Abstract
Purpose
The proteasome inhibitor bortezomib may be effective in combination with cytarabine and anthracyclines in the treatment of acute myeloid leukemia (AML) by virtue of targeting aberrantly activated NF-κB in AML stem cells. We tested whether bortezomib cytotoxicity is affected by multidrug resistance (MDR) proteins expressed in AML cells. We also tested whether bortezomib interactions with cytarabine and anthracyclines are affected by p53, because proteasome inhibition stabilizes p53 and may thus cause cell cycle arrest.
Experimental design
Bortezomib sensitivity of cell lines overexpressing P-glycoprotein, multidrug resistance protein-1, breast cancer resistance protein and lung resistance protein was studied in the presence and absence of established modulators of these transport proteins. Drug interactions during simultaneous and sequential exposure to bortezomib and anthracyclines or cytarabine in diverse ratios were evaluated by isobologram and combination index analyses in AML cell lines with wild type and inactive p53 and were correlated with cell cycle perturbations induced by bortezomib.
Results
Of the MDR mechanisms studied, only P-glycoprotein conferred resistance to bortezomib, and resistance was only twofold. Interactions between bortezomib and anthracylines and cytarabine changed from antagonistic to additive or synergistic with increasing drug activity levels and were not affected by p53 status.
Conclusions
MDR proteins and p53 do not affect bortezomib cytotoxicity or in vitro interactions with anthracyclines or cytarabine, but these interactions are concentration-dependent, and this concentration-dependency should be considered in the design of combination regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cure rates in acute myeloid leukemia (AML) remain low, and new treatments continue to be needed for this disease. Mechanisms known to contribute to treatment failure in AML include impaired cellular drug transport associated with expression of ATP-binding cassette (ABC) proteins, including P-glycoprotein (Pgp; ABCB1), multidrug resistance protein-1 (MRP-1; ABCC1) and breast cancer resistance protein (BCRP; ABCG2) [6, 20, 21, 32], and impaired cytoplasmic-nuclear drug transport associated with expression of the major vault protein lung resistance protein (LRP) [24]. In addition to impaired drug transport, aberrant activation of signal transduction proteins including the transcription factor nuclear factor-kappa B (NF-κB) has been implicated in treatment failure in AML [15].
Constitutive activation of NF-κB in AML stem cells [15] suggests that therapies inhibiting NF-κB have the potential to target AML stem cells, and lack of activation of NF-κB in normal hematopoietic stem cells [15] suggests that these therapies could be leukemia-specific. In in vitro studies, NF-κB inhibition specifically induces apoptosis in AML cells and potentiates the apoptotic response induced by doxorubicin, cytarabine and etoposide, while sparing normal CD34+ hematopoietic precursors [12]. Activation of NF-κB requires proteasome-dependent degradation of its inhibitor IκB [5, 19], and proteasome inhibitors thus have therapeutic potential in AML by virtue of targeting NF-κB.
Mechanisms of resistance to NF-κB inhibition have not been studied in AML cells. Bortezomib, the first proteasome inhibitor approved for use in humans [8], was designed to abrogate transport by Pgp, in contrast to the earlier generation of proteasome inhibitors, peptide aldehydes, whose efficacy was limited by Pgp-mediated transport [1, 18]. In contrast, transport by MRP-1, BCRP and LRP has not been studied. Moreover, in addition to its effects on NF-κB, bortezomib also stabilizes p53, resulting in cell cycle arrest (reviewed in Ref. [36]). Sensitivity to bortezomib and/or its interaction with cytotoxic chemotherapy drugs as a function of p53 status may be cell type-dependent (reviewed in Ref. [7]), with p53-dependence reported for breast [26] and lung [23] cancer and p53-independence reported for prostate [1] and colon [11] cancer and multiple myeloma [16]. We studied the effects of p53 status on the efficacy of bortezomib in combination with anthracyclines and cytarabine in AML cells, and correlated the effects of p53 status with bortezomib effects on cell cycle.
Materials and methods
Cell lines
Human AML cell lines included HL60, which is p53-null [20], ML1, which has wild-type p53 [22], and established drug-selected variants of HL60 cells with multidrug resistance mediated by Pgp (HL60/VCR) and MRP-1 (HL60/Adr). Because leukemia cell lines expressing BCRP and LRP are not available, we studied drug-selected 8226/MR20 multiple myeloma cells, which overexpress BCRP and LRP, and also studied parental 8226 cells, with low-level BCRP expression, and drug-selected 8226/Dox6 cells, with Pgp and low-level BCRP expression. Cell culture conditions and characterization of MDR protein expression and function in these cell lines were previously described [28, 31].
Drugs
Bortezomib (Velcade) was obtained from Millennium Pharmaceuticals Inc., Cambridge, MA, USA, and stored at −20 °C as a 50 μM stock solution in phosphate-buffered saline (PBS). Doxorubicin, daunorubicin and idarubicin were purchased from Sigma–Aldrich Corp., St. Louis, MO, USA and stock solutions of 1 mg/ml in PBS were stored at −20 °C. Mitoxantrone was also purchased from Sigma–Aldrich, and a stock solution of 19.3 mM in PBS was stored at −20 °C. Cytarabine was purchased from The Upjohn Company, Kalamazoo, MI, USA and stored as a 358 mM stock solution at −20 °C. MDR modulators used in comparison studies included PSC-833, which is Pgp-specific, obtained from Novartis, East Hanover, NJ, USA, MK-571, which is MRP-1-specific, purchased from Calbiochem, San Diego, CA, USA, and fumitremorgin C (FTC), which is BCRP-specific, obtained from Dr. Susan Bates, National Cancer Institute, Bethesda, MD, USA, at concentrations of 2.5, 15 and 10 μM, respectively [31].
Cytotoxicity assay
To study cytotoxicity of drugs alone or in combination with fixed non-cytotoxic concentrations of MDR modulators, cell lines were treated with drug at 11 logarithmically spaced concentrations (five-log range) in triplicate in 96-well plates. Cells were seeded at a starting density of 10,000/well and drugs were added to the cell cultures from frozen stocks to achieve the final desired concentrations in 100 μl final volumes. Cells were then cultured for 96 h, and viability was quantified by the WST-1 colorimetric assay (Roche Diagnostics, Mannheim, Germany), as described previously [31]. Briefly, 10 μl WST-1 were added to each well and culture plates were allowed to develop for 2–4 h in the incubator to achieve the desired absorbance in the control wells. Absorbance at 450 nm (A450) and 600 nm (A600, background) was read for each well using a plate reader (Beckman Coulter, Fullerton, CA, USA). The drug concentrations resulting in 50% decrease of viable cell numbers compared to the non-drug-treated controls (IC50) were determined through weighted curve-fitting, as described previously [14]. IC50 concentrations in different treatment groups were compared by non-paired t-test statistics.
To study combinations of bortezomib with anthracyclines or cytarabine, experiments were conducted with the same procedures as for single agent studies, but in quintuplicate 96-well plates. Each plate contained each single agent alone at 11 concentrations and drug combinations at five constant ratios (1:1 at the IC50, 2:1, 1:2, 4:1, 1:4) at 11 different concentrations. Drug interactions were then evaluated by isobologram analysis, as previously described [14], and by combination index analysis according to the method of Chou and Talalay [9], using CalcuSyn Software (Biosoft, Cambridge, UK).
Cell cycle distribution
To study cell cycle distribution before and during bortezomib exposure, 0.5 × 106 cells at each time point were fixed in 70% ice-cold ethanol for at least 1 h, then washed with PBS, stained with propidium iodide (PI) and analyzed on a FacScan flow cytometer as previously described [38].
Results
Activity of bortezomib in cell lines overexpressing MDR proteins
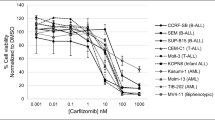
Sensitivity of multidrug resistant HL60/VCR, HL60/ADR, 8226/Dox6 and 8226/MR20 cells and of parental HL60 and 8226 cells to bortezomib was tested in the absence and presence of the MDR protein-specific modulators PSC-833 (Pgp), MK571 (MRP-1) and FTC (BCRP) (Fig. 1a). HL60/VCR and 8226/Dox6, the two cell lines expressing Pgp, displayed a low but significant level of resistance to bortezomib (1.8- and 2.0-fold resistance, respectively) and resistance was significantly modulated by the Pgp-specific modulator PSC-833. The HL60/ADR and 8226/MR20 cell lines, expressing MRP-1 and BCRP, respectively, were not resistant to bortezomib, in relation to parental cells, and the MRP-1- and BCRP-specific modulators MK571 and FTC had no effect on bortezomib sensitivity. Of note, since 8226/MR20 cells also overexpress LRP [31], the data indicate that bortezomib is also not subject to LRP-mediated resistance.
In vitro sensitivity of cell lines overexpressing Pgp (HL60/VCR, 8226/Dox6), MRP-1 (HL60/Adr), BCRP (8226/MR20, 8226/Dox6) and LRP (8226/MR20) to a bortezomib and b mitoxantrone in the absence and presence of the MDR protein-specific modulators PSC833 (Pgp), MK571 (MRP-1) or FTC (BCRP). Parental HL60 cells do not express any of these MDR transport proteins, whereas parental 8226 cells express a low level of BCRP. Each bar represents the mean IC50 concentration of triplicate experiments and error bars represent the standard errors of the mean. The black * and ** above the bars denote p < 0.01 and 0.001, respectively, for differences between IC50’s of drug-resistant and parental cell lines treated with drug (bortezomib or mitoxantrone) alone. The white * and ** inside the bars denote p < 0.01 and 0.001, respectively, for differences between IC50’s of cells treated with drug (bortezomib or mitoxantrone) in the absence and presence of modulator
As a control, sensitivity of the same cell lines to the MDR protein substrate drug mitoxantrone was determined in the absence and presence of modulators (Fig. 1b). Multidrug resistant HL60/VCR, HL60/ADR, 8226/Dox6 and 8226/MR20 cells were 15.8-, 390-, 39- and 4.7-fold resistant to mitoxantrone, respectively, and were sensitized by the relevant MDR modulators. FTC sensitization of parental 8226 cells was consistent with their known low-level BCRP expression [28]. MK571 unexpectedly modulated sensitivity of the HL60 parental cell line to mitoxantrone 2.8-fold, but this modulator had a much greater (ninefold) effect on mitoxantrone sensitivity of HL60/Adr cells.
Thus all of the MDR mechanisms studied, including Pgp, MRP-1, BCRP and LRP, confer resistance to mitoxantrone, but only Pgp conferred resistance to bortezomib, and resistance was low-level (twofold).
Effect of p53 status on interaction between bortezomib and anthracyclines in AML cells
To determine the effect of p53 status on the interaction between bortezomib and anthracyclines in AML cells, the effect of simultaneous exposure to bortezomib and doxorubicin, daunorubicin or idarubicin at fixed constant drug concentration ratios was studied and compared to the activity of each drug as a single agent in HL60 (p53 null) and ML1 (wild-type p53) cells. Figure 2 shows the isobologram analysis of the interactions between bortezomib and doxorubicin, daunorubicin and idarubicin at five different drug activity levels (IC10, IC25, IC50, IC75 and IC90). In each plot, the diagonal represents the additivity line, and data below and above the additivity line signify synergistic and antagonistic interactions, respectively. In HL60 cells the interaction between bortezomib and the anthracyclines was generally antagonistic, in particular at lower drug activity levels, but for doxorubicin and idarubicin the degree of antagonism decreased with increasing drug activity levels (Fig. 2a). The interaction between bortezomib and anthracyclines was also generally antagonistic in ML1 cells, and the degree of antagonism decreased with increasing drug activity levels for doxorubicin, but antagonism increased with increasing drug activity levels for daunorubicin and idarubicin (Fig. 2b).
Isobologram analysis of interactions between bortezomib and doxorubicin (top row), daunorubicin (middle row) or idarubicin (bottom row) under simultaneous drug exposure conditions in 96-h cultures. For each drug combination, the isobols at the IC10, IC25, IC50, IC75 and IC90 drug activity levels are shown. a Results for the p53-null cell line HL60 and b results for the wild-type p53 cell line ML1
Effect of drug sequence on interaction between bortezomib and anthracyclines
Since other reports have indicated that interactions between bortezomib with anthracyclines may be schedule-dependent [4, 29], the effect of a 24-h delay between the start of drug exposures was studied, with doxorubicin as a representative anthracycline. The isobols in Fig. 3 demonstrate that in HL60 cells, the interaction between doxorubicin and bortezomib was independent of the sequence of drug exposure.
Isobologram analysis of interactions between bortezomib and doxorubicin with bortezomib exposure started 24 h before doxorubicin exposure (top panels) and doxorubicin 24 h before bortezomib (bottom panels). For each drug combination, the isobols at the IC10, IC25, IC50, IC75 and IC90 drug activity levels are shown
Effect of method of analysis
In order to determine whether the observed drug interactions were affected by the method of analysis, all of the data were additionally analyzed using the combination index method of Chou and Talalay [9]. In the plots shown in Fig. 4, a combination index (CI) value of 1 equates with drug additivity, while CI values below or above 1 indicate synergistic or antagonistic drug interactions, respectively. Whereas with the isobologram analysis the drug interactions at different drug activity levels are plotted individually, in the CI plots interactions at different drug activity levels (Fa) are combined in one plot. The data in Fig. 4 demonstrate that, in agreement with the isobologram analyses, interactions between bortezomib and the anthracyclines were generally antagonistic in both HL60 (p53-null) and ML1 (wild-type p53) cells, regardless of the constant ratio between the partner drugs. The combination of bortezomib with idarubicin in ML1 cells was the only exception, showing a generally additive effect. The CI data demonstrated a general trend of gradual change of drug interactions from antagonism to additivity and synergy with increasing drug activity levels.
a Combination index (CI) analysis (Chou and Talalay method) of interactions between bortezomib and doxorubicin (top), daunorubicin (middle) or idarubicin (bottom) under simultaneous drug exposure conditions (96-h cultures). For each drug combination, CI’s at various drug activity levels (Fa) and various constant drug concentration ratios (as indicated in each plot) are shown. Results for the p53-null cell line HL60 are shown on the left and results for the wild-type p53 cell line ML1 are shown on the right. b Combination index (CI) analysis (Chou and Talalay method) of the interactions between bortezomib and cytarabine (Ara-C) in HL60 cells under simultaneous drug exposure conditions in 96-h cultures
Drug interaction between bortezomib and cytarabine
The interaction between bortezomib and cytarabine was studied in the HL60 cell line. Like the anthracyclines, cytarabine also had an antagonistic interaction with bortezomib, particularly at lower drug activity levels (Fig. 4b).
Effect of bortezomib pre-treatment on cytarabine and daunorubicin sensitivity
In a previous study of interactions between bortezomib and anthracyclines, the effect of 24-h pre-incubation with a fixed concentration of bortezomib on the IC50 of the second drug was studied [29]. To mimic these conditions, HL60 cells were exposed to bortezomib at a non-cytotoxic concentration (3 nM) or at its approximate IC50 concentration (10 nM). Cytarabine or daunorubicin was then added to the cultures after 24 h at a range of concentrations and the cell cultures were continued for 4 days in the presence of the drug combinations, after which cell viability was analyzed with the WST-1 assay and IC50 concentrations were determined using cells exposed to bortezomib alone as controls. As shown in Fig. 5 a, bortezomib did not enhance cytarabine or daunorubicin sensitivity under these conditions. In order to determine whether this lack of sensitization was particular to HL60 cells, we also treated ML1 cells and 8226 cells with bortezomib for 24 h, then added daunorubicin for 24 h, but, as in HL60 cells, bortezomib did not enhance daunorubicin cytotoxicity in either of these two additional cell lines (Fig. 5b).
Effect of pre-incubation with fixed concentrations of bortezomib on sensitivity of HL60 cells to daunorubicin or cytarabine. a Cells were exposed to bortezomib 24 h before and during exposure to daunorubicin or cytarabine. The IC50 concentrations were determined as the survival of the cells exposed to the drug combinations relative to cells exposed to bortezomib alone at the corresponding concentrations. Each bar represents the mean IC50 concentration of triplicate experiments and error bars represent the standard errors of the mean. IC50 concentrations did not change significantly as a function of bortezomib pre-incubation. b The same approach was applied to daunorubicin sensitivity in ML1 and 8226 cells
Bortezomib-induced cell cycle perturbations in p53-null and wt p53 cells
Cell cycle distributions of HL60 cells (p53-null) and ML1 cells (wt p53) before and during exposure to bortezomib are shown in Fig. 6. Cell cycle effects of bortezomib were both concentration- and p53-dependent. Bortezomib in concentrations up to 1 nM did not affect the cell cycle distributions in HL60 or ML1 cells, but at its approximate IC50 concentration of 10 nM, bortezomib induced an accumulation of cells in S-phase in the HL60 cells, which are p53-null [33], whereas no difference in cell cycle distribution was observed in ML1 cells, which have wild-type p53 [22]. Thus the antagonistic interactions observed at bortezomib activity levels below its IC50 concentration of 10 nM are not explained by cell cycle perturbations. On the other hand, the fact that bortezomib induces cell cycle arrest in HL60 cells at higher drug activity levels indicates that the additive or synergistic interactions observed at these drug concentration levels in these cells are independent of active cell cycle traverse.
Discussion
Bortezomib is an active drug in the treatment of multiple myeloma, and its activity in AML is currently being investigated [4, 10]. We sought to determine the effects of drug resistance mechanisms prevalent in AML on the cytotoxic activity of bortezomib and to study interactions between bortezomib and chemotherapy drugs used in the treatment of AML, including anthracyclines and cytarabine, in AML cells with active and inactive p53.
We demonstrated that the presence of Pgp, which conferred more than tenfold resistance to mitoxantrone in the cell line models studied, resulted in approximately twofold resistance to bortezomib. A recent study of the in vivo sensitivity of Pgp-expressing multidrug resistant neuroblastoma cells to bortezomib similarly showed a lack of resistance in relation to drug-sensitive parental cells [27], consistent with our finding that the effect of Pgp on bortezomib activity is small and is thus likely to be negligible in vivo. We also demonstrated here for the first time that the MDR proteins MRP-1, BCRP and LRP do not confer resistance to bortezomib.
We found that simultaneous combination of bortezomib with anthracyclines or cytarabine generally results in antagonistic or, at best, additive drug interactions at low to intermediate drug activity levels. These results are in agreement with some previous studies of the same drug combinations [2, 4, 17], but contradict others [25, 29]. Simultaneous combinations with drugs other than anthracyclines or cytarabine have also resulted in antagonistic interactions with some drugs [13, 17], but synergistic interactions with others [17, 25]. The apparent inconsistency in the literature also applies to the importance of sequence of administration in drug interactions. For example, in studies combining bortezomib with doxorubicin or paclitaxel, synergistic drug interactions were only seen when doxorubicin or paclitaxel was added to cultured cells 24 h after bortezomib, whereas the reverse combination or simultaneous exposure resulted in additive or antagonistic interactions [2]. In contrast, in a study combining bortezomib with SN-38, the active metabolite of irinotecan, synergy was only seen when bortezomib followed SN-38, while the reverse sequence resulted in antagonism [35]. Collectively, these inconsistent reports suggest that findings with regard to interactions between bortezomib and cytotoxic chemotherapy drugs might depend on the choice of drug used in combination, the cell line studied and the method used to assess the drug interactions.
The role of p53 in sensitivity to bortezomib and/or chemosensitization by bortezomib may also be cell type-dependent [7]. In the AML cell lines studied and in the bortezomib concentration range studied, p53 status did not affect drug interactions, although bortezomib effects on cell cycle differed in the p53 wild type and p53-null cell lines.
In the cell lines studied, bortezomib’s interactions with anthracyclines and cytarabine appeared to be independent of cell cycle perturbations, as no cell cycle perturbations were observed following exposure to bortezomib in the ML-1 cells with wild-type p53, and complete inhibition of cell cycle traverse was observed in the HL60 cells, which were p53-null, but only following exposure to the highest bortezomib concentration tested (10 nM), which was associated with additive or synergistic drug interactions in the drug combination assays. The antagonistic interactions observed at lower bortezomib activity levels may be associated with bortezomib’s inhibitory effect on NF-κB, as activity of both anthracycline [3] and cytarabine [34] is known to be NF-κB-dependent.
With regard to clinical applicability, an important consideration is that the highest concentrations of bortezomib, which resulted in greater than 90% cell kill in our in vitro studies (0.1–0.2 μM), are readily attainable in patients. Although the pharmacokinetics of bortezomib as a single agent have not been fully characterized at the recommended dose of 1.3 mg/m2 in multiple myeloma patients, the median estimated maximum plasma concentration following intravenous administration at this dose is 509 ng/ml (1.32 μM), with a range of 109–1,300 ng/ml (0.28–3.38 μM) [18]. Even if the 83% binding to human plasma proteins [8] is considered, levels of bioavailable drug would still range from 0.047 to 0.574 μM. Thus the synergistic interactions at high drug activity levels that we and others [17] have found are clinically relevant. However, the peak plasma concentrations of bortezomib are short-lived. Initial distribution half-lives of bortezomib in doses of 1.45–2.0 mg/m2 ranged from 0.22 to 0.46 h and were dose-independent, followed by a more sustained terminal elimination half-life of more than 10 h [30]. The near steady-state plasma concentration in the latter studies was approximately 1 ng/ml (0.0026 μM), which corresponds to the low to intermediate drug activity levels that resulted in antagonistic drug interactions in our in vitro studies. Thus the pharmacokinetic profile of bortezomib needs to be considered in choosing schedules for combination studies with anthracyclines or cytarabine.
Lack of synergistic interactions in in vitro assays does not rule out therapeutic benefit of drug combinations in vivo, since beneficial effects on factors pertinent to tumor environment are not measured in the in vitro studies. A recent study reporting that the combination of tipifarnib and bortezomib overcomes cell adhesion-mediated drug resistance in multiple myeloma and AML attests to potential beneficial effects of bortezomib on the tumor environment in leukemia [37].
In conclusion, bortezomib has the potential to be an effective drug in the treatment of AML since effective drug concentrations are readily attainable in patients and drug resistance mechanisms known to be relevant in AML do not affect its activity. Dose-dependent drug interactions between bortezomib and drugs with known efficacy in AML should be taken into consideration, along with pharmacokinetic profiles, in the design of combination regimens.
References
Adams J, Palombella VJ, Sausville EA, Johnson J, Destree A, Lazarus DD, Maas J, Pien CS, Prakash S, Elliott PJ (1999) Proteasome inhibitors: a novel class of potent and effective antitumor agents. Cancer Res 59:2615–2622
An J, Sun Y, Fisher M, Rettig MB (2004) Antitumor effects of bortezomib (PS-341) on primary effusion lymphomas. Leukemia 18:1699–1704
Ashikawa K, Shishodia S, Fokt I, Priebe W, Aggarwal BB (2004) Evidence that activation of nuclear factor-kappaB is essential for the cytotoxic effects of doxorubicin and its analogues. Biochem Pharmacol 67:353–364
Attar EC, Learner E, Amrein PC (2004) In vitro studies of bortezomib with daunorubicin and cytarabine: sequence of administration affects leukemia cell chemosensitivity. Blood 104 [Abstract 4464]
Baldwin AS (1996) The NF-κB and IκB proteins: new discoveries and insights. Annu Rev Immunol 14:649–681
Benderra Z, Faussat AM, Sayada L, Perrot JY, Chaoui D, Marie JP, Legrand O (2004) Breast cancer resistance protein and P-glycoprotein in 149 adult acute myeloid leukemias. Clin Cancer Res 10:7896–7902
Boccadoro M, Morgan G, Cavenagh J (2005) Preclinical evaluation of the proteasome inhibitor bortezomib in cancer therapy. Cancer Cell Int 5:18
Bross PF, Kane R, Farrell AT, Abraham S, Benson K, Brower ME, Bradley S, Gobburu JV, Goheer A, Lee SL, Leighton J, Liang CY, Lostritto RT, McGuinn WD, Morse DE, Rahman A, Rosario LA, Verbois SL, Williams G, Wang YC, Pazdur R (2004) Approval summary for bortezomib for injection in the treatment of multiple myeloma. Clin Cancer Res 10:3954–3964
Chou TC, Talalay P (1984) Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul 22:27–55
Cortes J, Thomas D, Koller C, Giles F, Estey E, Faderl S, Garcia-Manero G, McConkey D, Ruiz SL, Guerciolini R, Wright J, Kantarjian H (2004) Phase I study of bortezomib in refractory or relapsed acute leukemias. Clin Cancer Res 10:3371–3376
Cusack JC Jr, Liu R, Houston M, Abendroth K, Elliott PJ, Adams J, Baldwin AS Jr (2001) Enhanced chemosensitivity to CPT-11 with proteasome inhibitor PS-341: implications for systemic nuclear factor-kappaB inhibition. Cancer Res 61:3535–3540
Frelin C, Imbert V, Griessinger E, Peyron AC, Rochet N, Philip P, Dageville C, Sirvent A, Hummelsberger M, Berard E, Dreano M, Sirvent N, Peyron JF (2005) Targeting NF-κB activation via pharmacological inhibition of IKK2 induced apoptosis of human acute myeloid leukemia cells. Blood 105:804–811
Gatto S, Scappini B, Pham L, Onida F, Milella M, Ball G, Ricci C, Divoky V, Verstovsek S, Kantarjian HM, Keating MJ, Cortes-Franco JE, Beran M (2003) The proteasome inhibitor PS-341 inhibits growth and induces apoptosis in Bcr/Abl-positive cell lines sensitive and resistant to imatinib mesylate. Haematologica 88:853–863
Greco WR, Park HS, Rustum YM (1990) Application of a new approach for the quantitation of drug synergism to the combination of cis-diamminedichloroplatinum and 1-beta-d-arabinofuranosylcytosine. Cancer Res 50:18–27
Guzman ML, Neering SJ, Upchurch D, Grimes B, Howard DS, Rizzieri DA, Luger SM, Jordan CT (2001) Nuclear factor-κB is constitutively activated in primitive human acute myelogenous leukemia cells. Blood 98:2301–2307
Hideshima T, Richardson P, Chauhan D, Palombella VJ, Elliott PJ, Adams J, Anderson KC (2001) The proteasome inhibitor PS-341 inhibits growth, induces apoptosis, and overcomes drug resistance in human multiple myeloma cells. Cancer Res 61:3071–3076
Horton TM, Gannavarapu A, Blaney SM, D’Argenio DZ, Plon SE, Berg S. (2006) Bortezomib interactions with chemotherapy agents in acute leukemia in vitro. Cancer Chemother Pharmacol 58:13–23
Jung L, Holle L, Dalton WS (2004) Discovery, development, and clinical applications of bortezomib. Oncology 18(suppl 11):4–13
Karin M, Ben-Neriah Y (2000) Phosphorylation meets ubiquitination: the control of NF-κB activity. Annu Rev Immunol 18:621–663
Leith CP, Kopecky KJ, Godwin J, McConnell T, Slovak ML, Chen IM, Head DR, Appelbaum FR, Willman CL (1997) Acute myeloid leukemia in the elderly: assessment of multidrug resistance (MDR1) and cytogenetics distinguishes biologic subgroups with remarkably distinct responses to standard chemotherapy. A Southwest Oncology Group Study. Blood 89:3323–3329
Leith CP, Kopecky KJ, Chen IM, Eijdems L, Slovak ML, McConnell TS, Head DR, Weick J, Grever MR, Appelbaum FR, Willman CL (1999) Frequency and clinical significance of the expression of the multidrug resistance proteins MDR1/P-glycoprotein, MRP1, and LRP in acute myeloid leukemia: a Southwest Oncology Group Study. Blood 94:1086–1099
Li ZR, Hromchak R, Mudipalli A, Bloch A (1998) Tumor suppressor proteins as regulators of cell differentiation. Cancer Res 58:4282–4287
Ling YH, Liebes L, Jiang JD, Holland JF, Elliott PJ, Adams J, Muggia FM, Perez-Soler R (2003) Mechanisms of proteasome inhibitor PS-341-induced G(2)-M-phase arrest and apoptosis in human non-small cell lung cancer cell lines. Clin Cancer Res 9:1145–1154
List AF, Spier CS, Grogan TM, Johnson C, Roe DJ, Greer JP, Wolff SN, Broxterman HJ, Scheffer GL, Scheper RJ, Dalton WS (1996) Overexpression of the major vault transporter protein lung-resistance protein predicts treatment outcome in acute myeloid leukemia. Blood 87:2464–2469
Ma MH, Yang HH, Parker K, Manyak S, Friedman JM, Altamirano C, Wu ZQ, Borad MJ, Frantzen M, Rousos E, Neeser J, Mikail A, Adams J, Sjak-Shie N, Vescio RA, Berenson JR (2003) The proteasome inhibitor PS-341 markedly enhances sensitivity of multiple myeloma tumor cells to chemotherapeutic agents. Clin Cancer Res 9:1136–1144
MacLaren AP, Chapman RS, Wyllie AH, Watson CJ (2001) p53-dependent apoptosis induced by proteasome inhibition in mammary epithelial cells. Cell Death Differ 8:210–218
Michaelis M, Fichtner I, Behrens D, Haider W, Rothweiler F, Mack A, Cinatl J, Doerr HW, Cinatl J Jr (2006) Anti-cancer effects of bortezomib against chemoresistant neuroblastoma cell lines in vitro and in vivo. Int J Oncol 28:439–446
Minderman H, Suvannasankha A, O’Loughlin KL, Scheffer GL, Scheper RJ, Robey RW, Baer MR (2002) Flow cytometric analysis of breast cancer resistance protein expression and function. Cytometry 48:59–65
Mitsiades N, Mitsiades CS, Richardson PG, Poulaki V, Tai YT, Chauhan D, Fanourakis G, Gu X, Bailey C, Joseph M, Libermann TA, Schlossman R, Munshi NC, Hideshima T, Anderson KC (2003) The proteasome inhibitor PS-341 potentiates sensitivity of multiple myeloma cells to conventional chemotherapeutic agents: therapeutic applications. Blood 101:2377–2380
Papandreou CN, Daliani DD, Nix D, Yang H, Madden T, Wang X, Pien CS, Millikan RE, Tu SM, Pagliaro L, Kim J, Adams J, Elliott P, Esseltine D, Petrusich A, Dieringer P, Perez C, Logothetis CJ (2004) Phase I trial of the proteasome inhibitor bortezomib in patients with advanced solid tumors with observations in androgen-independent prostate cancer. J Clin Oncol 22:2108–2121
Qadir M, O’Loughlin K, Williamson NA, Fricke SM, Minderman H, Baer MR (2005) Cyclosporine A is a broad-spectrum multidrug resistance modulator. Clin Cancer Res 11:2320–2326
Schaich M, Soucek S, Thiede C, Ehninger G, Illmer T (2005) MDR1 and MRP1 gene expression are independent predictors for treatment outcome in adult acute myeloid leukaemia. Br J Haematol 128:324–332
Shimizu T, Pommier Y (1997) Camptothecin-induced apoptosis in p53-null human leukemia HL60 cells and their isolated nuclei: effects of the protease inhibitors Z-VAD-fmk and dichloroisocoumarin suggest an involvement of both caspases and serine proteases. Leukemia 11:1238–1244
Sreenivasan Y, Sarkar A, Manna SK (2003) Mechanism of cytosine arabinoside-mediated apoptosis: role of Rel A (p65) dephosphorylation. Oncogene 22:4356–4369
Vaziri SA, Hill J, Chikamori K, Grabowski DR, Takigawa N, Chawla-Sarkar M, Rybicki LR, Gudkov AV, Mekhail T, Bukowski RM, Ganapathi MK, Ganapathi R (2005) Sensitization of DNA damage-induced apoptosis by the proteasome inhibitor PS-341 is p53 dependent and involves target proteins 14-3-3 sigma and survivin. Mol Cancer Ther 4:1880–1890
Voorhees PM, Dees EC, O’Neil B, Orlowski RZ (2003) The proteasome as a target for cancer therapy. Clin Cancer Res 9:6316–6325
Yanamandra N, Colaco NM, Parquet NA, Buzzeo RW, Boulware D, Wright G, Perez LE, Dalton WS, Beaupre DM (2006) Tipifarnib and bortezomib are synergistic and overcome cell adhesion-mediated drug resistance in multiple myeloma and acute myeloid leukemia. Clin Cancer Res 12:591–599
Yin MB, Guo B, Vanhoefer U, Azrak RG, Minderman H, Frank C, Wrzosek C, Slocum HK, Rustum YM (2000) Characterization of protein kinase chk1 essential for the cell cycle checkpoint after exposure of human head and neck carcinoma A253 cells to a novel topoisomerase I inhibitor BNP1350. Mol Pharmacol 57:453–459
Acknowledgments
This work was supported by a Leukemia and Lymphoma Society Translational Research Program Grant (to MRB), by shared resources of the Roswell Park Cancer Center Support Grant (P30 CA16056), the Leonard S. LoVullo Memorial Fund for Leukemia Research and the Dennis J. Szefel Jr. Endowed Fund for Leukemia Research at Roswell Park Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Minderman, H., Zhou, Y., O’Loughlin, K.L. et al. Bortezomib activity and in vitro interactions with anthracyclines and cytarabine in acute myeloid leukemia cells are independent of multidrug resistance mechanisms and p53 status. Cancer Chemother Pharmacol 60, 245–255 (2007). https://doi.org/10.1007/s00280-006-0367-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-006-0367-6