Abstract
Purpose
The goal of this study was to identify molecular determinants of sensitivity and resistance to JM118, the active metabolite of satraplatin, an orally bioavailable cisplatin analog that has activity in prostate cancer.
Experimental design
Human ovarian carcinoma 2008/JM118 cells were derived from parental 2008 cells by repeated exposure to JM118; the revertant 2008/JM118/REV subline was isolated from the 2008/JM118 cells by growth in the absence of drug. Drug sensitivity was determined by clonogenic assay and Pt levels were measured by ICP-MS.
Results
Eight sequential rounds of selection yielded the 2008/JM118 subline that was 4.9-fold resistant to JM118 and cross-resistant at varying levels to satraplatin, cisplatin, carboplatin, and oxaliplatin. Cross-resistance to the other Pt drugs was lost as resistance to JM118 waned. The same parental 2008 cells selected for resistance to cisplatin were partially cross-resistant to JM118. The 2008/JM118 cells accumulated significantly more Pt than the 2008 cells when exposed to low concentrations of either JM118 or cisplatin indicating a detoxification process that involves intracellular sequestration. In contrast, 2008 cells selected for cisplatin resistance accumulated less cisplatin and less JM118 reflecting a mechanism involving reduced accumulation. The 2008 and 2008/JM118 cells did not differ in their uptake or efflux of 64Cu, expression of Cu efflux transporters ATP7A or ATP7B or their glutathione content. The 2008/JM118 cells exhibited 3.0–7.7-fold hypersensitivity to docetaxel, paclitaxel and doxorubicin. Expression profiling identified 4 genes that were significantly up-regulated and 19 that were down-regulated in the 2008/JM118 cells at a false discovery rate of 1 gene.
Conclusions
While the cellular defense mechanisms that protect cells against JM118 also mediate resistance to the other Pt drugs, these mechanisms are quite different from those commonly found in cells selected for resistance to cisplatin. JM118-resistant cells accumulate more rather than less Pt and rely on an intracellular detoxification mechanism different from that involved in cisplatin resistance. This is consistent with clinical evidence suggesting that satraplatin has activity in diseases in which cisplatin does not. In this model, JM118 resistance is associated with substantial collateral hypersensitivity to docetaxel, paclitaxel, and doxorubicin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Satraplatin, bis(acetato)amminedichloro(cyclohexylamine) platinum (Fig. 1), is a novel platinum (IV) complex that has substantial oral bioavailability (reviewed in [18]). It has potent in vitro growth inhibitory properties and is cytotoxic to tumors and cell lines that are generally unresponsive to cisplatin (DDP). Clinically, satraplatin has demonstrated activity in patients with advanced hormone-refractory prostate cancer [39], a disease in which DDP has no clinically useful activity. The key differences in their mechanism of action that account for their different spectrum of clinical activity are not known. Both drugs are thought to exert their cytotoxic activity by forming adducts in DNA in a similar manner. DNA damage caused by satraplatin is repaired in vitro by the nucleotide excision repair pathway with kinetics similar to those for the repair of DDP adducts [31].
Most cell lines selected for acquired DDP resistance have defects in drug accumulation [1, 19, 24, 28, 41, 43–45]. In contrast, no alteration of satraplatin accumulation was found in two ovarian carcinoma cell lines selected for resistance to satraplatin [18]. However, satraplatin is rapidly metabolized during absorption and is found in the blood primarily as JM118 (Fig. 1), a metabolite that is up to 16-fold more potent than native satraplatin [46]. JM118 is an active metabolite of satraplatin and has been shown to have greater cytotoxicity than DDP while forming intra- and inter-strand crosslinks in DNA in a manner similar to DDP (reviewed in [5]).
In the current study, a subline of the well-characterized 2008 ovarian carcinoma cell line was developed by repeated exposure to JM118 and the cellular pharmacology of JM118 was extensively examined in this subline. We report here that 2008/JM118 cells are resistant to both JM118 and satraplatin, and cross-resistant to DDP and its analogs carboplatin and oxaliplatin. Interestingly, 2008/JM118 cells were found to be hypersensitive to several non-Pt compounds, including docetaxel, paclitaxel, doxorubicin, and mitoxantrone. The changes in the cellular pharmacology of JM118 that accompany the development of resistance to JM118 are quite different from the changes in the cellular pharmacology of DDP that accompany the acquisition of resistance to DDP. Thus, while repeated exposure to JM118 selects for cells that are resistant to both DDP and JM118, it activates cellular protection mechanisms different from those engaged by cells selected for acquired resistance to DDP. The finding that ovarian carcinoma cells selected for resistance to JM118 are hypersensitive to paclitaxel is of particular importance in the case of ovarian cancer because this drug is one of the single most active agents in this disease and recent randomized clinical trials have established paclitaxel-based combination chemotherapy as the standard of therapy in the United States [27, 29].
Materials and methods
Drugs
DDP and CBDCA were generously provided by Bristol-Myers Squibb (Princeton, NJ), oxaliplatin by Sanofi-Aventis (Bridgewater, NJ) and JM118 and satraplatin by GPC Biotech (Munich, Germany). DDP was stored as a 3.3 mM stock solution in 0.9% NaCl in the dark at room temperature, JM118 was stored as a lyophilized powder in the dark at −20° and satraplatin was resuspended as a stock concentration of 1 mg/ml (2 mM) in 1:1 vol/vol ethanol:water and kept in the dark at 4°. Docetaxel was provided by Sigma-Aldrich Chemie (Taufkirchen, Germany) and was resuspended as a stock concentration of 10 mg/ml (12.4 mM) in 100% ethanol. Doxorubicin and paclitaxel were purchased from Bedford Laboratories (Bedford, OH) and Bristol Myers Squibb as a 3.4 and 7 mM stock solution, respectively. Mitoxantrone was purchased from Sigma-Aldrich (St. Louis, MO) and was resuspended to a concentration of 2 mg/ml (3.9 mM) in 0.9% NaCl. Etoposide was provided by Sigma-Aldrich Chemie (Taufkirchen, Germany) and resuspended in DMSO to form a 10 mg/ml (17 mM) stock solution. DDP, satraplatin, docetaxel, doxorubicin, paclitaxel, mitoxantrone, and etoposide stock solutions were diluted directly into media. JM118 was resuspended in 1:1 vol/vol ethanol:water to form a stock solution of 1.3 mM before being diluted directly into media.
Selection of JM118 resistant cell line
The 2008 cells were maintained at 37°C in a humidified incubator containing 5% CO2 in RPMI medium supplemented with 10% fetal bovine serum. The 2008 cells were grown in T25 flasks until they were 90% confluent. JM118 was then added at a concentration approximately equivalent to the IC90 and the cells were allowed to grow in drug-containing medium until the few surviving cells began to replicate and required fresh medium. The medium was then replaced with fresh, drug-free medium and the surviving cells were further cultured until the flask was approximately 80% confluent with recovered cells. The flask was then split into four T75 flasks; one of these was used to grow cells for freezing, the others were allowed to become 90% confluent and were again exposed to JM118.
Measurement of drug sensitivity
For clonogenic assays, cells were plated into 35 mm dishes at a density of 250 cells per dish and incubated overnight to allow the cells to adhere. The following day, the medium was removed from each plate and fresh medium containing various drug concentrations was added to the cells. The cells were incubated for 7–10 days in the continuous presence of the drug to allow surviving cells to form colonies. The plates were then washed with PBS, fixed with methanol and stained with 0.1% crystal violet. Clusters containing > 50 cells were scored as colonies using an AlphaInontech Imager. Each experiment was performed with triplicate culture and was performed at three independent times.
DDP and JM118 whole cell uptake
Cells were grown until 80% confluent in 35 mm wells of six-well plates. The cells were incubated in fresh medium containing 2 μM DDP or JM118 for 24 h. The cells were then washed twice with cold PBS and lysed by addition of 215 μl 70% nitric acid to each well. The cells were then collected and dissolved at 65°C overnight, after which the samples were diluted with water/0.1% Triton-X to a final concentration of 5% acid. Each experiment was performed with triplicate wells and each experiment was performed at least three independent times. Pt measurements were made by ICP-MS using a Thermo Finnigan ICP-MS (model Element2) at the Analytical Facility at the Scripps Institute of Oceanography and normalized to protein levels for each cell line. Indium was added to each sample at 1 ppb as a control for flow variation.
Cu accumulation
For measurement of 64Cu accumulation, the six wells of a single six-well plate were used for each data point and the cells were incubated in fresh OPTI-MEM media containing 2 μM 64Cu (Mallinckrodt Institute of Radiology, Washington University Medical School, St. Louis, MO). For efflux studies, after exposure to 64Cu cells were washed three times in warm OPTI-MEM media using a rapid sampling technique and fresh, non-radioactive media was added for various time periods. The wells were then washed three times with cold PBS containing 2 μM non-radioactive CuSO4 and 10 mM EDTA, lysed with 250 μl PBS solution containing 0.1% SDS and 1.0% Triton-X 100, scraped and the wells were washed with an additional 250 μl PBS solution containing 0.1% SDS and 1.0% Triton-X 100. 64Cu was quantified by gamma counter and normalized to protein levels for each cell line.
Measurement of cellular glutathione
Three independent cultures of 2008 and 2008/JM118 cells were plated into T75 flasks and grown until ∼80% confluent. Cells were trypsinized and 1.5 × 106 cells from each culture were resuspended in 3 ml of 50 μM monochlorobimane in RPMI medium without added serum. Each culture was split into three 1 ml samples and incubated for 1 h at room temperature. One ml of 0.1 M ice cold KOH was added to each sample and the samples were mixed, incubated for 15 min after which 40 μl of 1 M sulfosalicylic acid was added and the derivatized glutathione quantified by HPLC as previously reported [25] using a 4.6 × 150 mm μBondapak C18 reverse phase column (Waters Corp., Milford, MA) and a Varian model HPLC system (Autosampler 410, solvent delivery 9010 and model 9070 fluorescence detector). Excitation and emission wavelengths were 360 and 500 nm, respectively. Data collection and processing were performed using the Varian Star 6.3 software.
Isolation and quality control of RNA for microarray hybridization
For each cell line, total RNA was harvested from three independent cultures grown until ∼70% confluent in 100 mm plates. RNA was harvested using the Qiagen RNeasy Mini Kit following the manufacturer’s instructions. RNA was quantitated by UV absorption (NanoDrop ND-1000 Spectrophotometer) and 15 μg was provided to the GeneChip Microarray Core Facility at UC San Diego. The quality of the sample RNA, including integrity/purity, was assessed using RNA 6000 Labchip Kit on the Agilent 2100 Bioanalyzer.
Hybridization to Affymetrix U133A microarrays
All steps for labeling RNA and hybridization to microarrays were performed by the GeneChip Microarray Core Facility at UC San Diego (http://www.vmrf.org/research-websites/gcf/index.html) using reagents and following protocols provided by Affymetrix (http://www.affymetrix.com/support). Briefly, double-stranded cDNA was prepared using the One-Cycle cDNA Synthesis Kit. The GeneChip IVT Labeling kit was then used to synthesize biotin-labeled cRNA, which was then fragmented prior to hybridization. The labeled, fragmented cRNA samples were then hybridized to Affymetrix U133A microarrays, washed and stained and the array was scanned according to the standard protocol available at http://www.affymetrix.com/support.
Normalization
“GCOS” expression values were produced from CEL files using GeneChip Operating Software (GCOS) version 1.2 (Affymetrix, http://www.affymetrix.com). The GCOS gene-level expression values were normalized via quantile normalization [4]. “RMA” [11] and “GCRMA” [47] and (http://www.bepress.com/jhubiostat/paper1) expression values were generated from CEL files using R statistical analysis software (http://www.r-project.org/). “RMA” output was produced using the ‘rma’ function in the ‘affy’ package and “GCRMA” output was produced using the ‘gcrma’ function in the ‘gcrma’ package. Both packages were provided by the BioConductor project [9]. Default parameters were used for the ‘rma’ and ‘gcrma’ functions. Note that both the RMA and GCRMA algorithms employ cell-level (as opposed to gene-level) quantile normalization.
Statistical analysis of microarray data
Identification of genes of interest was accomplished using significance analysis of microarrays (SAM), a statistical tool that was developed for finding differentially expressed genes in microarray experiments. It works as a Microsoft Excel add-in and is available via http://www-stat.stanford.edu/∼tibs/SAM/index.html. The cutoff for significance is determined by a tuning parameter, delta, which is chosen by the user based on the estimated false discovery rate (FDR). For this study, a threshold was selected so that the list of discovered genes would be expected to include one false discovery and SAM was applied across all six hybridizations, using normalized, absolute signals and a two-class, unpaired dataframe [42].
Statistics
Comparisons were made using Student’s t test with the assumption of unequal variance and by determining the 95% confidence interval with an alpha of 0.05.
Results
Isolation of cells resistant to JM118
Although satraplatin is currently being tested clinically for the treatment of prostate cancer, it is cytotoxic to many types of tumor cell lines. Human ovarian carcinoma 2008 cells were chosen to serve as the parental cells for the development of a JM118 resistant subline because 2008 sublines have already been selected for resistance to other Pt-containing drugs and these have been extensively characterized [1, 2, 26, 32]. JM118 was added to exponentially growing cultures of 2008 cells at a concentration of 2 μM and allowed to remain in the culture until cell growth resumed after 7–14 days. The cultures were then split and treated again with the same or progressively higher concentrations of JM118. Over the course of eight cycles of selection, the JM118 concentration was increased to 10 μM. The resulting subline, designed 2008/JM118, was subsequently grown in the absence of any further JM118 exposure. There were no observable differences in the morphology of the 2008 and 2008/JM118 cells, but the growth rate of the resistant cells was twofold slower than the parental cells. After growth of the 2008/JM118 cells for 6 months in the absence of further JM118 exposure, it was noted that they had lost a substantial amount of their resistance. These revertant cells were identified as the 2008/JM118/REV subline. Since the Pt-containing drugs are all good mutagens and, as a result, the 2008/JM118 cells are expected to contain numerous gene expression changes unrelated to the resistant phenotype, such a revertant subline is of particular value in identify those changes most closely associated with a change in drug sensitivity.
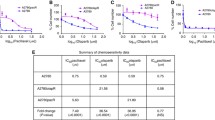
Cross resistance to other Pt-containing chemotherapeutic agents
The sensitivity of 2008 and 2008/JM118 cells to the cytotoxic effect of JM118, DDP, carboplatin, and oxaliplatin was determined using clonogenic assays with continuous drug exposure throughout the period of colony formation. As shown in Fig. 2a, based on the ratio of the slopes of the concentration–survival curves, determined from three independent experiments, the 2008/JM118 cells were 3.9 ± 1.2 (SEM)-fold resistant to JM118 (95% CI 1.5–6.2) and were cross-resistant to DDP (slope ratio 2.9 ± 0.4 (SEM); 95% CI 2.1–3.7), carboplatin [slope ratio 1.8 ± 0.2 (SEM); 95% CI 1.5–2.1] and oxaliplatin [slope ratio 3.7 ± 1.3 (SEM); 95% CI 1.3–6.2]. Thus, cells that were 3.9-fold resistant to JM118 were significantly cross-resistant to the three widely used Pt-containing drugs, and among these the greatest degree of cross-resistance was to oxaliplatin.
a sensitivity of 2008 (open square), 2008/JM118 (filled square) and 2008/JM118/REV (open triangle) cells to continuous exposure to JM118, DDP, carboplatin, oxaliplatin and satraplatin as determined by clonogenic assay. b sensitivity of 2008 (open square) and 2008/C13*5.25 (filled triangle) cells to DDP and JM118. Each data point represents the mean of three experiments performed using triplicate cultures for each drug concentration. Vertical bars ± SEM
Additional experiments were carried out to determine whether, when the 2008/JM118 cells lost resistance to JM118 over time they also lost their cross resistance to DDP, carboplatin and oxaliplatin. Figure 2a shows that this was indeed the case. The 2008/JM118/REV cells had reverted from being 3.9-fold resistant to being only 1.3 ± 0.1 (SEM)-fold resistant to JM118 relative to the 2008 cells (slope ratio for 2008/JM118 relative to 2008/JM118/REV, 3.1 ± 1.1 (SEM). In parallel, resistance to DDP decreased from 2.9-fold to 1.7 ± 0.2 (SEM)-fold, resistance to carboplatin decreased from 1.8-fold to 1.4 ± 0.2 (SEM)-fold, and resistance to oxaliplatin from 3.7 to 1.6 ± 0.3 (SEM)-fold. This provides further evidence that the same mechanism that protected the 2008/JM118 cells against JM118 also provided protection against carboplatin and oxaliplatin.
Given that the 2008/JM118 cells were cross-resistant to DDP, it was of interest to determine whether cells selected for resistance to DDP were cross-resistant to JM118. The 2008/C13*5.25 subline was originally developed by repeatedly exposing 2008 cells to DDP in a manner similar to the way in which the 2008/JM118 subline was developed [2]. The resistance of the 2008/C13*5.25 cells to DDP has remained stable for > 15 years of continuous growth in culture in the absence of further DDP exposure. As shown in Fig. 2b, while the 2008/C13*5.25 cells were 5.4 ± 0.65 (SEM)-fold resistant to DDP (95% CI 4.49–6.30), they were only 1.9 ± 0.21 (SEM)-fold resistant to JM118 (95% CI 1.64–2.12). Thus, the mechanisms that become engaged to protect 2008 cells against repeated injury by DDP also confer some protection against JM118 but the cross-resistance of DDP-selected cells to JM118 is less than the cross resistance of JM118-selected cells to DDP.
Whole cell Pt accumulation
To determine whether the differences in sensitivity to the growth inhibitory effects of JM118 were accompanied by differences in whole cell Pt accumulation, as is commonly observed in cells selected for DDP resistance [1, 24, 28, 41, 43–45], 2008 and 2008/JM118 cells were exposed to 2 μM DDP or JM118 for 1.5 or 24 h and intracellular Pt levels were quantified by ICP-MS. This low concentration of the drugs was selected to be in the range attainable in patients; however, at such low concentrations day-to-day variance in the absolute accumulation of Pt is high and it is necessary to include all the cell lines to be compared within a single experiment and base the analysis on the accumulation ratios determined from multiple independent experiments. Table 1 shows the mean whole cell accumulation of Pt in 2008 and 2008/JM118 cells. Despite their resistance to JM118, the 2008/JM118 cells accumulated modestly yet significantly more Pt following exposure to either DDP or JM118. This result is remarkable in that 2008 cells selected for resistance to DDP uniformly demonstrate reduced rather than enhanced DDP accumulation. The increase in the net uptake of both DDP and JM118 in the JM118-resistant cells indicates a type of resistance substantially different from that observed when the same cells are selected with DDP, and suggests a mechanism that detoxifies incoming drug by sequestering it into subcellular compartments and thus enhances total cell uptake. This mechanism must limit the access of these drugs to critical targets rather than increasing their export from the cell.
To further document that the mechanism that protects against JM118 and DDP toxicity in the 2008/JM118 cells is different from that which protects 2008/C13*5.25 against these drugs, whole cell accumulation was determined following exposure of 2008/C13*5.25 cells to 2 μM DDP or JM118 for 1.5 or 24 h. The data presented in Table 1 indicate the net uptake of both DDP and JM118 was reduced in the 2008/C13*5.25 cells at both time points measured. Thus, the mechanisms that become activated during selection of 2008 cells with these two drugs appear to be substantially different even though they both yield some degree of cross-resistance.
Cu homeostasis in JM118 resistant cells
Previous studies have demonstrated that the Cu efflux transporters ATP7A and ATP7B regulate sensitivity to DDP, carboplatin and oxaliplatin [20, 35, 37], and a recent study has demonstrated that this is also true for JM118 [33]. ATP7A and ATP7B appear to sequester DDP and JM118 into intracellular vesicles, thereby increasing whole cell Pt accumulation while at the same time rendering the cells resistant to the drug [34, 37]. The expression of ATP7A and ATP7B was compared in the 2008 and 2008/JM118 cells by Western blot analysis. Three independent lysates were harvested from each cell line and three independent Westerns were performed. One representative Western blot for each protein is presented in Fig. 3a. When quantified by densitometry, there was no discernable difference in expression of ATP7A or ATP7B between 2008 and 2008/JM118 cells.
Cu homeostatis in JM118-resistant cells. a western blots depicting expression of ATP7A (left) and ATP7B (right) in 2008 and 2008/JM118 cells. b accumulation and efflux of 64Cu in 2008 (open square) and 2008/JM118 (filled square) cells following a 24 exposure to 2 μM 64Cu. Each bar represents the mean of three independent experiments each performed with six replicate cultures. Vertical bars ± SEM
To confirm that the altered Pt accumulation in 2008/JM118 cells was not due to altered activity of ATP7A or ATP7B, the accumulation and efflux of 64Cu was compared between the 2008 and 2008/JM118 cells. Both types of cells were exposed to 2 μM 64Cu for 24 h and the whole cell 64Cu content was measured at the end of the loading period and at 0.5 and 1,440 min after rapid washing and incubation in Cu-free medium. The data presented in Fig. 3b indicate that, consistent with the similar levels of ATP7A and ATP7B observed on the Western blots, there was no significant difference in either whole cell accumulation or efflux of 64Cu between the sensitive and JM118-resistant cells.
Relative glutathione content of 2008 and 2008/JM118 cells
Previous studies have demonstrated a correlation between intracellular glutathione levels and satraplatin cytotoxicity [8, 30]. To determine whether JM118 resistance was a result of altered glutathione levels, glutathione was measured in 2008 and 2008/JM118 cells. In three independent experiments, each performed with triplicate samples, glutathione levels were quantified in the lysate from 0.5 × 106 cells for each cell line by HPLC. The concentration of glutathione was 331.8 ± 28.1 (SEM) nmol/106 cells in 2008 cells and 288.7 ± 7.7 (SEM) nmol/106 cells in 2008/JM118 cells. Thus, there was no significant difference in glutathione content/106 cells between 2008 and 2008/JM118 cells and no suggestion that the glutathione content was increased in the JM-resistant cells.
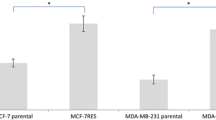
Cross resistance and collateral hypersensitivity in JM118 resistant cells
The sensitivity of 2008 and 2008/JM118 cells to the cytotoxic effect of a panel of non-Pt-containing drugs commonly used for the treatment of cancer was determined using clonogenic assays. The results, presented in Fig. 4, show that acquisition of resistance to JM118 was accompanied by cross-resistance to satraplatin, although the degree of resistance was not as great as for JM118 [slope ratio 2.6 ± 1.07 (SEM); 95% CI 1.4–3.9]. Resistance to JM118 was not accompanied by any change in sensitivity to etoposide [slope ratio 1.2 ± 0.02 (SEM); 95% CI]. However, the 2008/JM118 cells were quite hypersensitive to docetaxel [slope ratio 0.13 ± 0.04 (SEM); 95% CI 0.06–0.20], paclitaxel [slope ratio 0.27 ± 0.02 (SEM); 95% CI 0.23–0.32], doxorubicin [slope ratio 0.33 ± 0.07 (SEM); 95% CI 0.20–0.46] and to some extent to mitoxantrone [slope ratio 0.55 ± 0.17 (SEM); 95% CI 0.23–0.88]. The degree of hypersensitivity to docetaxel, paclitaxel, and doxorubicin was quite remarkable given the stringency of clonogenic assays. Because of the potential clinical significance of this observation, additional sets of three independent experiments were repeated in the same laboratory by a different investigator for paclitaxel and doxorubicin and the hypersensitivity of the 2008/JM118 cells to both of these drugs was confirmed. The mean slope ratio for the confirmatory paclitaxel experiments was 0.34 ± 0.19 (SEM) (95% CI 0.13–0.55) and for doxorubicin it was 0.33 ± 0.10 (SEM) (95% CI 0.22–0.43).
Sensitivity of 2008 (open square) and 2008/JM118 (filled square) cells to continuous exposure to etoposide, docetaxel, paclitaxel, doxorubicin and mitoxantrone as determined by clonogenic assays. For some drugs sensitivity of 2008/JM118/REV (ρ) cells was also tested. Each data point represents the mean of three experiments performed using triplicate cultures for each drug concentration. Vertical bars ± SEM
Identification of differentially expressed genes using microarray analysis
In an effort to identify genes or mechanisms that may play a role in conferring resistance to JM118, RNA from three independent flasks of each of the three cell lines growing under identical conditions was harvested and hybridized to Affymetrix U133A oligonucleotide arrays. Analyses were focused on identifying genes whose expression was altered in the 2008/JM118 cells and which reverted toward baseline in the 2008/JM118/REV cells that had lost much of their resistance to JM118. Following normalization, the statistical analysis approach developed by Tusher et al. (SAM) [42] was used to identify genes that were significantly differentially expressed between the sensitive parental cell line, the JM118-resistant and the 2008/JM118/REV sublines. This technique assigns a rank value (d-score) to each gene based on the variance of its expression across the three replicate experiments. Those gene expression values with low variance have a higher d-score compared with those values with higher variance. A cutoff is chosen by the user to identify genes with d-scores that are differentially expressed to a specified level of certainty. For these experiments, the false discovery rate was set at ∼1 gene. Given these parameters, SAM identified four genes whose transcripts were significantly more abundant and 19 genes whose transcripts were significantly less abundant in the 2008/JM118 cells than in the parental 2008 cells. These genes are listed in Table 2. Of note, none these the genes are clearly linked to mechanisms of resistance previously reported for the Pt-containing drugs. Additionally, none was found to be differentially expressed in 2008 sublines selected for resistance to DDP [6] and only one of these differentially expressed genes, phosphoribosyl pyrophosphate synthetase (PRPS1), was found to be differentially expressed in a 2008 subline selected for resistance to oxaliplatin [36].
Among the genes whose mRNA levels were altered in the 2008/JM118 cells, those whose expression reverted toward baseline as the resistance to JM118 was lost in the 2008/JM118/REV cells are potentially most directly linked to the resistance mechanism. Among the four up-regulated genes, in only one case did the reversion of expression toward baseline in the 2008/JM118/REV cells reach statistical significance. Among the 19 down-regulated genes, reversion toward baseline was significant for only six genes. These genes are listed in Table 3 along with the ratio of their expression in the 2008/JM118 and 2008/JM118/REV cells to that in the 2008 cells.
Discussion
Satraplatin is of substantial clinical interest because it can be given orally and has an attractive safety profile. One approach to identifying the mechanisms that determine sensitivity to satraplatin is to develop a cell line that has acquired resistance to its major active metabolite as a result of repeated exposure to the drug. The 2008 ovarian carcinoma cell line has been utilized extensively to study the cellular pharmacology of the Pt drugs [1, 7, 13, 23, 32]. Following eight rounds of selection, a subline that was 4.9-fold resistant to JM118 was isolated and utilized for further studies. The 2008/JM118 subline exhibited substantial cross-resistance to DDP, carboplatin and oxaliplatin, indicating that at least some of the mechanisms engaged to protect the 2008/JM118 cells against JM118 also provide protection against these other drugs. That indeed the same mechanism accounts for resistance to all these Pt drugs in the 2008/JM118 cells was further documented by the observation that as resistance to JM118 was lost so was the resistance to DDP, carboplatin, and oxaliplatin. The finding that 2008/C13*5.25 cells selected for resistance to DDP were cross-resistant to JM118 suggested that perhaps the same mechanisms are involved for both JM118 and DDP. However, there is at least one strong indication that the protective mechanisms that evolved during selection with JM118 are quite different from those that evolve during selection with DDP. The 2008/C13*5.25 cells accumulated less DDP and JM118, whereas the 2008/JM118 cells accumulated more of both drugs.
The observation that the 2008/JM118 cells accumulated significantly more Pt during a 24 h exposure to either DDP or JM118 is paradoxical but not inconsistent with recent studies suggesting that the Pt drugs are extensively sequestered into subcellular compartments that limit their access to critical targets. In some cell types, this sequestration process is accompanied by enhanced export of the drugs [14], whereas in other cell types the dominant effect is enhanced storage of drug inside the cell, presumably in a non-toxic form [35, 37].
Previous studies demonstrated that forced expression of either ATP7A or ATP7B can render cells resistant to DDP and other platinum drugs [10, 12, 15, 16, 20, 21, 35, 37]. Additionally, studies using 2008 cells engineered to over-express ATP7A demonstrated that ATP7A serves to sequester DDP and JM118 in intracellular vesicles, thereby increasing whole cell Pt accumulation while at the same time rendering the cells resistant to the drug [34, 37]. Thus, it was of interest to determine whether 2008/JM118 cells had altered expression of these Cu transporters. Western blot analysis demonstrated that there was no difference in expression of ATP7A or ATP7B and this finding was supported by studies demonstrating that there was no difference in Cu accumulation or efflux between 2008 and 2008/JM118 cells. Thus, the 2008/JM118 cells appear to utilize a mechanism of resistance that is independent of these Cu efflux transporters. The fact that resistance to JM118 is accompanied by an increase in whole cell drug uptake suggests some other sort of sequestration mechanism that limits access of the drug to critical targets but allows it to build up in the cell in a non-toxic form. The observation that there was no difference in the cellular content of glutathione in the parental and JM118-resistant cells suggests that this tripeptide is not involved in the detoxification process.
While the emergence of resistance appears to be a nearly inevitable consequence of repeated exposure to cytotoxic drugs, in rare cases the mechanisms that serve to protect the cells against one drug cause collateral hypersensitivity to another class of drugs. Although the 2008/JM118 cells showed no change in sensitivity to the topoisomerase II inhibitor etoposide, they were remarkably hypersensitive to docetaxel, paclitaxel, and doxorubicin and, to a lesser degree, to mitoxantrone. These drugs are representative of three classes of agents whose mechanism of action is quite different from each other and from that of the Pt-containing drugs. Doxorubicin and mitoxantrone trigger cellular injury primary by intercalating into DNA and inhibiting the activity of key enzymes involved in the function of DNA such as topoisomerase II [3, 22] whereas paclitaxel and docetaxel disrupt microtubule dynamics [17]. How resistance to JM118 might be linked molecularly to hypersensitivity to these unrelated classes of drugs is a matter of conjecture. Cells selected for resistance to DDP are not known to demonstrate remarkable hypersensitivity to these agents [38], an observation that provides further evidence of significant differences in the mechanisms involved in resistance to DDP and JM118. It is important to note that when resistance to JM118 waned in the 2008/JM118/REV cells, and cross-resistance to DDP, carboplatin, and oxaliplatin diminished in parallel, the hypersensitivity to paclitaxel and doxorubicin was nevertheless maintained. This suggests that the mechanisms involved in resistance to the Pt drugs and hypersensitivity to paclitaxel and doxorubicin are independent. The discovery of collateral sensitivity is promising in that it suggests that combination therapy with satraplatin and doxorubicin, mitoxantrone, paclitaxel or docetaxel may be unusually effective in the treatment of some types of malignancies, particularly for preventing the emergence of drug resistance. Alternatively, single agent therapy with any of these drugs may be effective in patients who have failed satraplatin therapy.
Expression profiling permits identification of genes that are differentially expressed in drug-sensitive and resistant cells, and sometimes elucidates the role of specific biochemical pathways. Application of the SAM technique identified only a modest number of genes that were significantly differentially expressed between the 2008 and 2008/JM118 cells, and an even smaller number in the subset whose expression reverted toward baseline when JM118 resistance faded. Caution is needed in attributing significance to these genes since the magnitude of the differences in sensitivity among the cell lines was not great. Although cell culture studies have shown that JM118 can partially overcome DDP resistance, suggesting a resistance mechanism based on tolerance or increased repair [8], few of the genes identified in the current study as being differentially expressed are recognizably associated with mechanisms such as DNA repair that have been reported to be important determinants of Pt drug sensitivity. A similar inability to link differentially expressed genes to recognized mechanisms of resistance has been observed in expression profiling studies of 2008 cells selected for resistance to cisplatin [6] and oxaliplatin [36]. However, it is noteworthy that PRPS1 (phosphoribosyl pyrophosphate synthetase 1) was found to be differentially expressed in 2008/JM118 cells as well as a 2008 subline selected for resistance to oxaliplatin [36]. PRPS plays a role in nucleotide synthesis by catalyzing the formation of phophoribosyl pyrophosphate [40]. There is no clear indication of how PRPS might be involved in acquired resistance to JM118, and further studies need to be performed in order to confirm the differential expression and determine whether altered expression of PRPS does indeed confer resistance to JM118. Nonetheless, the lack of genes identified as commonly differentially expressed in the 2008/JM118 and 2008 sublines selected for resistance to either DDP or oxaliplatin further suggests that cells engage different mechanisms to protect themselves against these three drugs even when the resulting phenotype is quite similar.
The results of this study suggest some important opportunities for the clinical development of satraplatin. First, based on differences in the mechanisms that cells utilize to defend against their toxicity, it would be reasonable to test satraplatin in diseases not responsive to cisplatin. Second, the apparent synthetic lethal interaction that results in hypersensitivity to other classes of drugs when cells become resistant to JM118 provides a strong impetus for testing combinations of satraplatin with the taxanes and doxorubicin, particularly in diseases whether there is rapid development of resistance to the Pt drugs.
Abbreviations
- DDP:
-
Cisplatin
- ICP-MS:
-
Inductively coupled plasma mass spectroscopy
- PBS:
-
Phosphate buffered saline
- PRPS:
-
Phosphoribosyl pyrophosphate synthetase
- SAM:
-
Statistical analysis of microarrays
References
Andrews PA, Albright KD (1992) Mitochondrial defects in cis-diamminedichloroplatinum(Ii) resistant human ovarian carcinoma cells. Cancer Res 52:1895–1901
Andrews PA, Murphy MP, Howell SB (1985) Differential potentiation of alkylating and platinating agent cytotoxicity in human ovarian carcinoma cells by glutathione depletion. Cancer Res 45:6250–6253
Binaschi M, Bigioni M, Cipollone A, Rossi C, Goso C, Maggi CA, Capranico G, Animati F (2001) Anthracyclines: selected new developments. Curr Med Chem Anticancer Agents 1:113–130
Bolstad BM, Irizarry RA, Astrand M, Speed TP (2003) A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. Bioinformatics 19:185–193
Boulikas T, Vougiouka M (2003) Cisplatin and platinum drugs at the molecular level. Oncol Rep 10:1663–1682
Cheng TC, Manorek G, Samimi G, Lin X, Berry CC, Howell SB (2006) Identification of genes whose expression is associated with cisplatin resistance in human ovarian carcinoma cells. Cancer Chemother Pharmacol 11:1–12
Deng HB, Parekh HK, Chow KC, Simpkins H (2002) Increased expression of dihydrodiol dehydrogenase induces resistance to cisplatin in human ovarian carcinoma cells. J Biol Chem 277:15035–15043
Fokkema E, Groen HJ, Helder MN, de Vries EG, Meijer C (2002) JM216-, JM118-, and cisplatin-induced cytotoxicity in relation to platinum-DNA adduct formation, glutathione levels and p53 status in human tumour cell lines with different sensitivities to cisplatin. Biochem Pharmacol 63:1989–1996
Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, Ellis B, Gautier L, Ge Y, Gentry J, Hornik K, Hothorn T, Huber W, Iacus S, Irizarry R, Leisch F, Li C, Maechler M, Rossini AJ, Sawitzki G, Smith C, Smyth G, Tierney L, Yang JY, Zhang J (2004) Bioconductor: open software development for computational biology and bioinformatics. Genome Biol 5:R80
Holzer AK, Samimi G, Katano K, Naerdemann W, Lin X, Safaei R, Howell SB (2004) The copper influx transporter human copper transport protein 1 regulates the uptake of cisplatin in human ovarian carcinoma cells. Mol Pharmacol 66:817–823
Irizarry RA, Bolstad BM, Collin F, Cope LM, Hobbs B, Speed TP (2003) Summaries of Affymetrix GeneChip probe level data. Nucleic Acids Res 31:e15
Ishida S, Lee J, Thiele DJ, Herskowitz I (2002) Uptake of the anticancer drug cisplatin mediated by the copper transporter Ctr1 in yeast and mammals. Proc Natl Acad Sci USA 99:14298–14302
Jennerwein M, Andrews PA (1995) Effect of intracellular chloride on the cellular pharmacodynamics of cis-diamminedichloroplatinum(II). Drug Metab Dispos 23:178–184
Katano K, Kondo A, Safaei R, Holzer A, Samimi G, Mishima M, Kuo Y-M, Rochdi M, Howell S (2002) Acquisition of resistance to cisplatin is accompanied by changes in the cellular pharmacology of copper. Cancer Res 62:6559–6565
Katano K, Safaei R, Samimi G, Holzer A, Rochdi M, Howell SB (2003) The copper export pump ATP7B modulates the cellular pharmacology of carboplatin in ovarian carcinoma cells. Mol Pharmacol 64:466–473
Katano K, Safaei R, Samimi G, Holzer A, Tomioka M, Goodman M, Howell SB (2004) Confocal microscopic analysis of the interaction between cisplatin and the copper transporter ATP7B in human ovarian carcinoma cells. Clin Cancer Res 10:4578–4588
Katsumata N (2003) Docetaxel: an alternative taxane in ovarian cancer. Br J Cancer 89(Suppl 3):S9–S15
Kelland LR (2000) An update on satraplatin: the first orally available platinum anticancer drug. Expert Opin Investig Drugs 9:1373–1382
Kelland LR, Mistry P, Abel G, Freidlos F, Loh SY, Roberts JJ, Harrap KR (1992) Establishment and characterization of an in vitro model of acquired resistance to cisplatin in a human testicular nonseminomatous germ cell line. Cancer Res 52:1710–1716
Komatsu M, Sumizawa T, Mutoh M, Chen Z-S, Terada K, Furukawa T, Yang X-L, Gao H, Miura N, Sugiyama T, Akiyama S (2000) Copper-transporting P-type adenosine triphosphatase (ATP7B) is associated with cisplatin resistance. Cancer Res 60:1312–1316
Lin X, Okuda T, Holzer A, Howell SB (2002) The copper transporter CTR1 regulates cisplatin uptake in saccharomyces cerevisiae. Mol Pharmacol 62:1154–1159
Malonne H, Atassi G (1997) DNA topoisomerase targeting drugs: mechanisms of action and perspectives. Anticancer Drugs 8:811–822
Marverti G, Andrews PA (1996) Stimulation of cis-diamminedichloroplatinum(II) accumulation by modulation of passive permeability with genistein: an altered response in accumulation-defective resistant cells. Clin Cancer Res 2:991–999
Metcalfe SA, Cain K, Hill BT (1986) Possible mechanisms for differences in sensitivity to cis-platinum in human prostate tumor cell lines. Cancer Lett 31:163–169
Miquel J (1993) (eds) CRC handbook of free radicals and antioxidants in biomedicine. CRC, Florida
Mishima M, Samimi G, Kondo A, Lin X, Howell SB (2002) The cellular pharmacology of oxaliplatin resistance. Eur J Cancer 38:1405–1412
Muggia FM, Braly PS, Grady MF, Sutton G, Niemann TH, Lentz SL, Alvarez RD, Kucera PR, Small JM (2000) Phase III randomized study of cisplatin versus paclitaxel versus cisplatin and paclitaxel in patients with suboptimal stage III or IV ovarian cancer: a gynecologic oncology group study. J Clin Oncol 18:106–115
Oldenburg J, Begg AC, van Vugt MJH, Ruevekamp M, Schornagel JH, Pinedo HM, Los G (1994) Characterization of resistance mechanisms to cis-diamminedichloroplatinum (II) in three sublines of the CC531 colon adenocarcinoma cell line in vitro. Cancer Res 54:487–493
Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, Mannel RS, DeGeest K, Hartenbach EM, Baergen R (2003) Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol 21:3194–3200
Raynaud FI, Odell DE, Kelland LR (1996) Intracellular metabolism of the orally active platinum drug JM216: influence of glutathione levels. Br J Cancer 74:380–386
Reardon JT, Vaisman A, Chaney SG, Sancar A (1999) Efficient nucleotide excision repair of cisplatinum, oxaliplatin, and bis-aceto-ammine-dichloro-cyclohexylamine-platinum(IV) (JM216) platinum intrastrand DNA diadducts. Cancer Res 59:3968–3971
Safaei R, Katano K, Larson BJ, Samimi G, Holzer AK, Naerdemann W, Tomioka M, Goodman M, Howell SB (2005) Intracellular localization and trafficking of fluorescein-labeled cisplatin in human ovarian carcinoma cells. Clin Cancer Res 11:756–767
Samimi G, Howell SB (2005) The effect of the copper transporters ATP7A and ATP7B on the cytotoxicity and cellular pharmacology of JM-118. Proc Am Assoc Cancer Res 46:969
Samimi G, Howell SB (2006) Modulation of the cellular pharmacology of JM118, the major metabolite of satraplatin, by copper influx and efflux transporters. Cancer Chemother Pharmacol 57:781–788
Samimi G, Katano K, Holzer AK, Safaei R, Howell SB (2004) Modulation of the cellular pharmacology of cisplatin and its analogs by the copper exporters ATP7A and ATP7B. Mol Pharmacol 66:25–32
Samimi G, Manorek G, Castel R, Breaux JK, Cheng TC, Berry CC, Los G, Howell SB (2005) cDNA-microarray-based identification of genes and mechanisms associated with oxaliplatin resistance. Cancer Chemother Pharmacol 55:1–11
Samimi G, Safaei R, Katano K, Holzer AK, Rochdi M, Tomioka M, Goodman M, Howell SB (2004) Increased expression of the copper efflux transporter ATP7A mediates resistance to cisplatin, carboplatin and oxaliplatin in ovarian cancer cells. Clin Cancer Res 10:4661–4669
Siddik ZH (2003) Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene 22:7265–7279
Sternberg CN, Whelan P, Hetherington J, Paluchowska B, Slee PH, Vekemans K, Van Erps P, Theodore C, Koriakine O, Oliver T, Lebwohl D, Debois M, Zurlo A, Collette L (2005) Phase III Trial of Satraplatin, an oral platinum plus Prednisone vs. Prednisone alone in patients with hormone-refractory prostate cancer. Oncology 68:2–9
Tatibana M, Kita K, Taira M, Ishijima S, Sonoda T, Ishizuka T, Iizasa T, Ahmad I (1995) Mammalian phosphoribosyl-pyrophosphate synthetase. Adv Enzyme Regul 35:229–249
Teicher BA, Holden SA, Herman TS, Sotomayor EA, Khandekar V, Rosbe KW, Brann TW, Korbut TT, Frei E 3rd (1991) Characteristics of five human tumor cell lines and sublines resistant to cis-diamminedichloroplatinum(II). Int J Cancer 47:252–260
Tusher VG, Tibshirani R, Chu G (2001) Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci USA 98:5116–5121
Twentyman PR, Wright KA, Mistry P, Kelland LR, Murrer BA (1992) Sensitivity to novel platinum compounds of panels of human lung cancer cell lines with acquired and inherent resistance to cisplatin. Cancer Res 52:5674–5680
Wallner KE, DeGregorio MW, Li GC (1986) Hyperthermic potentiation of cis-diamminedichloroplatinum(II) cytotoxicity in Chinese hamster ovary cells resistant to the drug. Cancer Res 46:6242–6245
Waud WR (1987) Differential uptake of cis-diamminedichloro-platinum(II) in sensitive and resistant murine L1210 leukemia cell lines. Cancer Res 46:6549–6555
Acknowledgments
The authors would like to thank Annette Dehyle, Ph.D. of the Scripps Institute of Oceanography Analytical Facility for technical assistance and Katja Wosikowski, Ph.D. for advice. The production of 64Cu at Washington University School of Medicine was supported by the NCI grant R24 CA86307.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samimi, G., Kishimoto, S., Manorek, G. et al. Novel mechanisms of platinum drug resistance identified in cells selected for resistance to JM118 the active metabolite of satraplatin. Cancer Chemother Pharmacol 59, 301–312 (2007). https://doi.org/10.1007/s00280-006-0271-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-006-0271-0