Abstract
Background
Fluoropyrimidine based therapy has modest activity in patients with metastatic renal carcinoma and inhibition of ribonucleotide reductase is synergistic in model systems. GTI-2040 is a 20-mer phosphorothioate oligonucleotide complimentary to the R2 component of ribonucleotide reductase that has activity in renal cancer models.
Methods
Metastatic renal carcinoma patients without prior fluoropyrimidine therapy and normal organ function were treated with oral capecitabine 880 mg/m2 twice daily along with continuous infusion GTI-2040 starting at 148 mg/m2/day for 21 days, for each 28-day cycle. After completion of the phase I portion, the phase II study portion sought to rule out a null hypothesized 10% response rate versus an alternative 25% response rate utilizing α and β errors of 0.05 and 0.2, respectively. GTI-2040 pharmacokinetics and effects on ribonucleotide reductase expression in peripheral mononuclear cells were evaluated in a subset of patients.
Results
Based on one dose limiting toxicity in nine patients in the phase I portion, the phase II portion was conducted using the previously recommended 185 mg/m2/day dose of GTI-2040. Twenty-six patients were enrolled in the phase II portion to obtain 18 fully evaluable for response. Only one patient, treated at a GTI 2040 dose of 185 mg/m2/day in the phase I portion of the protocol, responded. Toxicities and GTI-2040 pharmacokinetics were consistent with previously reported results. R2 expression in peripheral mononuclear cells was too variable for accurate interpretation.
Conclusion
Further study of GTI-2040 and capecitabine in metastatic renal cancer at this dose and schedule is not indicated. Further study is necessary to determine whether lack of activity is due to inadequate target inhibition or inadequate effect of appropriate targeting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite recent dramatic advances in the treatment of metastatic renal cancer with oral VEGFR/PDGFR tyrosine kinase inhibitors and mTOR inhibitors, therapy for these patients remains inadequate. These new agents, although leading to improved progression free and likely overall survival, have not led to complete responses and essentially all patients eventually progress [1, 2]. In fact, the only potential curative therapy for patients with metastatic renal cancer is high dose IL-2, which is poorly tolerated and leads to a complete response in only 4–8% of a select population [3, 4]. It thus remains critical to identify novel systemic treatments for this disease.
Traditionally renal cell cancer is considered resistant to standard cytotoxic, or DNA targeted, therapy. Nevertheless, use of fluoropyrimidines has led to low but reproducible objective response rates [5]. The combination of fluorouracil, or the oral analog capecitabine, with gemcitabine may be particularly effective, perhaps through inhibition of ribonucleotide reductase, but no randomized data demonstrating a clear advantage over a fluoropyrimidine alone exist [6–8]. To this end a combination of a fluoropyrimidine with other potentially synergistic agents is worthy of investigation.
GTI-2040 is a 20-mer phosphorothioate oligonucleotide complimentary to the R2 component of ribonucleotide reductase [9]. Ribonucleotide reductase catalyzes the synthesis of 2′-deoxyribonucleotides from their corresponding ribonucleotide 5′-diphosphate. This is the rate limiting reaction in the production of 2′-deoxyribonucleotide triphosphates necessary for DNA replication. The R2 component of ribonucleotide reductase is regulated differentially throughout the cell cycle, being highest during late G1 and early S-phase, and requires the stably expressed R1 component to form a fully active ribonucleotide reductase enzyme [10]. Finally, R2 is overexpressed in cancer cells and in experimental systems contributes to drug resistance [11].
Preclinical studies of GTI-2040 suggested potent antitumor activity especially in renal cell carcinoma models [9]. Toxicology and pharmacokinetic studies further suggested that GTI-2040 would be safe in humans at doses predicted to inhibit ribonucleotide reductase (data on file, Lorus Therapeutics). A phase I clinical study of GTI-2040 in solid tumor patients has been reported [12]. The recommended phase II dose was 185 mg/m2/day by continuous infusion for 21 days on a 28-day cycle, with dose limiting toxicities being fatigue and transient elevation of serum hepatic transaminases. Biochemical evidence of complement activation was also noted at the highest doses and was associated with elevated transaminases. Pharmacokinetics of GTI-2040 were quite variable with mean steady state levels of 0.63 μg/ml at the recommended phase II dose, which is theoretically sufficient for inhibiting ribonucleotide reductase as determined in model systems [9]. Based on these considerations a phase I/II trial of GTI-2040 and capecitabine was initiated in patients with advanced renal carcinoma.
Methods
Patients
Patients were required to have histologic/cytologic confirmation of metastatic renal cancer without limitation to any histologic subtype, as well as measurable disease on standard radiologic imaging as defined by the usual RECIST criteria [13]. Karnofsky performance status needed to be at least 70%, and patients needed to have adequate organ function defined by normal PT/PTT, hemoglobin >10.0 g/dl, WBC >3.0/μl, neutrophil count >1,500 cells/μl, platelet count >80,000/μl, creatinine ≤1.6 mg/dl, bilirubin <1.5 mg/dl, and AST and ALT <2 times the upper limit of normal. There was no limitation on prior therapy except for the exclusion of patients previously treated with any antisense drug or fluoropyrimidine. Any prior therapy must have been completed at least 28 days prior to enrollment and pregnancy and/or patients unwilling to comply with a contraceptive regimen were exclusion criteria. Other exclusions included a prior non-renal cell malignancy diagnosed within the previous 5 years, a serious bleeding tendency, use of aspirin, or significant infection. The clinical protocol was approved by each institution’s IRB and every patient provided written informed consent.
Treatment
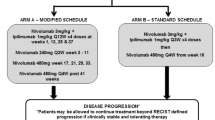
Patients were treated with oral capecitabine 1,660 mg/m2/day divided into two daily doses and rounded to the nearest whole tablet size along with continuous infusion GTI-2040 for 21 days, for each 28-day cycle. The initial GTI-2040 dose level was 148 mg/m2/day with a planned escalation to the phase II recommended dose of 185 mg/m2/day if fewer than two of six patients experienced dose-limiting toxicities in cycle 1. Dose reductions of capecitabine were also specified if more than two of six patients experienced a dose limiting toxicity at the starting dose levels. Dose limiting toxicities were defined as grade 4 neutropenia lasting 3 days or longer or grade 3/4 neutropenia associated with fever, grade 4 thrombocytopenia or grade 3 thrombocytopenia associated with hemorrhage, grade 3 elevated PT/PTT, delay of at least fourteen days in initiating the second cycle of therapy due to persistent treatment related toxicity grade 2 or greater, and any grade 3/4 non-hematologic toxicity except alopecia, gastrointestinal toxicity, or palmar plantar erythrodysesthesia. Protocol specified dose modifications were also made for grade 3 or 4 hematologic toxicity, grade 2 or greater palmar plantar erythrodysesthesia, and grade 2 or greater diarrhea or mucositis. Disease reevaluation by radiologic imaging was performed every 8 weeks and patients continued treatment until documented progression, serious toxicity, or patient withdrawal.
Pharmacokinetics and pharmacodynamics
Blood samples for pharmacokinetic analysis were collected from all patients at the first dose level and from the initial 12 patients at the recommended phase 2 dose at 1, 2, 3, 4 and 6 h after initiating GTI 2040 therapy, and at 0.25, 0.5, 1, 2, 4, and 6 h after initiating the infusion and prior to the end of infusion on day 22. Steady state levels were also obtained on day 8 and 15 of cycle 1 and day 1 of cycle 2. Analysis was performed as previously described [14].
Blood samples for RT-PCR evaluation of R1 and R2 ribonucleotide reductase expression were collected at baseline and on day 22. Erythrocytes were immediately lysed and the leukocyte pellet frozen at −80°C prior to shipping for central analysis. Real-time quantitative RT-PCR analysis was performed using TaqMan® Gene Expression Assay (Applied Biosystems) for both R1 and R2 ribonucleotide reductase relative to expression of the TATA box binding protein (TBP) mRNA using standard methodologies.
Statistics
The size of the phase II portion of the trial was based on a target activity level of 25% with a null hypothesis of 10%. The null hypothesis was based on reported activity of 5FU and capecitabine regimens in the literature and degree of improvement felt to be necessary to justify further evaluation of a continuous infusion regimen. An initial 18 patients were to be accrued and further accrual of an additional 25 patients planned if there were more than two responders in the initial cohort. At least 8 responders out of the final 43 patients were required for further study of this combination based on an α = 0.05 and a power of 80% [15]. Survival and time to progression were calculated using Kaplan–Meier statistics.
Results
In the initial phase I portion of the protocol none of the first three patients treated with 145 mg/m2/day GTI 2040 and one of six treated at 185 mg/m2/day experienced dose limiting toxicity (Grade 3 diarrhea). For the phase II portion, 26 patients were enrolled; two were found to be ineligible on central review and never received any study treatment, five were treated but found to be ineligible on retrospective review, and one patient stopped treatment due to toxicity prior to the first disease re-evaluation, thus leaving 18 patients fully evaluable by protocol definitions for efficacy. The five treated patients found to be ineligible had an elevated PT and/or PTT (3 pts), an elevated creatinine of 1.7 mg/dl (1 pt), or prior therapy with 5-fluorouracil (1 pt). Characteristics of all 33 treated patients are provided in Table 1. None of the patients in the phase II portion of the study and only one patient treated at a GTI 2040 dose of 185 mg/m2/day in the phase I portion of the protocol had an objective response and thus further accrual was halted. Maximal tumor change by RECIST criteria of the 30 patients with at least 2 radiologic evaluations is depicted in Fig. 1. One patient with a greater than 30% decrease in baseline lesion measurements also developed new lesions and was thus characterized as progressive disease.
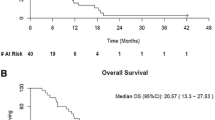
The median time to progression was 3.1 months and the median survival was 12.1 months (data not shown). Major toxicity is depicted in Table 2 and is consistent with previously reported toxicities of each agent alone. All of the cardiovascular and the majority of the infectious complications were felt to be unrelated or unlikely related to study treatment by the investigator. Only one patient had evidence of elevated hepatic transaminases (grade 2) and seven had evidence of prolonged PT and/or PTT, none of which led to any significant bleeding episodes.
Pharmacokinetic parameters exhibited high inter-patient variability (Table 3). At the phase II dose of 185 mg/m2 the mean and relative coefficient of variation for GTI-2040 AUC and t 1/2 were 1073 (35%) μg-hr/ml and 0.952 h (68%), respectively. The estimated mean (%CV) steady state concentration of GTI-2040 at 185 mg/m2 was 2.29 (26%) μg/ml. For pharmocodynamic analysis, only ten adequate paired samples were obtained and baseline R2/TBP ratios varied widely making interpretation of any changes with therapy impossible.
Discussion
In this study the combination of GTI-2040 and capecitabine was found to be tolerable with the spectrum and severity of the toxicities similar to that expected with capecitabine or GTI-2040 alone. Unfortunately, the response rate did not meet pre-specified criteria for further investigation of this combination. Even under the most conservative interpretation, only 1 of 18 (6%) patients in the phase II portion of the study responded. This is consistent with the response rate seen in a multi-institutional study of continuous infusion fluorouracil [16]. The change in tumor size also did not suggest a major disease stabilizing effect of the regimen. Likewise, time to progression and survival are consistent with previously reported studies of refractory renal cancer patients treated with inactive agents [17]. Although a multi-institutional study of capecitabine plus gemcitabine demonstrated an 11% response rate, it is difficult to compare results across studies and determine whether this truly represents an advantage [7].
The explanation for the limited responses is unclear. The enrolled patient population does not appear to have any worse prognostic features than reported in other trials for refractory renal cancer. The steady state levels of GTI-2040 observed were theoretically sufficient to inhibit ribonucleotide reductase while the observed toxicity does not suggest that patients received an inadequate drug exposure [9]. The pharmacodynamic studies were not adequate enough to determine whether consistent inhibition of ribonucleotide reductase R2 was achieved in circulating mononuclear cells. Degree of inhibition of tumor ribonucleotide reductase R2 is thus a matter of speculation Nevertheless, the combination of GTI-2040 and capecitabine, at these doses and schedules, is not recommended for further evaluation in renal cancer.
References
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, Hutson TE, Gore M, Freeman S, Schwartz B, Shan M, Simantov R, Bukowski RM (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Motzer R J, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356:115–124
Fyfe G, Fisher RI, Rosenberg SA, Sznol M, Parkinson DR, Louie AC (1995) Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J Clin Oncol 13:688–696
McDermott DF, Regan MM, Clark JI, Flaherty LE, Weiss GR, Logan TF, Kirkwood JM, Gordon MS, Sosman JA, Ernstoff MS, Tretter CP, Urba WJ, Smith JW, Margolin KA, Mier JW, Gollob JA, Dutcher JP, Atkins MB (2005) Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol 23:133–141
George CM, Stadler WM (2003) The role of systemic chemotherapy in the treatment of kidney cancer. In: Figlin R (eds) Kidney cancer. Kluwer, Norwell
Heinemann V, Schulz L, Issels RD, Plunkett W (1995) Gemcitabine: a modulator of intracellular nucleotide and deoxynucleotide metabolism. Semin Oncol 22:11–18
Stadler WM, Halabi S, Rini B, Ernstoff MS, Davila E, Picus J, Barrier R, Small EJ (2006) A phase II study of gemcitabine and capecitabine in metastatic renal cancer: a report of cancer and leukemia group B protocol 90008. Cancer 107:1273–1279
Stadler WM, Huo D, George C, Yang X, Ryan CW, Karrison T, Zimmerman TM, Vogelzang NJ (2003) Prognostic factors for survival with gemcitabine plus 5-fluorouracil based regimens for metastatic renal cancer. J Urol 170:1141–1145
Lee Y, Vassilakos A, Feng N, Lam V, Xie H, Wang M, Jin H, Xiong K, Liu C, Wright J, Young A (2003) GTI-2040, an antisense agent targeting the small subunit component (R2) of human ribonucleotide reductase, shows potent antitumor activity against a variety of tumors. Cancer Res 63:2802–2811
Nocentini G (1996) Ribonucleotide reductase inhibitors: new strategies for cancer chemotherapy. Crit Rev Oncol Hematol 22:89–126
Huang A, Fan H, Taylor WR, Wright JA (1997) Ribonucleotide reductase R2 gene expression and changes in drug sensitivity and genome stability. Cancer Res 57:4876–4881
Desai AA, Schilsky RL, Young A, Janisch L, Stadler WM, Vogelzang NJ, Cadden S, Wright JA, Ratain MJ (2005) A phase I study of antisense oligonucleotide GTI-2040 given by continuous intravenous infusion in patients with advanced solid tumors. Ann Oncol 16:958–965
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada (see comments). J Natl Cancer Inst 92:205–216
Zhang W, Leighl N, Zawisza D, Moore MJ, Chen EX (2005) Determination of GTI-2040, a novel antisense oligonucleotide, in human plasma by using HPLC combined with solid phase and liquid–liquid extractions. J Chromatogr B Analyt Technol Biomed Life Sci 829:45–49
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10
Kish JA, Wolf M, Crawford ED, Leimert JT, Bueschen A, Neefe JR, Flanigan RC (1994) Evaluation of low dose continuous infusion 5-fluorouracil in patients with advanced and recurrent renal cell carcinoma. A Southwest Oncology Group Study. Cancer 74:916–919
Motzer RJ, Bacik J, Schwartz LH, Reuter V, Russo P, Marion S, Mazumdar M (2004) Prognostic factors for survival in previously treated patients with metastatic renal cell carcinoma. J Clin Oncol 22:454–463
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stadler, W.M., Desai, A.A., Quinn, D.I. et al. A Phase I/II study of GTI-2040 and capecitabine in patients with renal cell carcinoma. Cancer Chemother Pharmacol 61, 689–694 (2008). https://doi.org/10.1007/s00280-007-0524-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0524-6