Abstract
Background
There is no standard first-line therapy for advanced gastric and gastroesophageal junction (GEJ) adenocarcinoma and the prognosis remains poor. Our institution conducted a phase I study of oxaliplatin, irinotecan, and capecitabine given in a novel, weekly schedule. The regimen was tolerated; pharmacodynamic studies revealed no drug interactions, and there was one confirmed response in a gastric cancer patient. We performed a phase II trial in advanced gastric and GEJ adenocarcinoma to determine response rate and response duration.
Methods
This was a multi-center single treatment arm study involving six sites. Only prior adjuvant therapy was allowed. Patients had ECOG performance status of 0–2, adequate organ function, and were able to tolerate oral medications. All patients received oxaliplatin 60 mg/m2 intravenously (IV) and irinotecan 50 mg/m2 IV weekly times 4 weeks with a 2-week rest period. Capecitabine 450 mg bid orally was received on days 1 through 5 every week for 4 weeks, followed by a 2-week rest. Patients were assessed for response after the first two cycles; response duration, overall survival, and adverse events were also recorded. We estimated an improvement in historical response rate by 30% would have clinical meaning.
Results
A total of 39 patients were accrued and all were assessed for toxicity; 30 patients were evaluable for response. The median age was 57.8 years (31–79 years) and 74% were male. Two patients had a complete response, with nine patients achieving a partial response. The total response rate was 28%, with nine patients not evaluable for response. The median response duration was noted at 5.97 months and median overall survival was 8.98 months. There were no grade 5 treatment related events, with all deaths secondary to disease progression. Only five grade 4 events occurred (neutropenia, hyperkalemia, hypokalemia (2), thrombosis/embolism) without grade 4 diarrhea or sensory neuropathy.
Conclusions
Oxaliplatin, irinotecan, and capecitabine given in a novel, weekly schedule does induce responses in advanced gastric and GEJ adenocarcinoma. However, the total response rate is modest and not an improvement over other regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Effective therapy for advanced gastric adenocarcinoma remains elusive, despite the high world-wide prevalence. In the United States for the year 2007, approximately 21, 260 new cases of gastric carcinoma are expected with approximately 11, 210 deaths [10]. All patients with inoperable or metastatic disease have a dismal 5-year survival of less than 10% [8]. Discovering regimens with significant survival benefits is requisite.
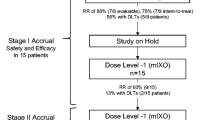
Our institution conducted a phase I study of oxaliplatin, irinotecan and capecitabine to find the maximum tolerated dose and dose limiting toxicity (DLT) of this combination [13]. Pharmacokinetics (PK) for all three agents were assessed and at least one woman was accrued to each cohort, based on reports of disproportionate adverse events with 5-fluorouracil/capecitabine when compared to men [2, 20]. The regimen was found to be equally well-tolerated in both women and men with DLT of diarrhea. Response was evaluated in 17 patients, with a confirmed complete response noted in a patient with gastric carcinoma. These agents have been beneficial in other combinations and dosing schedules in gastric carcinoma. PK data did not reveal any untoward drug interactions. First-line systemic treatment approach to gastric and gastroesophageal junction (GEJ) carcinoma is not established; therefore, we conducted a phase II study in advanced gastric and GEJ with this triple-drug regimen. Based on our phase I data, we evaluated this weekly schedule of more dose-dense treatment for efficacy and toxicity.
Patients and methods
Eligibility
Patients were required to have metastatic or inoperable pathologically confirmed adenocarcinoma of the stomach or GEJ (Siewert classification type I–III) [19]). Prior chemotherapy for metastatic disease was not allowed, but adjuvant or neoadjuvant chemotherapy and/or radiation therapy was permissible, as long as 4 weeks had elapsed since these prior therapies. Patients had to be age 18 years or older with a life expectancy of at least 12 weeks. Measurable disease by RECIST criteria [22] was required.
All patients were mandated to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2 and be able to tolerate oral medications. Adequate hematologic (hemoglobin ≥ 9.5 g/dL, ANC ≥ 1500/µL and platelet count ≥ 100,000/µL) and hepatorenal (total bilirubin ≤ 1.5 mg/dL; AST and ALT ≤ two times the upper limit of normal (ULN); creatinine clearance ≥ 60 mL/minute/1.73 m2 if serum creatinine above the ULN) were required for study entry. Exclusion criteria consisted of inability to take oral medications, New York Heart Association classification III or IV heart disease, brain metastases or primary brain tumors, pregnancy or lactation, and known hypersensitivity to 5-FU or compounds similar in structure to oxaliplatin or irinotecan.
Written informed consent forms were approved by Cancer Therapy Evaluation Program at the National Cancer Institute, by the Institutional Review Board of University Hospitals Case Medical Center, and by participating institutions review boards. Consent was signed by all participating patients.
Study design and dosing
Patients were required to have a routine history, physical exam, and radiographic tumor staging before treatment. One cycle was 6 weeks: 4 weeks of treatment with 2 weeks rest. Patients were assessed for response after cycle two by history, physical exam, and radiographic studies. Patients tolerating treatment with responding or stable disease were able to continue on study, with re-staging performed after every even-numbered cycle. Treatment was discontinued in patients with progressive disease; these patients were then monitored for survival.
All patients received oxaliplatin 60 mg/m2 intravenously (IV) and irinotecan 50 mg/m2 IV weekly times 4 weeks with a 2-week rest period. Capecitabine 450 mg bid orally was received on days 1 through 5 every week for 4 weeks, followed by a 2-week rest. Oxaliplatin (NSC 266064) was provided by the Division of Cancer Treatment, Diagnosis and Centers, NCI, (Bethesda, MD) as a lyophilized powder in vials containing 50 or 100 mg of oxaliplatin. The powder was reconstituted by adding 10 mL (for the 50 mg vial) or 20 mL (for the 100 mg vial) of water for injection or 5% dextrose in water, yielding a 5 mg/mL solution, which was diluted in an infusion solution of 250–500 mL 5% dextrose in water. Irinotecan and capecitabine were obtained from commercially available sources.
Supportive care and dose modifications
Antiemetics including steroids plus prochlorperazine or a 5-HT3 receptor antagonist were administered before each dose of oxaliplatin. Oral antiemetics and anti-diarrheal agents were discussed with each patient. Growth factor support was employed at the discretion of the treating physician, but was in accordance with American Society of Clinical Oncology guidelines.
Toxicity was graded according to Common Terminology Criteria for Adverse Events version 2.0. The start of a new cycle could be delayed as long as 3 weeks to allow toxicities to return to a grade 1 or better; the absolute neutrophil count had to be at least 1,250/mm3. During a cycle, treatment could be held as long as 2 weeks and re-instituted when myelosuppression returned to a grade 2 or better and non-hematological toxicities were a grade 1 or better.
Dose modifications were specified. If a course of treatment was complicated by grade 3 mucositis/diarrhea or grade 4 myelosuppression/febrile neutropenia, then the irinotecan dose was reduced by 20% to 40 mg/m2. If a second treatment was complicated by these factors, then the oxaliplatin dose was reduced by 20% to 48 mg/m2 and the capecitabine dose was reduced by 33% to 300 mg orally bid. A third episode of these toxicities resulted in removal from the study.
Statistical analysis
This clinical trial employed Simon’s MinMax two-stage design to study the primary objective of total response rate. Based on the literature, there is an estimated 50% total response rate to many multi-agent regimens for advanced gastric adenocarcinoma [16, 18, 26]. We estimated an improvement in this historical response rate by 30%, which would yield a total response rate of 65% for our regimen to have clinical meaning. With α = 0.10 and β = 0.10 (power = 0.90), 19 of the first 40 patients must respond to continue accrual to a total of 72 patients. All patients, except those who did not receive any chemotherapy, were analyzed for response. Kaplan–Meier methods were used to analyze the secondary endpoint of response duration and overall survival using a historical control of 7 months [16, 18, 26].
Results
Patient chararcteristics
This was a multi-center single treatment arm study involving four academic sites and two community partner institutions. A total of 39 patients were accrued from February 2004 to February 2007; the study was closed before a 40th patient could be accrued due to statistical inability to obtain the required 19 responses. See Table 1 for patient characteristics.
Adverse events
All 39 patients were evaluated for toxicity. Study related adverse events (AE) are summarized in Table 2 and are categorized by grade. There were no grade 5 related events, with all patient deaths secondary to disease progression. Only five grade 4 events occurred (neutropenia, hyperkalemia, hypokalemia (2), thrombosis/embolism) without grade 4 diarrhea or sensory neuropathy.
Constitutional symptoms accounted for 77% (n = 30) of treatment related AE experienced; 79% (n = 31) of patients complained of gastrointestinal effects. Only 15% (n = 6) experienced stomatitis and there was one episode of febrile neutropenia. Treatment-related diarrhea, mainly grade 1 occurred in 69% (n = 27) with hypokalemia experienced by 31% (n = 12) of patients.
Baseline symptoms were recorded for 33 patients, with an average of 5 baseline symptoms per patient. Over the course of the study, 28% of patients were taken off study due to AE or other complications. For patients who completed one cycle of therapy, the median number of cycles received was three, with a range of 1–12.
Response rate and survival
Two patients had a complete response, with nine patients achieving a partial response. See Table 3 for response rate data; the total response rate was 28% with 23% (n = 9) of patients not evaluable for response. Reasons for inability to assess response include patient withdrawal before the end of cycle 2 for non-disease and non-treatment related issues (N = 4), withdrawal before the end of cycle 2 with death 2–9 days after stopping treatment due to disease (N = 3), progressive non-measurable disease (pleural effusion N = 1), and physician withdrawal for patient noncompliance (N = 1). The secondary objective of median response duration was noted at 5.97 months. Median overall survival was 8.98 months with 95%CI (6.85, 13.31) months (see Fig. 1) and progression-free survival was 5.38 months 95%CI 3.38, 8.46) months (see Fig. 2) with three patients alive at last data analysis.
Discussion
The incidence of stomach/GEJ adenocarcinoma has remained essentially stable over the past few years, except for the known increase in GEJ and distal esophagus adenocarcinomas in the United States, starting in approximately 1975 [5, 25]. The higher incidence of adenocarcinoma of the stomach/GEJ coincides with increased rates of gastroesophageal reflux disease, obesity, and tobacco abuse. The pathogenesis of adenocarcinoma includes multiple environmental factors, such as Helicobacter pylori infections, and genetic mutations of p53, p27, E-cadherin, and others with activation of cellular epidermal and vascular proliferative pathways [11]. Some consider these particular mutations lead to a more aggressive entity. The standard of care or reference regimen for clinical trials varies by geography due to international differences in screening, surgical approach, and subsequently the natural history. Systemic treatment improves mortality over best supportive care [25] and doublet or triplet regimens are accepted as superior to single agents [25].
In the United States, cisplatin (CDDP) and fluorouracil (5-FU) in combination (CF) is among the most frequently employed treatment, due to improved progression-free survival (PFS) [12, 24]. Epirubicin, cisplatin, and infusional 5-FU (ECF) is another regimen, widely used in the United Kingdom, based on overall survival improvement seen against 5-fluorouracil, leucovorin, doxorubicin and methotrexate (FAMTX) [16, 26]. A randomized, international trial of docetaxel, cisplatin, and continuous infusion 5-FU (DCF) or CF was recently completed and the primary objective of improved time to progression with DCF was achieved. Also, there was a significant improvement in overall survival between the two regimens of over half a month (9.2 vs. 8.6 months, P = 0.0201) [23].
In this population of potentially debilitated patients, the toxicity of a triple-drug regimen could be problematic. Currently, a randomized trial of DCF with growth factor support versus a modified DCF regimen is under way to answer the question of clinical feasibility (MSKCC 06-103 http://www.clinicaltrials.gov). At this time, DCF and ECF and are the only regimens from randomized clinical trials with statistically superior overall survival (OS) from the comparator therapies. However, a large randomized non-inferiority trial with a two by two design assessed different permutations of ECF, including the parent regimen and substitutions of capecitabine for 5-FU and oxaliplatin for CDDP. The hazard ratio for death was consistent with non-inferiority for the use of capecitabine and oxaliplatin. Overall survival was a secondary objective and favored epirubicin, oxaliplatin, and capecitabine at 11.2 months (EOX) over ECF at 9.9 months (HR 0.80, 95% confidence interval 0.66–0.97, P = 0.002) [3]. EOX does eliminate the need for venous access and continuous 5-FU infusion, which may be more desirable for many patients. Irinotecan-based trials are also ongoing; although an abstract describing a weekly schedule of irinotecan and 5-FU/LCV with continuous infusion 5-FU for 24 h versus CF was superior only in having fewer adverse events [4].
Our triple-drug regimen of oxaliplatin, irinotecan and capecitabine did not distinguish itself with regard to response rate, although response rate is not necessarily a correlate for survival. The study’s primary aim targeting a 30% increase in response rate as compared to the literature was a venerable goal; a median survival of 9 months is consistent with reports with other regimens. The total response rate did not exceed expected rates for reasons that may include the 56% rate of ECOG PS 1–2 patients and a weekly dosing schedule requiring multiple trips to the clinic; 15% (N = 7) patients withdrew after starting treatment. Pharmacokinetic studies from the phase I study by Krishnamurthi et al. did not reveal any abnormal drug interactions; however, since many patients did have a prior gastrectomy or gastric bypass, it is feasible that capecitabine absorption was altered in this population. The most likely reason for non-statistical significance in our trial is that cytotoxic agents alone are simply ineffectual therapy.
Oxaliplatin, irinotecan and capecitabine does not appear to be noticeably different from the other regimens. However, it appeared to be well-tolerated except for a high rate of grade 3 diarrhea. This study reiterated the known ability of cytotoxic agents in combination to impart a good response rate and survival rate in some patients. Multiple randomized trials have elucidated response rates of 42–45% for ECF [16, 26] 21–41% FAMTX [26, 27] 37% for DCF [23] 25–34% for 5-FU/cisplatin [23] and 48% for EOX [3]. S-1 has been studied in Japan with great success in phase II studies, but results of JCOG 9912 versus 5-FU versus irinotecan and CDDP are pending. Comparison between American and Japanese patients should occur with caution, given the differing surgical approaches and natural history, drug availability, and genetic polymorphisms.
Although some phase II studies are obtaining an approximately 50% response rate and current cytotoxic agent-only combinations such as DCF and EOX report median survivals of 9–11 months [3, 23], overall survival does not appear to be significantly changing. Novel agents and altered dosing schedules are possible alternative strategies for this disease. This study utilized a schedule with lower doses per each treatment and a more frequent administration, similar in structure to metronomic chemotherapy administration; however, the 2-week rest period would argue against this designation [9]. FOLFOX-4 (bi-weekly oxaliplatin, infusional 5-FU and leucovorin) has been tested in phase II studies for this patient population, with an essentially equivalent doses of oxaliplatin over 6 weeks (255 mg/m2 in FOLFOX-4 and 240 mg/m2 in this study) and reports of less diarrhea, neutropenia, and less frequent chemotherapy administration than this regimen [1, 6]. A more manageable toxicity profile is one attractive component of novel dosing therapies [21] and alternative drug administration schedules should continue to be assessed.
As the molecular pathogenesis of gastric carcinoma becomes more apparent, it is reasonable to target therapies to these perturbations. For example, it is known that the expression of the vascular endothelial growth factor receptor (VEGF) is linked to a poor prognosis [28]. A phase II trial of the VEGFR inhibitor bevacizumab in combination with irinotecan and cisplatin displayed provocative results with a median survival of 12.2 months [17]. Currently, there are multiple angiogenesis inhibitors being assessed in phase I and II clinical trials for solid tumors (i.e., bevacizumab, sunitinib, vatalanib, NPI-2358; see http://www.cancer.gov/search/clinical_trials).
Additionally, inhibition of the epidermal growth factor receptor (EGFR), as well as nuclear factor kappa-B, have been attempted in several studies with variable results [7, 14, 15]. The utilization of cytotoxic therapies needs to be maximized; agents that disrupt the cellular pathways and genetic mutations controlling gastric/GEJ adenocarcinoma should be added to these drugs with the goal of improving survival.
References
Al-Batran SE, Atmaca A, Hegewisch-Becker S et al (2004) Phase II trial of biweekly infusional flurouracil, folinic acid, and oxaliplatin in patients with advanced gastric carcinoma. J Clin Oncol 22:658–663
Chansky K, Benedetti J, Macdonald JS (2005) Differences in toxicity between men and women treated with 5-fluorouracil therapy for colorectal carcinoma. Cancer 103:1165–1171
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR, Upper Gastrointestinal Clinical Studies Group of the National Cancer Research Institute of the United Kingdom (2008) Capecitabine and oxaliplatin for advanced esophagogastric Cancer. N Engl J Med 358:36–46
Dank M, Zaluski J, Barone C, Valvere V, Peschel C, Wenczl E, Goker M, Risse M, Awad L, Bugat R (2005) Randomized phase 3 trial of irinotecan + 5FU/folinic acid vs CDDP + 5FU in first-line advanced gastric cancer patients. J Clin Oncol 23:308s abstr 4003
Devesa SS, Blot WJ, Fraumeni JF Jr (1998) Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83:2049–2053
DeVita F, Orditura M, Matano E et al (2005) Phase II trial of biweekly oxaliplatin plus infusional 5-flurouracil and folinic acid (FOLFOX-4) as first-line therapy of advanced gastric carcinoma patients. Br J Cancer 92:1644–1649
Dragovich T, McCoy S, Fenoglio-Preiser CM, Wang J, Benedetti JK, Baker AF, Hackett CB, Urba SG, Zaner KS, Blanke CD, Abbruzzese JL (2006) Phase II trial of erlotinib in gastroesophageal junction and gastric adenocarcinomas: SWOG 0127. J Clin Oncol 24:4922–4927
Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, Morrow M (2002) AJCC Cancer staging manual, Chap. 10, 6th edn. Springer-Verlag, New York, p 112
Hahnfeldt P, Folkman J, Hlatky L (2003) Minimizing long-term tumor burden: logic for metronomic chemotherapeutic dosing and its angiogenesis basis. J Theor Biol 220:545–554
Jemel A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer statistics. CA Cancer J Clin 57:43–66
Keller G, Hofler H, Becker KF (2005) Molecular medicine of gastric adenocarcinomas. Expert Rev Mol Med 7:1–13 Review
Kim Ni, Park YS, Hedo DS, Suh C, Kim SY, Park KC, Kang YK, Shin DB, Kim HT, Kim HJ (1993) Phase III randomized study of 5-fluorouracil and cisplatin versus 5-fluorouracil, doxorubicin, and mitomycin C versus 5-fluorouracil alone in the treatment of advanced gastric cancer. Cancer 71:3813–3818
Krishnamurthi SS, Brell JM, Hoppel CL, Egorin MJ, Weaver KC, Li X, Ingalls ST, Zuhowski EG, Schluchter MD, Dowlati A, Cooney MM, Gibbons J, Overmoyer BA, Ivy SP, and Remick SC (2008) Phase I clinical trial and pharmacokinetic study of oxaliplatin, irinotecan, and capecitabine. Cancer Chemother Pharmacol Apr 15 [Epub ahead of print]
Ocean AJ, Schnoll-Sussman F, Keresztes R, Chen X, Holloway S, Matthews N, Christos P, Mazumdar M, Wright J, Wadler S (2006) Phase II study of PS-341 (bortrezominb) with or withour irinotecan in patients with advanced gastric adenocarcinomas. ASCO annual meeting proceedings. J Clin Oncol 24:14040
Pinto C, Di Fabio F, Siena S, Cascinu S, Rojas Llimpe FL, Ceccarelli C, Mutri V, Giannetta L, Giaquinta S, Funaioli C, Berardi R, Longobardi C, Piana E, Martoni AA (2006) Phase II study of cetuximab in combination with FOLFIRI in patients with untreated advanced gastric or gastroesophageal junction adenocarcinoma (FOLCETUX study). Ann Oncol 18:510–517
Ross P, Nicolson M, Cunningham D, Valle J, Seymour M, Harper P, Price T, Anderson H, Iveson T, Hickish T, Lofts F, Norman A (2002) Prospective randomized trial comparing mitomycin, cisplatin and protracted venous-infusion fluorouracil (PVI 5-FU) with epirubicin, cisplatin, and PVI 5-FU in advanced esophagogastric cancer. J Clin Oncol 20:1996–2004
Shah MA, Ramanathan RK, Ilson DH, Levnor A, D’Adamo D, O’Reilly E, Tse A, Trocola R, Schwartz L, Capanu M, Schwartz GK, Kelsen DP (2006) Multicenter phase II study of irinotecan, cisplatin, and bevacizumab in patients with metastatic gastric or gastroesophageal junction adenocarcinoma. J Clin Oncol 20:5201–5206
Shirao K, Shimada Y, Kondo H, Saito D, Yamao T, Ono H, Yokoyama T, Fukuda H, Oka M, Watanabe Y, Ohtsu A, Boku N, Fujii T, Oda Y, Muro K, Yoshida S (1997) Phase I-II study of irinotecan hydrochloride combined with cisplatin in patients with advanced gastric cancer. J Clin Oncol 15:921–927
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85:1457–1459
Sloan JA, Goldberg RM, Sargent DJ, Vargas-Chanes D, Nair S, Cha SS, Novotny PJ, Poon MA, O’Connell MJ, Loprinzi CL (2002) Women experience greater toxicity with fluorouracil-based chemotherapy for colorectal cancer. J Clin Oncol 20:1491–1498
Suvannasankha A, Fausel C, Juliar BE, Yiannoutsos CT, Fisher WB, Ansari RH, Wood LL, Smith GG, Cripe LD, Abonour R (2007) Final reports of toxicity and efficacy of phase II study or oral cyclophosphamide, thalidomide, and prednisone for patients with relapsed or refractory multiple myeloma: a Hoosier Oncology Group Trial, HEM01-21. Oncologist 12:99–106
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors: European Organization for Research and Treatment of Cancers, National cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni C, Rodrigues A, Fodor M, Chao Y, Voznyi E, Risse ML, Ajani JA, V325 Study Group (2006) Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: report of the V325 Study Group. J Clin Oncol 24:4991–4997
Vanhoefer U, Rougier P, Wilke H, Ducreux MP, Lacave AJ, Van Cutsem E, Planker M, Santos JG, Piedbois P, Paillot B, Bodenstein H, Schmoll HJ, Bleiberg H, Nordlinger B, Couvreur ML, Baron B, Wils JA (2000) Final results of a randomized phase III trial of sequential high-dose methotrexate, fluorouracil, and doxorubicin versus etoposide, leucovorin, and fluorouracil versus infusional fluorouracil and cisplatin in advanced gastric cancer: a trial of the European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. J Clin Oncol 81:2648–2657
Wagner AD, Grothe W, Haerting J, Kleber G, Grothey A, Fleig W (2006) Chemotherapy in advanced gastric cancer: systemic review and meta-analysis based on aggregate data. J Clin Oncol 24:2903–2909
Webb A, Cunningham D, Scarffe JH, Harper P, Norman A, Joffe JK, Hughes M, Mansi J, Findlay M, Hill A, Oates J, Nicolson M, Hickish T, O’Brien M, Iveson T, Watson M, Underhill C, Wardley A, Meehan M (1997) Randomized trial comparing epirubicin, cisplatin, and fluorouracil versus fluorouracil, doxorubicin, and methotrexate in advanced esophagogastric cancer. J Clin Oncol 15:261–267
Wils JA, Klein HO, Wagener DJ, Bleiberg H, Reis H, Korsten F, Conroy T, Fickers M, Leyvraz S, Buyse M (1991) Sequential high-dose methotrexate and fluorouracil combined with doxorubicin—a step ahead in the treatment of advanced gastric cancer: a trial of the European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cooperative Group. J Clin Oncol 9:827–831
Zhao HC, Qin R, Chen XX, Sheng X, Wu JF, Wang DB, Chen GH (2006) Microvessel density is a prognostic marker of human gastric cancer. World J Gastroenterol 21:7598–7603
Acknowledgments
Supported by NIH grant U01 CA62502.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brell, J.M., Krishnamurthi, S.S., Javle, M. et al. A multi-center phase II study of oxaliplatin, irinotecan, and capecitabine in advanced gastric/gastroesophageal junction carcinoma. Cancer Chemother Pharmacol 63, 851–857 (2009). https://doi.org/10.1007/s00280-008-0807-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-008-0807-6