Abstract
Purpose
We previously demonstrated the increase of reactive oxygen species (ROS) production and myeloperoxidase (MPO) activity in the small intestine of methotrexate (MTX)-treated rats. In the present study, we investigated the role of ROS modulating intestinal mucosal permeability in this damage.
Method
MTX (20 mg/kg body weight) was administered to rats intravenously. N-Acetylcysteine (NAC; 80 mg/kg body wt), an antioxidant and a precursor of glutathione (GSH) was administered to rats intraperitoneally to investigate the contribution of ROS to the intestinal permeability enhancement. Intestinal permeability was evaluated by determining that of a poorly absorbable marker, fluorescein isothiocyanate-labeled dextran (FD-4; average molecular mass, 4.4 kDa) using the in vitro everted intestine technique. The occurrence of oxidative stress in the small intestine was assayed by measuring chemiluminescence and thiobarbituric acid reactive substances (TBARS) productions in mucosal homogenates of the small intestine.
Results
The mucosal permeability of FD-4 significantly (p < 0.01) increased in MTX-treated rats compared with control rats, as demonstrated by a twofold increase of FD-4 permeation clearance. This suggests an increase in paracellular permeability. Interestingly, the ROS production was observed preceding the increase of paracellular permeability. Treatment with NAC prevented the MTX-induced ROS production and the increase of paracellular permeability.
Conclusions
NAC protected the small intestine of rats from MTX-induced change in paracellular permeability, suggesting that ROS played an important role in the enhanced paracellular permeability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methotrexate (MTX) is an anti-tumor drug that is effective for the treatment of acute leukemia, trophoblastic disease, and intraosseous sarcoma, and has recently been used as an antirheumatic drug [1, 2]. MTX antagonizes folate metabolism and inhibits the de novo synthesis of thymidine and purine, constituent factors of nucleic acid, resulting in the inhibition of proliferation of rapidly dividing cells such as cancer cells [3]. Because intestinal epithelial cells also divide rapidly, their proliferation is easily inhibited by MTX. MTX often causes mucosal inflammation of the mouth and intestine, leading to nausea and diarrhea [4, 5]. The mechanism for this side effect has not been completely clarified. Symptomatic therapy, such as with antibiotics and antidiarrheal drugs, has been used to reduce the side effects [6–8].
There are many studies about MTX-induced intestinal damage, and some of them demonstrated that simultaneous treatment of some growth factors, the antioxidants, and the nutrients with MTX protected the small intestine from this side effect. For example, keratinocyte growth factor [9], insulin-like growth factor-1 [10], and melatonin [11] stimulate regrowth of the damaged intestine and protect mice and rats from gastrointestinal injury. We also demonstrated a protective effect of retinol [12], docosahexaenoic acid [13], aged garlic extract [14], synthetic analogs of prostaglandin [15], and sodium tungstate [16] on MTX-induced intestinal damage.
MTX-induced intestinal damage is accompanied by a decrease in the function of intestinal barrier due to cell proliferation inhibition, and following invasion of xenobiotics and endotoxins. Accordingly, phagocytes, such as macrophages and neutrophils, infiltrate into the inflammatory region, and produce reactive oxygen species (ROS) [16, 17]. This is the well-known biophylaxis reaction. Chemotherapy-induced intestinal mucositis is now characterized by a five-phase model: (1) initiation, (2) upregulation and message generation, (3) signaling and amplification, (4) ulceration, and (5) healing [18]. In this model, ROS generation during the chemotherapy is the first step leading to intestinal inflammation. Moreover, the potential role of ROS in activation of nuclear factor-кB, an inflammatory-related transcription factor that upregulates inflammatory cytokines and adhesion molecules, is also suggested to be involved in intestinal inflammation.
The diseases such as inflammatory disease, cancer, ischemia–reperfusion injury, and diabetes, and the side effects of drugs like doxorubicin and cisplatin are related to oxidative stress [19, 20]. The protective effect of antioxidants for these side effects of anticancer drugs had been reported [21, 22]. On the other hand, ROS at very low concentration modulate the cell function and act as signal transmitter on apoptosis, cell proliferation, cell adhesion, and chemotaxis through regulation of nuclear transcription factors [23].
We reported an increase of intestinal paracellular permeability [24], ROS production [16, 25], neutrophil migration [16], and a decrease of intracellular glutathione (GSH) [16, 25] after MTX treatment in rats. Simultaneous use of prostaglandin E1 analogs [15], retinol [12] and aged garlic extract [14] prevented such a change in the intestinal paracellular permeability. N-Acetylcysteine (NAC), an antioxidant and a precursor of GSH, prevented such decreases of intracellular GSH and neutrophil migration [16].
ROS are reported to regulate the paracellular permeability and tight junction opening [26, 27]. The barrier function of tight junctions is maintained during neutrophil transepithelial migration, but high-density neutrophil migration can damage the integrity of epithelial cells [28, 29]. In this study, we intended to verify the hypothesis that the oxidative stress caused by the MTX treatment enhances intestinal paracellular permeability.
Materials and methods
Materials
MTX was kindly supplied from Wyeth Lederle Ltd. (Tokyo, Japan). NAC was purchased from Wako Pure Chemical Industry Ltd. (Osaka, Japan). FITC-dextran (average molecular weight, 4,400 Da; FD-4) was obtained from Sigma Chemical Company (St Louis, MO, USA). All other reagents were of analytical grade.
Animals
Male Wistar rats (7 weeks of age; Japan SLC Inc., Shizuoka, Japan) were housed under 12 h light/dark cycle at an ambient temperature of 25°C and given food (MF diet, standard laboratory diet commercially available, Oriental Yeast Company, Ltd., Tokyo, Japan) and water ad libitum. They were acclimatized for 1 week before starting experiments.
Drug treatments
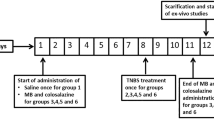
A single dose of MTX (20 mg/kg body weight) was injected intravenously into the rats. Control rats received the equivalent volumes of saline solution intravenously. NAC (80 mg/kg body wt) was injected to rats intraperitoneally at the same time with MTX administration. The treatment of rats was carried out as the following groups: saline solution (control), MTX alone, MTX and NAC, and NAC alone. Each group has 4 rats. All experiments were approved by the animal care committee of Chiba University.
FD-4 permeation in small intestine
Intestinal permeation was examined in vitro using everted segments of the small intestine, as described previously [24]. Rats were anesthetized with diethylether and their intestines were removed. Intestinal segments (14 cm) were cut out at a distance of 3 cm from the end of the duodenum. The segments were everted in ice-cold saline solution. A glass cannula was inserted into each end of the everted segment and a 10 cm plastic syringe was attached to the exposed end of each cannula as described by Doluisio et al. [30]. The segments were then placed in 40 mL of incubation medium (modified Krebs–Ringer bicarbonate–phosphate (mKRBP) buffer, pH 7.4) containing FD-4 at 37°C. Five milliliters of the buffer was added to the serosal side of the segments via the syringe. The plungers were gently moved up and down. Gas (95% O2–5% CO2) was gently bubbled into the buffer on the mucosal side during the absorption experiments. At designated times after the start of the experiments, 300 μL of sample solution was taken from the serosal side to determine the permeation of FD-4 and, at the same time, a similar volume of buffer was added to maintain the volume of the serosal side constant. Then, 30 μL of sample solution was taken from the mucosal side to determine the concentration of FD-4 in the mucosal side. The sample solutions taken from the serosal and mucosal sides were diluted with mKRBP buffer. The fluorescence intensity of FD-4 in the sample solutions was determined at an excitation wavelength of 495 nm and an emission wavelength of 515 nm using a Hitachi fluorescence spectrometer F-2000.
Data analysis
The permeation clearance and rate were determined as follows [24]:
where \( X_{{t_{1} }} \) and \( X_{{t_{2} }} \) are the amounts of marker substances permeated into the serosal side at incubation times, t 1 and t 2, respectively.
Preparation of small intestine homogenate
The rats were killed by decapitation at 24, 48, and 72 h after the treatment. The small intestine (about 40 cm in length from the end of the duodenum) was removed and washed with ice-cold saline solution. Immediately after the scraped mucosa from the intestine (about 30 cm length) was homogenized, chemiluminescence and TBARS in the homogenates were measured to evaluate the oxidative stress. The homogenates were used for the assays.
Chemiluminescence analysis
ROS production in the small intestine was evaluated by in vitro luminol-enhanced chemiluminescence as described previously [25]. In vitro experiments: intestinal mucosal scrapings (0.1 mg) were homogenized with 1 mL of ice-cold oxygenated carbonate buffer (50 mM, pH 9.0). The suspension was centrifuged at 15,000 rpm for 2 min by Beckmann Microfuge E™ and the supernatant was used for the assay. The samples were mixed with an incubation mixture containing 5 mM glucose and 400 μM luminol in phosphate buffered saline solution (PBS). The luminol-enhanced chemiluminescence from the samples was measured at 37°C using a single photoelectron counting system (Tohoku electronic Industries Co., Ltd., Sendai, Japan). The chemiluminescence was expressed as counts/min/mg protein by subtracting chemiluminescence of the incubation mixture only.
TBARS assay
Thiobarbituric acid reactive substances (TBARS) in intestinal mucosa were assayed by the method of Buege and Aust [31], and were expressed as nmol of malondialdehyde (MDA) equivalents per milligram protein. Briefly, the intestinal mucosa (0.1 mg) was homogenized with 1 mL of 15% trichloroacetic acid (TCA). Thiobarbituric acid (TBA) reagent (15% TCA, 0.375% TBA and 0.25 N HCl) (2 mL) was added to the mixture, followed by boiling for 15 min. The reaction mixture was then cooled and was centrifuged at 1,000g for 15 min. The absorbance of supernatant at 535 nm was determined with 1,1,3,3-tetraethoxypropane as the standard.
Statistical analysis
Statistical analysis was undertaken using two-way analysis of variance (ANOVA) followed by Turkey–Kramer’s post hoc test. A level of p < 0.05 was considered to be statistically significant.
Results
FD-4 permeation
The FD-4 permeation through the small intestine at 24, 48, and 72 h after the intravenous administration of MTX to rats was examined using the in vitro everted intestine technique. The FD-4 permeability was unaffected at 24 h after the MTX-treatment, but significantly increased, compared with the control at 48 h after the MTX-treatment (Fig. 1). The FD-4 permeability through the small intestine was the same as the control rats at 72 h after the MTX-treatment (data not shown). Permeation clearance of FD-4 in the small intestine at 48 h after the MTX-treatment was significantly higher than that of control rats, but it was unchanged at 24 (Fig. 2) and 72 h (data not shown).
Time course of FD-4 permeation in the small intestine of MTX-treated rats. FD-4 permeation in the in vitro everted small intestine was examined at 24 (a) and 48 (b) h after the intravenous administration of MTX to rats. Treatment: saline alone (open circle) and MTX (20 mg/kg body wt) (filled circle). Data represent mean ± SEM of 3–4 rats. *p < 0.05, **p < 0.01, significantly different from the control rats
Permeation clearance of FD-4 in the small intestine of MTX-treated rats in the in vitro everted intestine. FD-4 permeation in the in vitro everted small intestine was examined at 24 (a) and 48 (b) h after the i.v. administration of MTX to rats. Data represent mean ± SEM of 3–4 rats. *p < 0.05, significantly different from the control rats
NAC treatment
An antioxidant, NAC, was administered to rats to investigate the contribution of ROS to the intestinal permeability enhancement. Enhanced FD-4 permeability of the small intestine of rats at 48 h after the MTX-treatment as shown in Figs. 1b and 2b was significantly depressed by the treatment of NAC (Fig. 3). This finding indicated that ROS contributed to the MTX-induced intestinal paracellular permeability enhancement.
Effect of NAC on FD-4 permeation in the small intestine. FD-4 permeation in the in vitro everted small intestine was examined at 48 h after the intravenous administration of MTX and/or NAC to rats. Time course of FD-4 permeation (a) and permeation clearance of FD-4 (b) in the in vitro everted small intestine. Treatment: saline alone (open circle), MTX (20 mg/kg body wt) (filled circle), NAC (80 mg/kg body wt) (open square), and MTX with NAC (filled triangle). Data represent mean ± SEM of 4 rats. *p < 0.05, **p < 0.01, significantly different from the control rats. # p < 0.05, ## p < 0.01, significantly different from the MTX-treated rats
Oxidative stress
The oxidative stress in the small intestinal mucosa of rats at 24, 48, and 72 h after the MTX-treatment was evaluated by measuring chemiluminescence and TBARS. The chemiluminescence was used for detection of ROS production in the intestine. Luminol-enhanced chemiluminescence was detected in the homogenate of mucosal scrapings of the MTX-treated rats (Fig. 4). The chemiluminescence in the MTX-treated rats at 24 and 48 h after MTX treatment was significantly higher than that in the control rats, but at 72 h after MTX-treatment, it was almost the same counts as in the control rats (data not shown). The chemiluminescence reached a maximum intensity at 24 h after the MTX-treatment. The MTX treatment was found to produce ROS in the small intestine. TBARS formation showed a significant increase at 48 h after the MTX-treatment (Fig. 5) and was depressed by the treatment of NAC. It was not significantly different from that of control at 24 and 72 h (data not shown). The similar results were observed in chemiluminescence by the NAC treatment (data not shown).
Chemiluminescence emitted from the small intestine of rats. Rats were intravenously administered MTX. Luminol-enhanced chemiluminescence was detected in the homogenates of mucosal scrapings of rat small intestine at 24 (closed column) and 48 (open column) h after the MTX treatment. Data represent mean ± SEM of 3–4 rats. *p < 0.05, significantly different from the control rats. # p < 0.05, significantly different from the MTX-treated rats
TBARS production in the small intestine of rats. Rats were intravenously administered MTX and/or NAC. TBARS were detected in the homogenates of mucosal scrapings of rat small intestine at 24 (closed column) and 48 (open column) h after the MTX and/or NAC treatments. Data represent mean ± SEM of 5 rats. *p < 0.05, significantly different from the control rats
Body weight change
The time course of body weight of rats treated with MTX and/or NAC were measured for evaluation of toxicity induced by MTX (Fig. 6). Rat body weight was decreased at 24 and 48 h after the MTX treatment. It had a tendency to increase after that (data not shown). The MTX-induced decrease of body weight was not changed by the treatment of NAC.
Changes in body weight of rats. Treatment: saline alone (open circle), MTX (20 mg/kg body wt) (filled circle), NAC (80 mg/kg body wt) (open triangle), and MTX with NAC (filled triangle). Data represent mean ± SEM of 4–8 rats. *p < 0.05, **p < 0.01, significantly different from control rats, #p < 0.05, significantly different from MTX-treated rats
Discussion
Oral administration of MTX to rats and mice caused small intestinal damage and enhanced the permeation through the paracellular pathway of the small intestine [15, 24]. Since MTX is administered not only orally but also intravenously in clinical use, it is important to know how the different administration routes of MTX affect the small intestine. The effect of intravenous injection of MTX on the small intestine was examined using the permeation of the non-permeable macromolecule, FD-4, in the small intestine. FD-4 permeation of the small intestine increased at 48 h after a single intravenous injection of MTX to rats. The intravenous injection of MTX was also shown to affect the paracellular pathway of the small intestine, as was the oral administration. The permeation of FD-4 in the small intestine was not affected at 24 and 72 h after the intravenous injection of MTX to rats, which may be related to the turnover rate of small intestinal epithelial cells.
We reported that MTX administration in rats enhanced the production of ROS in small intestinal mucosa [16, 25]. MTX-induced enteritis was reported to be ameliorated by melatonin, having an antioxidant effect [11]. ROS is reported to activate tyrosinekinase and phosphatidylinositol3-kinase, and alter the localization of components of tight junctions [26, 27], resulting in change of the paracellular permeation. Thus, it is important to clarify whether ROS is related to the alteration of small intestinal permeation of MTX-treated rats.
MTX administration to rats decreased the intracellular GSH of intestinal epithelial cells [16]. The coadministration of NAC, the precursor of GSH, with MTX in rats preserved the FD-4 permeation of the small intestine to the level of that in rats treated with saline alone (control). This is possibly due to improvement of the intracellular redox state accompanied by the increased GSH and/or the antioxidative effect of NAC itself. Thus, ROS were shown to contribute to the increased permeation of the small intestine caused by MTX.
The occurrence of oxidative stress in the intestinal mucosa of rats treated with MTX was examined, using an ultraweak chemiluminescence instrument. The chemiluminescence was used for detection of ROS production in the intestine. Luminol-enhanced chemiluminescence was detected in the homogenate of intestinal mucosa of the MTX-treated rats. The chemiluminescence from the homogenates reached a maximum intensity at 24 h after MTX administration to rats and its intensity was still high even at 48 h. The coadministration of NAC with MTX to rats depressed the ROS production to the control level at 24 and 48 h after MTX treatment. Following ROS production, lipid peroxidation occurred, as shown by the production of TBARS. TBARS produced in the intestinal mucosa significantly increased at 48 h after MTX treatment in rats. The TBARS production was depressed by the coadministration of NAC with MTX to rats. We previously reported that the activity of myeloperoxidase, which is a marker enzyme of glanulocytes and reflects the neutrophil infiltration in intestinal mucosa, increased at 48 h after the MTX administration to rats, but not at 24 h [16]. Thus, the enhanced ROS production at 24 h shown in this study seems not to originate from inflammatory cells like neutrophils at the inflammation site.
As shown here, the paracellular permeation of the small intestine was altered followed by the ROS production. Under oxidative stress conditions, it is reported that the epithelial paracellular permeability is altered by the change in localization of occludin and ZO-1, which compose tight junctions [27]. Therefore, the change of protein localization in tight junctions is reported to be mediated by tyrosine phosphorylation [27, 32]. Such molecular mechanisms in tight junctions are under investigation to further elucidate the mechanism of enhanced permeation of paracellular pathway in the small intestine of MTX-treated rats.
MTX treatment decreased the body weight of rats at 24 and 48 h. However, since the coadministration of NAC with MTX did not prevent their loss, such loss of body weight may possibly be caused by the action of MTX itself rather than by the generated ROS. On the other hand, the MTX treatment of rats increased the FD-4 permeation of the small intestine at 48 h and the treatment of NAC with MTX prevented this enhancement of intestinal permeability, suggesting that the enhanced permeability of the small intestine is due to ROS.
Aged garlic extract has been shown to prevent the damage of the small intestinal epithelial cells caused by MTX [33, 34]. To perform effective MTX therapy for cancer treatment, it is important to develop a method of treatment to prevent MTX-induced small intestinal damage, including finding protective substances like aged garlic extract.
In conclusion, the present study has clearly shown that the MTX-induced ROS plays an important role in the enhancement of paracellular permeability of small intestine in the MTX-induced intestinal damage of rats.
References
Thomas HJ (1987) Searching for magic bullet: early approaches to chemotherapy-antifolate, methotrexate. Cancer Res 47:5528–5536
Rosen G, Caparros B, Huvos AG, Kosloff C, Nirenberg A, Cacavio A, Marcove RC, Lane JM, Mehta B, Urban C (1982) Preoperative chemotherapy for osteogenic sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor to preoperative therapy. Cancer 49:1221–1230
Ortiz Z, Shea B, Suarez-Almazor ME, Moher D, Wells GA, Tugwell P (1998) The efficacy of folic acid and folinic acid in reducing methotrexate gastrointestinal toxicity in rheumatoid arthritis. A metaanalysis of randomized controlled trials. J Rheumatol 25:36–43
Taminiau JA, Gall DG, Hamilton JR (1980) Response of the rat small-intestine epithelium to methotexate. Gut 21:486–492
Pinkerton CR, Cameron CH, Sloan JM, Glasgow JF, Gwevava NJ (1980) Jejunal crypt cell abnormalities associated with methotrexate treatment in children with acute lymphoblatic leukaemia. J Clin Pathol 35:1272–1277
Beck PL, Wong JF, Li Y, Swaminathan S, Xavier RJ, Devaney KL, Podolsky DK (2004) Chemotherapy- and radiotherapy-induced intestinal damage is regulated by intestinal trefoil factor. Gastroenterology 126:796–808
Khan SA, Wingard JR (2001) Infection and mucosal injury in cancer treatment. NCI Monogr 29:31–36
Keefe DM, Schubert MM, Elting LS, Sonis ST, Epstein JB, Raber-Durlacher JE, Migliorati CA, McGuire DB, Hutchins RD, Peterson DE (2007) Mucositis Study Section of the Multinational Association of Supportive Care in Cancer and the International Society for Oral Oncology updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer 109:820–831
Gibson RJ, Keefe DM, Clarke JM, Regester GO, Thompson FM, Goland GJ, Edwards BG, Cummins AG (2002) The effect of keratinocyte growth factor on tumour growth and small intestinal mucositis after chemotherapy in the rat with breast cancer. Cancer Chemother Pharmacol 50:53–58
Howarth GS, Cool JC, Bourne AJ, Ballard FJ, Read LC (1998) Insulin-like growth factor-I (IGF-I) stimulates regrowth of the damaged intestine in rats, when administered following, but not concurrent with, methotrexate. Growth Factors 15:279–292
Jahovic N, Sener G, Cevik H, Ersoy Y, Arbak S, Yegen BC (2004) Amelioration of methotrexate-induced enteritis by melatonin in rats. Cell Biochem Funct 22:169–178
Tsurui K, Kosakai Y, Horie T, Awazu S (1990) Vitamin A protects the small intestine from methotrexate-induced damage in rats. J Pharmacol Exp Ther 253:1278–1284
Horie T, Nakamaru M, Masubuchi Y (1998) Docosahexaenoic acid exhibits a potent protection of small intestine from methotrexate-induced damage in mice. Life Sci 62:1333–1338
Horie T, Matsumoto H, Kasagi M, Sugiyama A, Kikuchi M, Karasawa C, Awazu S, Itakura Y, Fuwa T (1999) Protective effect of aged garlic extract on the small intestinal damage of rats induced by methotrexate administration. Planta Med 65:545–548
Gao F, Nakamaru M, Masubuchi Y, Horie T (2001) Protective effect of a synthetic analog of prostaglandin E1 on the small intestinal damage induced by the administration of methotexate to rats. J Pharm Sci 90:1040–1048
Miyazono Y, Gao F, Horie T (2004) Oxidative stress contributes to methotrexate-induced small intestinal toxicity in rats. Scand J Gastroenterol 39:1119–1127
Gao F, Ueda S, Horie T (2001) Effect of a synthetic analog of prostaglandin E1 on the intestinal mucosa of methotrexate-treated rats. Anticancer Res 21:1913–1917
Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, Bekele BN, Raber-Durlacher J, Donnelly JP, Rubenstein EB (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100:1995–2025
Quiles JL, Huertas JR, Battino M, Mataix J, Ramirez-Tortosa MC (2002) Antioxidant nutrients and adriamycin toxicity. Toxicology 180:79–95
Conklin KA (2000) Dietary antioxidants during cancer chemotherapy: impact on chemotherapeutic effectiveness and development of side effects. Nutr Cancer 37:1–18
Dehne N, Lautermann J, Petrat F, Rauen U, de Groot H (2001) Cisplatin ototoxicity: involvement of iron and enhanced formation of superoxide anion radicals. Toxicol Appl Pharmacol 174:27–34
Hagiwara SI, Ishii Y, Kitamura S (2000) Aerosolized administration of N-acetylcysteine attenuates lung fibrosis induced by bleomycin in mice. Am J Respir Crit Care Med 162:225–231
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Nakamaru M, Masubuchi Y, Narimatsu S, Awazu S, Horie T (1998) Evaluation of damaged small intestine of mouse following methotrexate administration. Cancer Chemother Pharmacol 41:98–102
Gao F, Horie T (2002) A synthetic analog of prostaglandin E(1) prevents the production of reactive oxygen species in the intestinal mucosa of methotrexate-treated rats. Life Sci 71:1091–1099
Sheth P, Basuroy S, Li C, Naren AP, Rao RK (2003) Role of phosphatidylinositol 3-kinase in oxidative stress-induced disruption of tight junctions. J Biol Chem 278:49239–49245
Rao RK, Basuroy S, Rao VU, Karnaky KJ Jr, Gupta A (2002) Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem J 368(Pt 2):471–481
Edens HA, Levi BP, Jaye DL, Walsh S, Reaves TA, Turner JR, Nusrat A, Parkos CA (2002) Neutrophil transepithelial migration: evidence for sequential, contact-dependent signaling events and enhanced paracellular permeability independent of transjunctional migration. J Immunol 169:476–486
Zen K, Parkos CA (2003) Leukocyte-epithelial interactions. Curr Opin Cell Biol 15:557–564
Doluisio JT, Billups NF, Dittert LW, Sugita ET, Swintosky JV (1969) Drug absorption I: an in situ rat gut technique yielding realistic absorption rates. J Pharm Sci 58:1196–1200
Buege JA, Aust SD (1978) Microsomal lipid peroxidation. Methods Enzymol 52:302–310
Hartsok A, Nelson WJ (2008) Adherens and tight junctions: structure, function and connections to the actin cytoskeleton. Biochim Biophys Acta 1778:660–669
Li T, Ito K, Sumi S-I, Fuwa T, Horie T (2005) Antiapoptosis action of aged garlic extract (AGE) protects epithelial cells from methotrexate induced injury. Gut 54:1819–1820
Li T, Ito K, Sumi S-I, Fuwa T, Horie T (2009) Protective effect of aged garlic extract (AGE) on the apoptosis of intestinal epithelial cells caused by methotrexate. Cancer Chemother Pharmacol 63:873–880
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, T., Miyazono, Y., Ito, K. et al. Oxidative stress and enhanced paracellular permeability in the small intestine of methotrexate-treated rats. Cancer Chemother Pharmacol 65, 1117–1123 (2010). https://doi.org/10.1007/s00280-009-1119-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-009-1119-1