Abstract
Objectives
To study the toxicity and efficacy of weekly paclitaxel and carboplatin (PC-W) in women with primary ovarian cancer
Methods
This investigation extended a phase-I dose finding study and was approved by the institutional review boards of all participating institutions. Between 1999 and 2003, women with radically resected ovarian cancer of FIGO stages II B to IV were enrolled at 17 German centres. Patients received weekly paclitaxel at a dose of 100 mg/m2, followed by carboplatin AUC 2. After a first treatment block consisting of six cycles of chemotherapy, patients had a treatment-free interval of 14 days, followed by a second block of six cycles. Treatment was completed by a 28-days break and a final block of six cycles.
Results
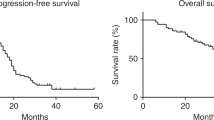
Altogether, 129 women with a mean age of 59 ± standard deviation 11 years entered the study. Most patients (82.9%) had serous papillary carcinoma of FIGO stage III (72.9%) and IV (20.9%). Participants received 1,851 cycles of chemotherapy; averaging 14.3 ± 4.3 cycles each patient. PC-W produced low rates of peripheral neuropathy (grade 3: 2.3%, 95% confidence interval [CI] 0.5–6.6%), with rapid recovery after 3 months. However, 72 patients had grade III/IV anaemia (55.8%, 95% CI 46.8–64.5%). There were 36 events of grade III/IV leukopenia (27.9%, 95% CI 20.4–36.5%). One patient sustained neutropenic fever. CA-125- and objective response was noted in 73.9% (95% CI 64.7–81.8%) and 55.6% (95% CI 41.4–69.1%) of patients. Median progression free and overall survival was 21 and 43 months, respectively.
Conclusions
PC-W is feasible; a randomized study is warranted to compare this new regimen with conventional 3-weekly treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First-line treatment of ovarian cancer demands aggressive resection followed by adjuvant chemotherapy.
In a recent randomized trial of the Gynaecologic Oncology Group (GOG) with more than 4,500 patients, the addition of other chemotherapeutic agents to the established paclitaxel and carboplatin combination failed to improve progression free or overall survival [1]. Thus, until new, innovative compounds will be available on the market, paclitaxel and carboplatin given every 3 weeks remain the undisputed standard of care [2–10]. Rather than changing or adding drugs, the cytotoxic properties of this regimen may, however, be improved by modifying its schedule or route of administration. Specifically, optimizing pharmacokinetics may aid in overcoming the challenge of platinum-resistance.
Preclinical data indicate that duration of exposure is one of the most important predictors of cell death. Xenograft models suggested an additive anti-angiogenic effect with low-dose paclitaxel infusions [11–19]. Exposing solid tumours with long doubling times continuously to a high concentration of cytotoxic agents may enhance the chance of killing malignant clusters during the cell cycle.
Increasing the total dose is associated with higher rates of grade III and IV haematological and non-haematological toxicity. Another way of intensifying drug exposure is to administer chemotherapy more frequently, for example, by a weekly schedule.
We had previously demonstrated in a phase-I study that weekly paclitaxel and carboplatin (PC-W) can be applied safely as first-line and salvage chemotherapy to patients with ovarian cancer [20]. We found 100 mg/m2 of paclitaxel and carboplatin at AUC 2 to be the maximum tolerated dose in this setting. To allow for more robust conclusions about safety, and to gain an impression on the efficacy with the weekly schedule, we proceeded with an exploratory phase-II study. We had objectives in describing the toxicity profile, response and survival rates with the new PC-W regimen.
Patients and methods
Study design
In this multi-centre phase II study, we enrolled patients with histologically confirmed epithelial ovarian cancer of FIGO stages II B to IV. Patients had undergone primary surgery with the aim of maximal tumour reduction. The institutional review boards of the participating centres approved this study, and all patients provided written informed consent.
Eligibility rules resembled those defined in the previous phase-I study. Patients were required to have all of the following inclusion criteria: a life expectancy of more than 3 months with an Eastern Cooperative Oncology Group (ECOG) performance status ≤2; a glomerular filtration rate (GFR) greater than 60 ml/min, or serum creatinine levels below 1.6 mg/dl; liver transaminases less than two times the normal levels, and bilirubin concentrations below 1.5 mg/dl and adequate bone marrow function as indicated by a leukocyte count greater than 4,000/μl, and a platelet count greater than 100,000/μl. Patients suffering from secondary malignancy or concurrent serious, uncontrolled medical or psychiatric disease were excluded from this study, as were subjects receiving other chemo-, immune-, or hormonal therapy.
The target dose of paclitaxel depended on the body surface area (BSA). The carboplatin dose was computed according to Calvert’s formula [21], and is expressed as the equating area under the curve (AUC, mg/ml × min). The GFR was estimated using Jellife’s equation [22], which accounts for patient’s age, gender, weight, and serum creatinine.
The detailed treatment protocol has been published elsewhere [20]. Briefly, 100 mg/m2 of paclitaxel was delivered as 1.0–1.5 h infusion (in 500 ml of 5% glucose solution), and carboplatin AUC 2 (distribute in 250 ml 0.9% saline) as 0.5 h infusion via a venous port. Intravenous premedication consisting of clemastine 2 mg, ranitidine 50 mg, dexamethasone 12 mg, and a 5-HT3-antagonist was administered 15 min prior to the chemotherapy.
The first treatment block consisted of six cycles of chemotherapy, administered on a weekly basis with a subsequent 14-day break. This was followed by another six cycles of chemotherapy. After a treatment-free interval of 28 days, patients received another three cycles. Additional cycles could be delivered if the patient experienced at least partial response, and wanted to undergo further treatment. Therapy duration of less than 12 doses of chemotherapy was considered premature termination.
Toxicity
Toxicity was graded according to the National Cancer Common Toxicity Criteria [23]. Patients did not receive primary supportive granulocyte-colony-stimulating factors (G-CSF). Secondary G-CSF prophylaxis was provided in case of a treatment delay caused by severe leucopenia or neutropenic fever. Patients were withdrawn from the protocol if they experienced grade 3 or 4 (excluding alopecia and nausea grade 3) toxicity, or had treatment delays of more than 2 weeks.
Efficacy
Response in patients with bi-dimensionally measurable tumours was defined according to the criteria of the International Union Against Cancer (UICC) and was determined by physical examination and ultrasound, CT, or MRI scan before the seventh and thirteenth course of chemotherapy. If the patient responded to therapy (i.e., partial or complete response), the same examination method was repeated for confirmation. Response in subjects without measurable lesions was determined by the CA-125 assay alone [24, 25].
Statistical analysis
The institutional review board mandated commencing a phase-II investigation in case of promising preliminary findings of the dose-finding study. This was arranged to consolidate estimates, and to strengthen conclusions before proceeding with a randomized trial. We posed no formal null hypothesis, and toxicity and efficacy were handled as equitable endpoints for non-confirmative analyses. We strived for a sample size in the typical range of phase-II designs, that is, between 75 and 150 patients. Since we aimed at determining objective response, at least 25% of all patients were required to have a macroscopic residual tumour mass ≥2 cm. Recruitment was stopped after this prevalence was reached in a consecutive cohort of patients.
We tabulated means, medians, and proportions with their adequate measures of distribution. We computed 95% confidence intervals (CI) for toxicity and response rates. Kaplan–Meier analysis was performed to determine the probability of progression-free and overall survival.
Results
Between March 1999 and April 2003, 129 women with histological proven ovarian cancer were enrolled at 17 German cancer canters after primary surgery. Mean age was 59 years ± standard deviation 11 years. Most patients (82.9%) had serous papillary carcinoma of FIGO stage III (72.9%) and IV (20.9%). Demographic details are listed in Table 1.
Participants received 1,851 cycles of chemotherapy; averaging 14.3 ± 4.3 cycles each patient. Overall, 67.4% of patients received at least 12 cycles of chemotherapy, and 57.4% received at least 15 cycles.
Details on toxicity are provided in Table 2. We noted a high incidence of grade 3 and 4 anaemia. Fifty-six patients (43.4%, 95% CI 34.7–52.4%) needed a median of 2 (range 0–12) units of packed erythrocytes. Twenty patients received erythropoietin (15.5%, 95% CI 9.7–22.9%). Three patients required transfusion of platelet concentrates. Secondary G-CSF prophylaxis was administered to 49 patients (38.0%, 95% CI 29.6–46.9%). We noted one episode of neutropenic fever (0.8%, 95% CI 0.0–4.2%). No patient developed sepsis.
There were no unexpected adverse drug effects, or therapy-related deaths. Toxicity required reducing the paclitaxel dose to 80 mg/m2 in four patients. Another three patients had to continue treatment with lowered carboplatin doses.
A treatment delay of 1 week or longer occurred in 47 cycles (2.8%, 95% CI 2.1–3.7%).
Forty-three patients (33.3%, 95% CI 25.3–42.2%) terminated treatment early because of 19 haematological and 9 non-haematological toxic events. Logistic reasons and patients’ decisions resulted in further six and two withdrawals. In six patients, treatment was discontinued because of tumour progression.
Except alopecia, severe non-haematological toxicity was rare. Of note, only three patients encountered grade 3 neurotoxicity. Peripheral sensory neuropathy of any grade, although reported by 71% of all patients immediately after treatment, resolved rapidly over time (see Fig. 1).
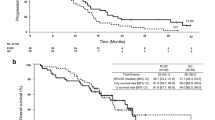
Thirty of 54 patients with measurable disease had complete or partial response (55.6%, 95% CI 41.4–69.1%). Of 111 patients with elevated CA-125 concentrations at study entry, 82 normalized during treatment (response rate 73.9%, 95% CI 64.7–81.8%). Figure 2 displays pre- and post-treatment tumour marker levels.
Median progression-free survival was 22 months (95% CI 17–27). Median overall survival was 45 (95% CI 33–57) months. Results of univariate survival analyses are displayed in Fig. 2. Overall survival meets estimates from published randomized trials of 3-weekly chemotherapy [9, 10]. Figure 3 illustrates the similarity in Kaplan–Meier-estimates (Fig. 4).
Residual disease, performance status, and the number of delivered cycles contributed independently to the probability of survival. The findings from Cox regression analysis are summarized in Table 3.
Discussion
In this reasonably large cohort of patients, PC-W was associated with a high incidence of grade III and IV haematological toxicity. Progression-free and overall survival rates curtailed the expectations from in vitro and preliminary clinical evidence, and did not exceed those reported for conventional treatment.
Weekly chemotherapy is commonly prescribed in patients with relapsed ovarian cancer, and other solid tumours. Phase-II studies showed response rates about 25% in patients with relapsed ovarian cancer and resistance to first-line, 3-weekly platinum and paclitaxel [26–28]. In a randomized trial, weekly administration was less toxic than the conventional 3-weekly schedule [3]. Previous investigations strived for lower paclitaxel doses (that is, 60–80 mg/m2) than those applied in the present protocol but they have not performed a dose-finding study and patients were all pre-treated with platinum-based chemotherapy [29].
In our previous phase-I study different doses of weekly paclitaxel and carboplatin were analysed for defining the dose limiting toxicities and the maximal tolerated dose (MTD) of this new regimen [20]. So, consequently we used the dose of 100 mg/m2 for paclitaxel and AUC 2 for carboplatin. Nevertheless, there are only preclinical studies but no phase-III data available, which have showed any clinically relevant dose–response effect for higher doses of paclitaxel or carboplatin. In a study of 330 patients previously treated with first-line platinum-based combination chemotherapy were treated with either 175 mg/m2 over 24 h every 3 weeks or 250 mg2 over 24 h plus G-CSF support [30]. The higher dose produced a higher response rate (36 vs. 28%), but no differences in progression free survival or overall survival were observed. Moreover, phase II trials have not shown convincing evidence indicating a role for high-dose chemotherapy in advanced ovarian cancer. Based on the experience in relapsed ovarian cancer we believe that a weekly dose of 80 mg/m2 of paclitaxel induce the same response rate as a higher dose of 90 or 100 mg/m2 but associated with a better toxicity profile. Nevertheless, there are no randomized studies available which have defined the best dose for weekly paclitaxel in patients with ovarian cancer.
Furthermore, only few data are available on weekly treatment for primary disease. In a recent study, Safra et al. [31] assigned 37 women with stage I C to IV epithelial ovarian, tubal or primary peritoneal carcinoma to weekly carboplatin and 80 mg/m2 of paclitaxel. Patients received, on average, six cycles of chemotherapy. Grade 3 and 4 neutropenia were recorded in five (13.5%) and one patient (2.7%), respectively. Thus, severe neutropenia occurred in 16.2% (95% CI 6.2–32.0%) of cases, compared to an incidence of 55.8% (95% CI 46.8–64.5%) noted in our investigation. With an incidence of zero and one case, patients in both studies had a negligible risk for neutropenic fever.
Response rates were displayed inconsistently in Safra’s study. Although 26 and 7 of 33 women with measurable disease were reported to have achieved complete and partial response, 13 and 1 had progressed or died by the time of data collection. So, the rate of complete and partial response was 19/33, or 57.6% (95% CI 39.2–74.5%), which exactly meets the response rate observed in our patient sample.
With a median time to progression of only 7.5 months, and lacking estimates of overall survival, no valid conclusions can be drawn about the efficacy of Safra’s approach. The authors stress the low rate of grade 3 neurotoxicity (2/37, or 5.4% [95% CI 0.7–18.2%]) with PC-W, which is in line with our results. However, grade 3 neuropathy is a similarly rare complication with 3-weekly administration of paclitaxel and carboplatin.
The incidence of grade 2 and 3 neuropathy in patients treated with conventional paclitaxel and carboplatin was estimated at 13% [32]. In a reanalysis of the Multicenter Italian Trial in Ovarian cancer (MITO-4) [33], 65 of 120 women (54.2%) had at least grade 1 neurotoxicity during chemotherapy. The incidence of sensory grade 2 and 3, and motor grade 1 toxicity was 13/120 (10.8%), 1/120 (0.8%), and 3/120 (2.5%). Of note, 46 of 60 patients (76.7%) fully recovered, mostly within 6 months after end of treatment. Assuming that five women lost to follow-up still had neuropathy, patients may be assured of a 70% chance for complete resolution of symptoms. Also, only 2 (2.3%) and 3 (5.0%) participants had sensory grade 2 and motor grade 1 residual toxicity, whereas no patient suffered from grade 3 severity.
The high paclitaxel exposure in our study may have, in part, caused the unfavourable haematological toxicity profile of the PC-W regimen. However, we deliberately proceeded with the optimal dose of 100 mg/m2 derived from the preceding dose finding study. Although toxicity was not associated with serious complications like sepsis or neutropenic fever, a considerable number of additional treatments were needed to counterbalance the impaired bone marrow function. This will also produce extra costs. Maybe, a lower dose of paclitaxel of 80 mg/m2 will produce a better toxicity profile.
Progression free survival and overall survival are accepted endpoints for first-line trials and are more relevant than response rates. Although not deduced from a head-to-head-comparison, the similarity between survival curves with the present PC-W approach and conventional 3-weekly treatment is compelling.
Improving the therapeutic index is a major goal of ovarian cancer research, either by reducing toxicity (while maintaining current survival rates), or accepting higher toxicity for a considerably longer survival.
The dose of paclitaxel utilized in our regimen was 100 mg/m2 per week. In comparison to the conventional therapy, this is slightly (29%) higher than one would have received if they received a 3-week schedule of 175 mg/m2 per week. The total dose of paclitaxel administered in this first-line regimen was 1,800 mg/m2 compared to the 1,050 mg/m2 for the 3-week schedule (71% more). In comparison to the standard every 3-week schedule the platinum dose was equivalent but the dose intensity was lower in this study by 33%. This may have adversely affected the efficacy.
In a randomized trial of the Danish Ovarian Cancer Group, a doubling of the carboplatin dose-intensity did not result in any significant improvement of survival when combined with cyclophosphamide [34]. Future research must prove if dose saturation by additional treatment cycles is necessary to improve survival rates when using a combination of carboplatin and paclitaxel.
Based on our large phase-II trial a valid comparison of the weekly regimen with the 3-week regimen of paclitaxel and carboplatin is not possible. But we think that it is unlikely that PC-W contributes substantially improvement as first-line therapy. For patients with platinum-sensitive patients the weekly regimen seems to be maybe more attractive. Nevertheless, only a large randomized phase-III study is able to answer this question.
In conclusion, PC-W is associated with high rates of severe anaemia and leukopenia. Although not producing a high risk for sepsis or neutropenic fever, many patients may require rescue treatment with erythropoietin, erythrocytes, and G-CSF. Potentially lower neurotoxicity is a argument in favour of PC-W, given the reasonable chance for a self-limiting course of the condition. Median progression-free and overall survival did not exceed rates expected with standard treatment.
Only a prospective randomized study comparing the weekly schedule with the established 3-week schedule of the combination of carboplatin and paclitaxel is able to identify the best regimen with the best therapeutic index. Beside efficacy parameter (e.g. progression free survival) quality of life must be defined as primary objectives.
References
Bookman MA for the Gynecologic Cancer InterGroup (GCIG) through the Gynecologic Oncology Group (GOG) (2006) GOG0182-ICON5: 5-arm phase III randomized trial of paclitaxel and carboplatin vs combinations with gemcitabine, PEG-lipososomal doxorubicin, or topotecan in patients with advanced-stage epithelial ovarian or primary peritoneal carcinoma (Abstract 5002). J Clin Oncol 24 (Suppl 18):256s
Advanced Ovarian Cancer Trialists Group. Chemotherapy for advanced ovarian cancer (1999) Cochrane Database of Systematic Reviews 1999, Issue 1. Art. No.: CD001418. doi:10.1002/14651858.CD001418
Rosenberg P, Andersson H, Boman K, Ridderheim M, Sorbe B, Puistola U, Paro G (2002) Randomized trial of single agent paclitaxel given weekly versus every three weeks and with peroral versus intravenous steroid premedication to patients with ovarian cancer previously treated with platinum. Acta Oncol 41:418–424
Berek JS, Bertelsen K, du Bois A et al (1999) Advanced epithelial ovarian cancer: 1998 consensus statement. Ann Oncol 10(Suppl 1):87–92
National Comprehensive Cancer Network (2006) Clinical Practice Guidelines in Oncology-v.1.2006. Ovarian Cancer. Available at http://www.nccn.org/professionals/physician_gls/PDF/ovarian.pdf
NHS National Institute for Health and Clinical Excellence (2005) TA91 Ovarian cancer (advanced)-paclitaxel, pegylated liposomal doxorubicin hydrochloride and topotecan (review): guidance 2005. Available at http://www.nice.org.uk/download.aspx?o = TA091guidance
McGuire WP, Hoskins WJ, Brady MF et al (1996) Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med 334:1–6
Piccart MJ, Bertelsen K, James K et al (2000) Randomized intergroup trial of cisplatin-paclitaxel versus cisplatin-cyclophosphamide in women with advanced epithelial ovarian cancer: three-year results. J Natl Cancer Inst 92:699–708
Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, Mannel RS, DeGeest K, Hartenbach EM, Baergen R (2003) Phase III trial of carboplatin and paclitaxel compared with cisplatin and pacltitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol 21:3194–3200
Du Bois A, Lück HJ, Meier W, Adams HP, Mobus V, Costa S, Bauknecht T, Richter B, Warm M, Schröder W, Olbricht S, Nitz U, Jackisch C, Emons G, Wagner U, Kuhn W, Pfisterer J (2003) A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst 95:1320–1330
Sugimura M, Sagae S, Ishioka S, Nishioka Y, Tsukada K, Kudo R (2004) Mechanisms of paclitaxel-induced apoptosis in an ovarian cancer cell line and its paclitaxel-resistant clone. Oncology 66:53–61
Richardson A, Kaye SB (2005) Drug resistance in ovarian cancer: the emerging importance of gene transcription and spatio-temporal regulation of resistance. Drug Resist Updat 8:311–321
Lopes NM, Adams EG, Pitts TW, Bhuyan BK (1996) The microtubule-affecting drug paclitaxel has antiangiogenic activity. Clin Cancer Res 2:1843–1849
Smith JA, Ngo H, Martin MC, Wolf JK (2005) An evaluation of cytotoxicity of the taxane and platinum agents combination treatment in a panel of human ovarian carcinoma cell lines. Gynecol Oncol 98:141–145
Lopes NM, Adams EG, Pitts TW, Bhuyan BK (1993) Cell kinetics and cell cycle effects of taxol on human and hamster ovarian cell lines. Cancer Chemother Pharmacol 32:235–242
Browder T, Butterfield CE, Kraling BM et al (2000) Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 60:1878–1886
Pasquier E, Carre M, Pourroy B, Camoin L, Rebai O, Briand C, Braguer D (2004) Antiangiogenic activity of paclitaxel is associated with its cytostatic effect, mediated by the initiation but not completion of a mitochondrial apoptotic signaling pathway. Mol Cancer Ther 3:1301–1310
Liebmann JE, Cook JA, Lipschultz C, Teague D, Fisher J, Mitchell JB (1993) Cytotoxic studies of paclitaxel (taxol) in human tumour cell lines. Br J Cancer 68:1104–1109
Schiff PB, Horwitz SB (1980) Taxol stabilizes microtubules in mouse fibroblasts. Proc Natl Acad Sci USA 77:1561–1565
Sehouli J, Stengel D, Elling D et al (2002) First-line chemotherapy with weekly paclitaxel and carboplatin for advanced ovarian cancer: a phase I study. Gynecol Oncol 85:321–326
Calvert AH, Newell DR, Gumbrell LA et al (1989) Carboplatin dosage: prospective evaluation of a simple formula based on renal function. J Clin Oncol 7:1748–1756
Jelliffe RW (1973) Creatinine clearance: bedside estimate. Ann Intern Med 79:604–605
National Cancer Institute common toxicity criteria (1990) In: Perry MC (eds) The chemotherapy source book. Williams & Wilkins, Baltimore, pp 1133–1140
Gronlund B, Hogdall C, Hilden J, Engelholm SA, Hogdall EV, Hansen HH (2004) Should CA-125 response criteria be preferred to response evaluation criteria in solid tumours (RECIST) for prognostication during second-line chemotherapy of ovarian carcinoma? J Clin Oncol 22:4051–4058
Guppy AE, Rustin GJ (2002) CA125 response: can it replace the traditional response criteria in ovarian cancer? Oncologist 7:437–443
Havrilesky LJ, Alvarez AA, Sayer RA, Lancaster JM, Soper JT, Berchuck A, Clarke-Pearson DL, Rodriguez GC, Carney ME (2003) Weekly low-dose carboplatin and paclitaxel in the treatment of recurrent ovarian and peritoneal cancer. Gynecol Oncol 88:51–57
Kaern J, Baekelandt M, Tropé CG (2002) A phase II study of weekly paclitaxel in platinum and paclitaxel-resistant ovarian cancer patients. Eur J Gynaecol Oncol 23:383–389
Watanabe Y, Nakai H, Ueda H, Nozaki K, Hoshiai H (2005) Evaluation of weekly low-dose paclitaxel and carboplatin treatment for patients with platinum-sensitive relapsed ovarian cancer. Gynecol Oncol 96:323–329
Katsumata N, Watanabe T, Mukai H et al (2001) A phase II trial of weekly paclitaxel/carboplatin as salvage chemotherapy in patients with relapsed ovarian cancer (Abstract). Proc Am Soc Clin Oncol 19:865
Omura GA, Brady MF, Look KY, Averette HE, Delmore JE, Long HJ, Wadler S, Spiegel G, Arbuck SG (2003) Phase III trial of paclitaxel at two dose levels, the higher dose accompanied by filgrastim at two dose levels in platinum-pretreated epithelial ovarian cancer: an intergroup study. J Clin Oncol 21(15):2843–2848
Safra T, Bernstein Molho R et al (2006) A. phase-II study evaluating safety and efficacy with weekly paclitaxel and carboplatin as a primary treatment for patients with advanced epithelial ovarian cancer (Abstract). J Clin Oncol 24(Suppl 18):274s
Markman M, Kennedy A, Webster K, Kulp B, Peterson G, Belinson J (2001) Neurotoxicity associated with a regimen of carboplatin (AUC 5–6) and paclitaxel (175 mg/m2 over 3 h) employed in the treatment of gynecologic malignancies. J Cancer Res Clin Oncol 127:55–58
Pignata S, De Placido S, Biamonte R et al (2006) Residual neurotoxicity in ovarian cancer patients in clinical remission after first-line chemotherapy with carboplatin and paclitaxel: the Multicenter Italian Trial in Ovarian cancer (MITO-4) retrospective study. BMC Cancer 6:5
Jakobsen A, Bertelsen K, Andersen JE, Havsteen H, Jakobsen P, Moeller KA, Nielsen K, Sandberg E, Stroeyer I (1997) Dose effect study of carboplatin in ovarian cancer: a Danish Overian Cancer Group study. J Clin Oncol 15:193–198
Acknowledgments
The authors acknowledge Guelten-Oskay Özcelik, Dominique Koensgen and Isil Gücuncu, for assistance in data collection. We thank all participating patients and study nurses. Without their enthusiastic collaboration, this work would not have been possible.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This study was presented in part as selected poster at the 38th Annual Meeting of American Society of Clinical Oncology 2002 (Abstract 811).
Rights and permissions
About this article
Cite this article
Sehouli, J., Stengel, D., Mustea, A. et al. Weekly paclitaxel and carboplatin (PC-W) for patients with primary advanced ovarian cancer: results of a multicenter phase-II study of the NOGGO. Cancer Chemother Pharmacol 61, 243–250 (2008). https://doi.org/10.1007/s00280-007-0466-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0466-z