Abstract
Purpose
Low-dose methotrexate (MTX) therapy is the cornerstone treatment of acute lymphoblastic leukemia (ALL) and may enhance the activation of 6-mercaptopurine (6-MP) to 6-thioguanine nucleotides (6-TGN). Yet, data have established that high-dose MTX (HDMTX) hampers the accumulation of 6-TGN in red blood cells (RBC) and lymphoblasts.
Methods
To clarify the pharmacokinetic interactions between these two antimetabolites, we serially measured RBC 6-TGN and MTX polyglutamates (MTXPG) levels following repeated courses of HDMTX (5 g/m² over 24 h) with daily oral 6-MP (25 mg/m²) during interval therapy in 20 children with ALL.
Results
HDMTX produced a rapid reduction in RBC 6-TGN 24 h after the start of MTX, and this effect was sustained at least by the third day (median decrease −21%; P < 0.001). However, a return to pre-infusion of 6-TGN levels was observed by the time of the following HDMTX course 14 days later (P < 0.001). RBC MTX polyglutamates accumulation followed Michaelis–Menten kinetics but was not associated with the change in pre-infusion 6-TGN levels which remained stable during the interval period.
Conclusion
HDMTX does not appear to enhance 6-MP activation to 6-TGN. Moreover, given that the deleterious effect of HDMTX on intracellular 6-MP disposition has been shown to be several folds greater in lymphoblasts than in RBC. Our data warrant additional studies elucidating the optimal MTX dose synergizing with 6-MP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The optimization of antileukemic treatment regimens has considerably improved the outcome of childhood acute lymphoblastic leukemia (ALL), and the most recent TOTAL XV protocol has reported a 5-year survival rate greater than 90% [1]. Nonetheless, while these data are very encouraging, the incidence of relapse in ALL is still significant, and additional efforts to optimize the sequence, dosing, and schedule of administration of antileukemic agents will be essential to improve the survival of patients with high risk ALL and poor prognosis.
One of the cornerstone treatments of ALL is the combination of 6-mercaptopurine (6-MP) with low-dose methotrexate (MTX), and the observation that both these anticancer agents produce greater antileukemic effects than either treatment alone can be traced back nearly half a century ago [2]. 6-MP is a prodrug activated to 6-thioguanine nucleotides (6-TGN) by a multistep process involving several enzymes of the purine salvage pathway including hypoxanthine guanine phosphoribosyl transferase (HPRT), an anabolic route in competition with a thiopurine S-methyltransferase (TPMT)- and xanthine oxidase (XO)-mediated inactivation of 6-MP to 6-methylmercaptopurine (6-MMPN) and 6-thiouric acid, respectively [3]. Alternatively, MTX is an antifolate producing antileukemic effects through an accumulation to long-chain MTXPG that potently inhibit de novo purine, tetrahydrofolate, and thymidylate biosynthesis [4].
The biochemical and pharmacological basis to combine 6-MP and MTX stem from various in vivo and in vitro observations whereby de novo purine biosynthesis inhibition by MTXPG produces an elevation in cellular phosphoribosylpyrophosphate (PPPR) levels [5, 6], the cofactor for HPRT. Hence, the combination of MTX with 6-MP is synergistic in enhancing the activation of 6-MP to 6-TGN that are incorporated to nucleic acids. Furthermore, by inhibiting of XO [7], MTX produces an increase in 6-MP peak plasma concentrations and area under the curve [8]. Arguably, the rational to combine MTX with 6-MP is sound, and in vivo data have established that greater accumulation of red blood cells (RBC) MTXPG are associated with greater RBC 6-TGN levels during maintenance therapy of ALL with weekly low-dose MTX (i.e., 40 mg/m2) and daily oral 6-MP (75 mg/m2) [9]. Yet, the premise that MTX synergizes with 6-MP is somewhat challenged by recent data indicating that high MTX dosage (e.g., 1 g/m2) hampers 6-TGN accumulation following IV 6-MP administration (1 g/m2) during upfront treatment of ALL [10].
In the present study, we sought to clarify the relative contribution of HDMTX on 6-MP intracellular pharmacokinetics during interval therapy in children who received consecutive intravenous HDMTX courses (5 g/m² over 24 h every 14 days) with daily 6-MP (25 mg/m²).
Methods
Twenty children with ALL were enrolled in the European Organization for Research and Treatment of Cancer (EORTC) 58951 protocol. The protocol was divided into five treatment phases including induction (with a prephase), consolidation, interval, late intensification, and maintenance. Interval therapy started 77 days after induction and consisted of daily oral 6-MP (25 mg/m²) for 56 days together with three or four intravenous HDMTX (5 g/m²) courses at 14-days interval (days 8, 22, 36, and 50) depending on the risk group allocation at diagnostic (very high risk patients received only three HDMTX courses). Local institutional review committee approved the study, and informed consent from parents or guardians was collected for all children. HDMTX courses consisted of 500 mg/m² MTX infused over the first hour followed by a continuous infusion of 4,500 mg/m² MTX over the remaining 23 h. Folinic acid rescue therapy (12 g/m²) was administered every 6 h, starting 36 h after the beginning of infusion and given until MTX plasma levels were lower than 0.2 μM. Biochemical and hematological monitoring was carried out at each course. Grading scale used for adverse events evaluation was assessed using NCI CTC v3 criteria. Compliance to daily 6-MP treatment was assessed by study nurses.
During each course, MTX plasma concentrations were monitored at 24, 48, and 72 h after the start of MTX infusion using standard enzyme multiplied immunoassay technique (EMIT) (Cobas MiraTM, Roche laboratories). Similarly, RBC MTX polyglutamates (MTXPG, up to the pentaglutamate) and RBC 6-MP metabolites concentrations (6-TGN and 6-MMPN nucleotides) were measured before MTX infusion (0 h) and at 24, 48, and 72 h using validated liquid chromatography methods as described [11, 12] and reported as pmol/109 RBC for MTXPG and pmol/8 × 108 for 6-MP metabolites. RBC MTXPG levels were categorized as short-chains MTXPG (MTXPG1–2 as the sum of MTXPG1 with MTXPG2), long-chain MTXPG (MTXPG3), or very long-chains MTXPG (MTXPG4–5 as the sum of MTXPG4 with MTXPG5). Total MTXPG levels were calculated as the sum of all MTXPG species (MTXPG1–5). Statistical analysis was carried out using Statistica (Statsoft, Tulsa, OK). The kinetics of MTXPG accumulation was assessed using GraphPad Prism 4 software (GraphPad, La Jolla, CA). Pairwise differences between 6-TGN and 6-MMPN levels were analyzed using Wilcoxon’s test, and correlations were determined using Spearman rank test.
Results
A total of 20 children (13 boys and 7 girls) with ALL aged 2–15 (mean: 6.35 ± 3.42 y, average ± SD) were enrolled. Fifteen patients presented with B-ALL, and five patients presented T-ALL. A total of 78 HDMTX courses were administered, 18 patients received four courses HDMTX, and two patients received three courses (one patient relapsed after the third course, and one patient with very high risk ALL received three courses per protocol). Blood for RBC 6-thiopurine nucleotides (6-TGN and 6-MMPN) or RBC MTXPG measurements was available in 76 of these 78 courses. Creatinine clearance was 127 ± 22 ml/min (n = 20) at the start of the first course, and renal function remained normal during interval therapy (not shown). No significant hematological or biochemical toxicities occurred during the study period, and none of the patients required discontinuation of or alteration in 6-MP therapy. Three grade 3–4 adverse effects occurred in three patients (two infections and one meningitis relapse).
Plasma and RBC MTX concentrations during the first HDMTX course (day 8) are presented in Fig. 1a, b. RBC MTXPG1 (MTX) concentrations rapidly increased and then decreased in parallel to plasma MTX concentrations. Low albeit significant MTX di-glutamate (MTXPG2) formation was detected in circulating erythrocytes during the first HDMTX course, but MTXPG with greater than two glutamic residues were undetectable. Within each subsequent course, there was no significant change in RBC MTXPG3–5 levels from pre-infusion levels to 72 h (not shown). Thus, total MTXPG1–5 concentrations were calculated as the sum of pre-infusion values for MTXPG1–2 plus the average RBC MTXPG3 and RBC MTXPG4–5 measured from 0 to 72 h within each course. Figure 1c, d highlights the accumulation of RBC MTXPG in 17 patients (in one patient, RBC MTXPG levels were available at day 50). The changes in MTXPG1–5 over the interval period were best described by Michaelis–Menten kinetics (coefficient of determination ranged from 0.74 to 0.99) and with apparent plateau in total MTXPG by the 4th HDMTX infusion (6-weeks after the 1st infusion). In contrast, RBC MTXPG3 and MTXPG4–5 concentrations increased linearly (R2 ranged from 0.71 to 0.99) with a selective redistribution of MTXPG toward long-chain MTXPG4–5 which represented over 40% of total MTXPG at day 50 (Fig. 1d).
Methotrexate pharmacokinetics and MTXPG accumulation in children with ALL receiving HDMTX. Error bars represent standard deviations (SD). a Changes in MTX plasma concentrations during the first HDMTX infusion (day 8), b change in RBC MTXPG1 (MTX) and MTXPG2 during the first HDMTX infusion (day 8). MTXPG3–5 levels were undetectable, c accumulation of RBC MTXPG during interval therapy. HDMTX was administered at days 8, 22, 36, and 50 in 17 patients. Median MTXPG1–5 levels at day 50 were 20 pmol/109 cells (IQ range 15–29 pmol/109 RBC). Median MTXPG5 levels were 9 pmol/109 cells (IQ range 7–11 pmol/109 RBC), d change in the distribution of short chains (MTXPG1–2) long chains (MTXPG3) and very long chains (MTXPG4–5) MTXPG during interval therapy
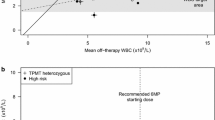
The impact of HDMTX on RBC thiopurine nucleotides concentrations following 76 HDMTX in 20 patients is presented in Table 1 and revealed a rapid decrease in RBC 6-TGN and 6-MMPN levels (nadir) within 24 h hours of HDMTX (compared to pre-HDMTX levels at 0 h; P < 0.001) and lasting for a minimum of 3 days. However, this reduction was followed by a return to baseline levels prior to the initiation of the following HDMTX course 14 days later (6-TGN: 114 ± 55 versus 184 ± 82 pmol/8 × 108 RBC; 6-MMPN: 1003 ± 985 versus 1351 ± 1307 pmol/8 × 108 RBC; P < 0.001, n = 60) (average ± SD). The change in RBC 6-TGN or 6-MMPN levels from initiation of HDMTX infusion to 72-h post-infusion was not associated with concomitant MTX peak plasma levels or RBC MTXPG concentrations (P > 0.09; not shown). A lack of greater activation of 6-MP to intracellular metabolites by consecutive HDMTX was evident (Fig. 2). A high inter-individual variability of RBC 6-thiopurine nucleotide levels was observed. No significant difference between pre-infusion levels measured after 8 days 6-MP (6-TGN: 177 ± 81 pmol/8 × 108 RBC; 6-MMPN: 1522 ± 1326 pmol/8 × 108 RBC) versus those measured after 22 days (6-TGN: 167 ± 82 pmol/8 × 108 RBC; 6-MMPN: 1338 ± 1101 pmol/8 × 108 RBC), 36 days (6-TGN: 199 ± 87 pmol/8 × 108 RBC; 6-MMPN: 1544 ± 1755 pmol/8 × 108 RBC), and 50 days (6-TGN: 184 ± 76 pmol/8 × 108 RBC; 6-MMPN: 1126 ± 848 pmol/8 × 108 RBC) (average ± SD; P > 0.14).
Impact of HDMTX infusions on 6-thiopurine disposition in RBC. Average pre-HDMTX infusion of RBC 6-TGN and 6-MMPN levels and nadir concentrations within 72-h post-infusion measured from day 8 to day 50 of interval therapy. Error bars represent standard deviations (SD). Dotted line corresponds to baseline and trough 6-TGN and 6-MMPN concentrations. Days of HDMTX infusion are indicated
Discussion
This study is the first to describe the build-up of MTXPG in the erythrocytic compartment following consecutive HDMTX courses and the second report to suggest a negative impact of HDMTX on 6-MP intracellular metabolism [10].
MTX is activated to MTXPG by a FPGS-mediated sequential addition of glutamic residues on MTX, and several studies have established that MTXPG accumulation in leukemic blasts or surrogate erythrocytes is associated with antileukemic effects [13, 14]. Our data indicate that the accumulation of MTXPG1–5 following consecutive HDMTX was slow, and the apparent plateau approaching steady state by the 6th-week therapy is consistent with previous reports with low weekly MTX dosage [15, 16]. During the first HDMTX course, the kinetics of RBC MTXPG1 (parent methotrexate) mirrored those of plasma MTX, and no MTXPG with greater than two glutamic residue was detected. These data substantiate the notion that the circulating erythrocytes do not produce significant MTXPG, and the low, albeit significant MTX di-glutamate formation observed during the first infusion probably reflected low polyglutamation from newly released reticulocytes from bone marrow. Alternatively, the subsequent elevation in RBC MTXPG3–5 likely reflected the pulsative release of MTXPG incorporated in bone marrow erythroid progenitors. Interestingly, the median RBC MTXPG1–5 levels measured at the initiation of the last HDMTX course was 20 pmol/109 cells, and these values are similar to those reported in RBC from children receiving weekly MTX dosages 125-fold lower (40 mg/m2: 29 pmol/109 cells) [9]. We explain these results by rate-limiting FPGS activity in marrow progenitors rather than saturation of MTX uptake (which is passive at higher dose MTX). However, HDMTX administration resulted in fourfold higher MTXPG5 levels (median 9.2 pmol/109 cells) by comparison with very long-chain MTXPG levels observed during weekly low-dose MTX during maintenance (median MTXPG5–7 was 2.4 pmol/109 cells) [9], and these data are consistent with the greater accumulation of long-chain MTXPG in bone marrow lymphoblasts following higher dose MTX [17]. Moreover, the percentage of very long-chain MTXPG4–5 (over 40% of the total MTXPG) following HDMTX courses was significantly higher than those reported following maintenance therapy of ALL (i.e., 18% MTXPG4–5 with a 20 g/m2 dosage) [9, 18]. Altogether, these data support the rational of administering HDMTX to produce longer chain MTXPG which are more potent inhibitors of de novo purine biosynthesis than short-chains MTXPG [17, 19].
The studies that directly investigated the impact of MTX on 6-thiopurine nucleotides (6-TGN and 6-MMPN) accumulation are in vivo very limited [9, 10], and the only trial that was specifically design to address the synergism between HDMTX and 6-MP metabolism (TOTAL XIIIb) surprisingly revealed that HDMTX (e.g., 1 g/m2) hampered the accumulation of intracellular 6-thiopurine nucleotides in bone marrow blasts, circulating blasts, and erythrocytes following IV 6-MP during upfront treatment of ALL [10]. In our study, the impact of HDMTX on 6-MP intracellular disposition was assessed in erythrocytes after a minimum of 8 days of continuous daily 6-MP, and thus at steady state concentration [20]. Our data consolidate and provide a valuable complement of the previous unexpected finding that HDMTX can negatively impact the intracellular metabolism of 6-MP. We observed a ~25% reduction in RBC 6-TGN and 6-MMPN levels within the first 72 h following the initiation of HDMTX with oral daily 6-MP, an effect remarkably similar to those reported in TOTALXIIIb (6-TGN: −35%; 6-MMPN: −29%) 20 h after initiation of intravenous 6-MP. However, we establish that the rapid reduction in RBC 6-MP metabolites by HDMTX which was sustained at least by the 3rd day post-HDMTX was followed by a recovery by the time of the next HDMTX infusion (14 days later). Several explanations were set forth [10] to explain the antagonism of HDMTX on 6-MP intracellular metabolism in TOTAL XIIIb, despite the significant de novo purine biosynthesis inhibition by MTX [17] and hence the likely elevation in PRPP levels [6]. In particular, an alteration in 6-MP uptake following tumor cell lysis and release of hypoxanthine (that competes with 6-MP for HPRT) was proposed, but this primary mechanism of cell lysis cannot hold given that our children were in remission [10]. We believe that alternative mechanisms including a selective efflux of 6-TGN and 6-MMPN is more likely to explain the results of this study and our.
It is important to note that in vitro studies in leukemic cell lines have reported an opposite effects of MTX on 6-TGN accumulation ranging from synergism at low-dose MTX (~twofold higher 6-TGN following 0.02 μM MTX) [21] to antagonism at much higher dosage (~2 lower fold higher 6-TGN following 40 μM MTX) [22], and it is tempting to suggest that MTX dose may produce differential effects on 6-TGN accumulation in vivo. Our contention is supported by the observation that low-dose MTX can enhance 6-TGN accumulation as seen during continuation therapy of ALL [9]. In addition, should HDMTX only transiently decrease 6-TGN levels by the time of its administration but in fine synergize with repetitive daily 6-MP dose, we should have observed an elevation in pre-infusion 6-TGN levels during the interval period. As we have not, we speculate that HDMTX does not synergize with 6-MP, while lower MTX dosage may enhance 6-MP activation to 6-thiopurine nucleotides. Whether these observations are clinically relevant is not know, but the reduction in 6-TGN accumulation in bone marrow lymphoblasts following HDMTX with intravenous 6-MP has been reported to be significantly greater (~13 fold) than those observed in red cells (~1.5 fold) during upfront therapy of ALL [10], and lower RBC 6-TGN are associated with lower antileukemic effects during maintenance of ALL [13, 23]. Clearly, these data cannot be ignored, and mechanisms of interaction between 6-MP and MTX are important to identify, not only to increase our knowledge on the transport, metabolism, and action of these drugs, but also to open new ways for treatment optimization and individualization.
Our data warrant additional studies assessing the duration of thioguanine levels suppression, the impact on their incorporation into DNA, the tolerance of increasing 6-MP dosage during HDMTX courses. Moreover, 6-MP and MTX transporters polymorphisms and/or expression might participate to inter-individual variability in both 6-thioguanine and MTXPG concentrations and also impact 6-TGN decrease. These investigations could help determine the dosing regimen for optimal clinical efficacy during interval therapy.
References
Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC et al (2009) Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med 360:2730–2741
Frei E III, Freireich EJ, Gehan E, Pinkel D, Holland JF et al (1961) Studies of sequential and combination antimetabolite therapy in acute lymphoblastic leukemia: 6-mercaptopurine and methotrexate. Blood 18:431–453
Lennard L (1992) The clinical pharmacology of 6-mercaptopurine. Eur J Clin Pharmacol 43:329–339
Gorlick R, Goker E, Trippett T, Waltham M, Banerjee D, Bertino JR (1996) Intrinsic and acquired resistance to methotrexate in acute leukemia. N Engl J Med 335:1041–1048
Bokkerink JP, Bakker MA, Hulscher TW, De Abreu RR, Schretlen ED, van Laarhoven JP, De Bruyn CH (1986) Sequence-, time- and dose-dependent synergism of methotrexate and 6-mercaptopurine in malignant human T-lymphoblasts. Biochem Pharmacol 35:3549–3555
Tan CT, Wollner N, Trippett T, Goker E, Tong WP, Kheradpour A et al (1994) Pharmacologic-guided trial of sequential methotrexate and thioguanine in children with advanced malignancies. J Clin Oncol 12:1955–1962
Lewis AS, Murphy L, McCalla C, Fleary M, Purcell S (1984) Inhibition of mammalian xanthine oxidase by folate compounds and amethopterin. J Biol Chem 259:12–15
Balis FM, Holcenberg JS, Zimm S, Tubergen D, Collins JM, Murphy RF, Gilchrist GS, Hammond D, Poplack DG (1987) The effect of methotrexate on the bioavailability of oral 6-mercaptopurine. Clin Pharmacol Ther 41:384–387
Dervieux T, Hancock M, Evans W, Pui CH, Relling MV (2002) Effect of methotrexate polyglutamates on thioguanine nucleotide concentrations during continuation therapy of acute lymphoblastic leukemia with mercaptopurine. Leukemia 16:209–212
Dervieux T, Hancock ML, Pui C-H, Rivera GK, Sandlund JT, Ribeiro R, Boyett J, Evans WE, Relling MV (2003) Antagonism of methotrexate on mercaptopurine disposition in lymphoblasts during up-front treatment of acute lymphoblastic leukemia. Clin Pharmacol Ther 73:506–516
Dervieux T, Boulieu R (1998) Simultaneous determination of 6-thioguanine and methyl 6-mercaptopurine nucleotides of azathioprine in red blood cells by HPLC. Clin Chem 44:551–555
Dervieux T, Orentas LD, Marcelletti J, Pischel K, Smith K, Walsh M, Richerson R (2003) HPLC determination of erythrocyte methotrexate polyglutamates after low-dose methotrexate therapy in patients with rheumatoid arthritis. Clin Chem 49:1632–1641
Schmiegelow K, Schroder H, Gustafsson G, Kristinsson J, Glomstein A, Salmi T, Wranne L (1995) Risk of relapse in childhood acute lymphoblastic leukemia is related to RBC methotrexate and mercaptopurine metabolites during maintenance chemotherapy. Nordic society for pediatric hematology and oncology. J Clin Oncol 13:345–351
Masson E, Relling MV, Synold TW, Liu Q, Schuetz JD, Sandlund JT, Pui CH, Evans WE (1996) Accumulation of methotrexate polyglutamates in lymphoblasts is a determinant of antileukemic effects in vivo. A rationale for high- dose methotrexate. J Clin Invest 97:73–80
Schroder H, Clausen N, Ostergaard E, Pressler T (1986) Pharmacokinetics of erythrocyte methotrexate in children with acute lymphoblastic leukemia during maintenance treatment. Cancer Chemother Pharmacol 16:190–193
Hendel J, Nyfors A (1984) Pharmacokinetics of methotrexate in erythrocytes in psoriasis. Eur J Clin Pharmacol 27:607–610
Dervieux T, Brenner TL, Hon YY, Zhou Y, Hancock ML, Sandlund JT et al (2002) De novo purine synthesis inhibition and antileukemic effects of mercaptopurine alone or in combination with methotrexate in vivo. Blood 100:1240–1247
Schroder H, Fogh K, Schrder H (1988) Methotrexate and its polyglutamate derivatives in erythrocytes during and after weekly low-dose oral methotrexate therapy of children with acute lymphoblastic leukemia. Cancer Chemother Pharmacol 21:145–149
Allegra CJ, Drake JC, Jolivet J, Chabner BA (1985) Inhibition of phosphoribosylaminoimidazolecarboxamide transformylase by methotrexate and dihydrofolic acid polyglutamates. Proc Natl Acad Sci U S A 82:4881–4885
Rostami-Hodjegan A, Lennard L, Lilleyman JS (1995) The accumulation of mercaptopurine metabolites in age fractionated red blood cells. Br J Clin Pharmacol 40:217–222
Giverhaug T, Loennechen T, Aarbakke J (1998) Increased concentrations of methylated 6-mercaptopurine metabolites and 6-thioguanine nucleotides in human leukemic cells in vitro by methotrexate. Biochem Pharmacol 55:1641–1646
Innocenti F, Danesi R, Di Paolo A, Loru B, Favre C, Nardi M, Macchia P, Del Tacca M (1996) Clinical and experimental pharmacokinetic interaction between 6-mercaptopurine and methotrexate. Cancer Chemother Pharmacol 37:409–414
Lennard L, Lilleman JS (1989) Variable mercaptopurine metabolism and treatment outcome in childhood lymphoblastic leukemia. J Clin Oncol 7:1816–1823
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adam de Beaumais, T., Dervieux, T., Fakhoury, M. et al. The impact of high-dose methotrexate on intracellular 6-mercaptopurine disposition during interval therapy of childhood acute lymphoblastic leukemia. Cancer Chemother Pharmacol 66, 653–658 (2010). https://doi.org/10.1007/s00280-009-1205-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-009-1205-4