy T, Merlin JL, Riviere A, Perrocheau G, Etienne MC, Milano G (1998) Clinical impact of pharmacokinetically-guided dose adaptation of 5-fluorouracil: results from a multicentric randomized trial in patients with locally advanced head and neck carcinomas. Clin Cancer Res 4:2039–2045
Fowler JF, Lindstrom MJ (1992) Loss of local control with prolongation in radiotherapy. Int J Radiat Oncol Biol Phys 23:457–467
Hitt R, Lopez-Pousa A, Martinez-Trufero J, Escrig V, Carles J, Rizo A, Isla D, Vega ME, Marti JL, Lobo F, Pastor P, Valenti V, Belon J, Sanchez MA, Chaib C, Pallares C, Anton A, Cervantes A, Paz-Ares L, Cortes-Funes H (2005) Phase III study comparing cisplatin plus fluorouracil to paclitaxel, cisplatin, and fluorouracil induction chemotherapy followed by chemoradiotherapy in locally advanced head and neck cancer. J Clin Oncol 23:8636–8645
Hitt R, Paz-Ares L, Brandariz A, Castellano D, Pena C, Millan JM, Calvo F, Ortiz de Urbina D, Lopez E, Alvarez-Vicent JJ, Cortes-Funes H (2002) Induction chemotherapy with paclitaxel, cisplatin and 5-fluorouracil for squamous cell carcinoma of the head and neck: long-term results of a phase II trial. Ann Oncol 13:1665–1673
Innocenti F (ed) (2009) Genomics and pharmacogenomics in anticancer drug development and clinical response. Humana Press, Totowa
Jacobs C, Lyman G, Velez-Garcia E, Sridhar KS, Knight W, Hochster H, Goodnough LT, Mortimer JE, Einhorn LH, Schacter L et al (1992) A phase III randomized study comparing cisplatin and fluorouracil as single agents and in combination for advanced squamous cell carcinoma of the head and neck. J Clin Oncol 10:257–263
Johnson MR, Hageboutros A, Wang K, High L, Smith JB, Diasio RB (1999) Life-threatening toxicity in a dihydropyrimidine dehydrogenase-deficient patient after treatment with topical 5-fluorouracil. Clin Cancer Res 5:2006–2011
Longley DB, Harkin DP, Johnston PG (2003) 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer 3:330–338
Mercier C, Ciccolini J (2006) Profiling dihydropyrimidine dehydrogenase deficiency in patients with cancer undergoing 5-fluorouracil/capecitabine therapy. Clin Colorectal Cancer 6:288–296
Mercier C, Yang C, Ciccolini J, Balti M, Evrard A, Blesius A, Dahan L, Richard K, Seitz J, Lacarelle B, Favre R (2006) Determination of uracil/UH2 ratio as a potential surrogate for DPD status in cancer patients presenting with severe toxicities during fluoropyrimidine treatment. J Clin Oncol 24:2020 Meeting Abstracts
Milano G, Chamorey AL (2002) Clinical pharmacokinetics of 5-fluorouracil with consideration of chronopharmacokinetics. Chronobiol Int 19:177–189
Parker WB, Cheng YC (1990) Metabolism and mechanism of action of 5-fluorouracil. Pharmacol Ther 48:381–395
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Peters LJ, Withers HR (1997) Applying radiobiological principles to combined modality treatment of head and neck cancer–the time factor. Int J Radiat Oncol Biol Phys 39:831–836
Posner MR, Hershock DM, Blajman CR, Mickiewicz E, Winquist E, Gorbounova V, Tjulandin S, Shin DM, Cullen K, Ervin TJ, Murphy BA, Raez LE, Cohen RB, Spaulding M, Tishler RB, Roth B, Viroglio Rdel C, Venkatesan V, Romanov I, Agarwala S, Harter KW, Dugan M, Cmelak A, Markoe AM, Read PW, Steinbrenner L, Colevas AD, Norris CM Jr, Haddad RI (2007) Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N Engl J Med 357:1705–1715
Roos PH, Bolt HM (2005) Cytochrome P450 interactions in human cancers: new aspects considering CYP1B1. Expert Opin Drug Metab Toxicol 1:187–202
Santini J, Milano G, Thyss A, Renee N, Viens P, Ayela P, Schneider M, Demard F (1989) 5-FU therapeutic monitoring with dose adjustment leads to an improved therapeutic index in head and neck cancer. Br J Cancer 59:287–290
Schneider M, Etienne MC, Milano G, Thyss A, Otto J, Dassonville O, Mobayen H, Saudes L, Guillot T, Demard F (1995) Phase II trial of cisplatin, fluorouracil, and pure folinic acid for locally advanced head and neck cancer: a pharmacokinetic and clinical survey. J Clin Oncol 13:1656–1662
Specenier PM, Vermorken JB (2007) Neoadjuvant chemotherapy in head and neck cancer: should it be revisited? Cancer Lett 256:166–177
Specenier PM, Vermorken JB (2008) Recurrent head and neck cancer: current treatment and future prospects. Expert Rev Anticancer Ther 8:375–391
Sumi S, Kidouchi K, Ohba S, Wada Y (1995) Automated screening system for purine and pyrimidine metabolism disorders using high-performance liquid chromatography. J Chromatogr B Biomed Appl 672:233–239
Thyss A, Milano G, Renee N, Vallicioni J, Schneider M, Demard F (1986) Clinical pharmacokinetic study of 5-FU in continuous 5-day infusions for head and neck cancer. Cancer Chemother Pharmacol 16:64–66
Trump DL, Egorin MJ, Forrest A, Willson JK, Remick S, Tutsch KD (1991) Pharmacokinetic and pharmacodynamic analysis of fluorouracil during 72-hour continuous infusion with and without dipyridamole. J Clin Oncol 9:2027–2035
van Kuilenburg AB, Muller EW, Haasjes J, Meinsma R, Zoetekouw L, Waterham HR, Baas F, Richel DJ, van Gennip AH (2001) Lethal outcome of a patient with a complete dihydropyrimidine dehydrogenase (DPD) deficiency after administration of 5-fluorouracil: frequency of the common IVS14 + 1G > A mutation causing DPD deficiency. Clin Cancer Res 7:1149–1153
Vermorken JB, Remenar E, van Herpen C, Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss JH, van den Weyngaert D, Awada A, Cupissol D, Kienzer HR, Rey A, Desaunois I, Bernier J, Lefebvre JL (2007) Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer. N Engl J Med 357:1695–1704
Vokes EE, Mick R, Kies MS, Dolan ME, Malone D, Athanasiadis I, Haraf DJ, Kozloff M, Weichselbaum RR, Ratain MJ (1996) Pharmacodynamics of fluorouracil-based induction chemotherapy in advanced head and neck cancer. J Clin Oncol 14:1663–1671
Walko CM, McLeod HL (2008) Will we ever be ready for blood level-guided therapy? J Clin Oncol 26:2078–2079
Wihlm J, Leveque D, Velten M, Klein T (1993) Pharmacokinetic monitoring with dosage adjustment of 5 fluorouracil administered by continuous infusion. Bull Cancer 80:439–445
Worden FP, Moon J, Samlowski W, Clark JI, Dakhil SR, Williamson S, Urba SG, Ensley J, Hussain MH (2006) A phase II evaluation of a 3-hour infusion of paclitaxel, cisplatin, and 5-fluorouracil in patients with advanced or recurrent squamous cell carcinoma of the head and neck: Southwest Oncology Group study 0007. Cancer 107:319–327
Boisdron-Celle M, Remaud G, Traore S, Poirier AL, Gamelin L, Morel A, Gamelin E (2007) 5-Fluorouracil-related severe toxicity: a comparison of different methods for the pretherapeutic detection of dihydropyrimidine dehydrogenase deficiency. Cancer Lett 249:271–282
Acknowledgments
Dr. Chen Guang Yang had a generous grant from the Ambassade de France en Chine (French embassy in China). This work was supported by the Association pour la Recherche contre le Cancer (Grant #1094), by the Groupe des Entreprises Finançant la Lutte contre le Cancer (GEFLUC-Marseille Provence) and by Roche Oncologie France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, C.G., Ciccolini, J., Blesius, A. et al. DPD-based adaptive dosing of 5-FU in patients with head and neck cancer: impact on treatment efficacy and toxicity. Cancer Chemother Pharmacol 67, 49–56 (2011). https://doi.org/10.1007/s00280-010-1282-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1282-4