Abstract
Peripheral neuropathy is induced by multiple doses of oxaliplatin and interferes with the clinical utility of the drug in patients with colorectal cancer. In this study, we sought to determine whether cell loss or selective neuronal damage was the basis for the peripheral neuropathy caused by oxaliplatin. Adult female rats were given 1.85 mg/kg oxaliplatin twice per week for 8 weeks. Nerve conduction and L5 dorsal root ganglia (DRG) were studied 1 week after the completion of all treatment. No mortality occurred during oxaliplatin treatment, but the rate of body weight gain was reduced compared to age-matched vehicle-treated controls. Oxaliplatin slowed conduction velocity and delayed conduction times in peripheral sensory nerves, without affecting central or motor nerve conduction. In L5 DRG, total numbers of neurons were unchanged by oxaliplatin, but there were significant reductions in neuronal size distribution, ganglion volume, average cell size and the relative frequency of large cells. In addition, the relative frequency of small DRG cells was increased by oxaliplatin. Oxaliplatin significantly altered the size distribution and average cell body area of the predominantly large parvalbumin-immunoreactive DRG neurons without affecting the frequency of parvalbumin staining. On the contrary, neither the staining frequency nor the size distribution of the predominantly small substance P-immunoreactive DRG neurons was changed by oxaliplatin. In conclusion, oxaliplatin causes selective atrophy of a subpopulation of DRG neurons with predominantly large parvalbumin-expressing cells without inducing neuronal loss. Because DRG cell body size and axonal conduction velocity are positively correlated, neuronal atrophy may be the morphological basis for the development of decreased sensory nerve conduction velocity that characterizes oxaliplatin-induced peripheral neuropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oxaliplatin is a new platinum-based drug with clinical efficacy against colorectal cancer [34], a disease widely considered to be resistant to most existing chemotherapy drugs including cisplatin and carboplatin. After intracellular transformation, oxaliplatin intermediates react with DNA to form platinum-DNA adducts, which exert cytotoxicity by inhibiting DNA replication, halting progression through the mitotic cell cycle and inducing apoptosis in dividing cells [39]. Oxaliplatin forms the same type of DNA lesions at the same sites as cisplatin and carboplatin but these DNA adducts are bulkier, less easily recognized by DNA repair proteins and less susceptible to DNA replicative bypass. In three large randomized clinical trials comparing 5-fluorouracil and leucovorin alone or with oxaliplatin in patients with colorectal cancer, higher response rates and prolonged disease-progression-free survival times have been documented in the oxaliplatin-containing arms [12, 17, 20]. On this basis, oxaliplatin is now approved in many countries for the treatment of colorectal cancer as initial therapy or at disease progression after first-line chemotherapy. Oxaliplatin-induced peripheral neuropathy is the most frequent dose-limiting toxicity associated with therapy and currently there is no treatment available. With the expanding medical use of oxaliplatin, an increasing number of patients are at risk of developing this adverse effect.
Oxaliplatin neuropathy is characterized by the development of paraesthesias, dysaesthesias, proprioceptive loss and decreased tendon reflexes in a glove and stocking distribution, which are associated with reduced velocity and amplitude of sensory nerve conduction on neurophysiological testing [8, 16, 21]. The severity of the neuropathy is closely related to the cumulative dose of oxaliplatin, as evidenced by the occurrence of dose-limiting neurotoxicity in 10% and 50% of patients after cumulative doses of 780 and 1170 mg/m2, respectively [21]. After repeated doses, most patients develop some signs or symptoms of peripheral neuropathy and there is a tendency for recovery after the cessation of treatment. In addition, oxaliplatin causes an acute syndrome of generalized peripheral nerve hyperexcitability, which is short-lived, reversible and potentially avoidable by taking action to keep away from known precipitating factors [30, 46] and, therefore, of less concern than its cumulative neuropathy. The cause of the cumulative neuropathy is unclear and it appears to be unrelated to the amount of platinum accumulating within the peripheral nervous system [26, 41, 42]. Histological and biodistribution studies suggest that the cell bodies of peripheral sensory neurons and the dorsal root ganglia (DRG) are major sites of damage [10, 26, 32, 41, 42]. However, because DRG neurons do not undergo mitosis or DNA replication, the neurotoxicity mechanism must differ from the antitumour action of oxaliplatin discussed above.
The cumulative neuropathy induced by oxaliplatin has many similarities to the peripheral neuropathy caused by cisplatin. There have been many previous studies of the effect of chronic cisplatin treatment on the DRG of rats [9, 33, 44]. A common finding of these cisplatin studies is a decrease in cell body, nuclear and nucleolar size of DRG neurons after treatment. Some reports conclude that the change in DRG cell size indicates neuronal atrophy because of the lack of morphological evidence of cell death [4, 33, 44]. However, other studies have shown apoptosis of DRG neurons occurring after cisplatin treatment, which in turn could lead to altered DRG size profiles and other signs of peripheral neuropathy [15, 18]. In addition, it is unclear whether the cisplatin effects occur generally among all DRG neurons or specifically within a particular subpopulation of cells. For instance, Tomiwa et al. [44] described morphological changes in the cell bodies of most DRG neurons, but the clinical syndrome is more consistent with selective damage to the subpopulation of DRG neurons with large myelinated fibres.
Like cisplatin, oxaliplatin has been shown to decrease DRG neuronal cell body, nucleus and nucleolus size parameters after chronic treatment in rats [10, 26]. The published studies, however, do not shed light on the selectivity of oxaliplatin-induced damage among different populations of DRG cells, or on the role of neuronal loss in the development of oxaliplatin-induced peripheral neuropathy. We sought to address these two issues in the current study. To investigate the selectivity of oxaliplatin-induced DRG neuronal damage, we studied two immunohistochemically distinct DRG cell populations that stained positively with either parvalbumin or substance P. Parvalbumin and substance P have been previously described as cell markers for predominantly large and predominantly small DRG neuronal subpopulations, respectively [7, 11, 13, 25]. In addition, stereological counting techniques [37, 45] have been used to obtain estimates of the total number of neurons in L5 DRG from oxaliplatin-treated rats and age-matched vehicle-treated control animals. These investigations were carried out under conditions that resulted in unambiguous changes in nerve conduction and DRG neuronal size profiles so that any alteration in immunohistochemically defined subpopulations or total DRG neuronal counts could be related back to the established effects of oxaliplatin.
Materials and methods
Animals
Age-matched 10-week-old female Wistar rats weighing between 200 and 300 g at the start of experimentation were used in this study. Oxaliplatin (Sigma, St. Louis, Mo.) was made up for injection in 5% dextrose (Baxter Healthcare, Old Toongabbie, Australia). Animals were treated twice weekly with either oxaliplatin at a dose of 1.85 mg/kg or the vehicle control solution of 5% dextrose. Drug and vehicle solutions were administered by intraperitoneal (i.p.) injection at a volume of 15 ml/kg twice per week (Monday and Friday) for 8 weeks. Injections were performed between 1300 and 1500 hours to avoid possible time-dependent variability in pharmacokinetics and pharmacodynamics. All animal procedures complied with ethical guidelines and had approval from the Animal Ethics Committee of the University of Auckland and met the requirements of the UKCCCR guidelines. Animals had unrestricted access to food and water and were housed in a temperature-controlled environment.
Nerve conduction studies
Nerve conduction studies were carried out 1 week after the completion of all treatment, as previously described [31]. In brief, animals were lightly anaesthetized with an intramuscular injection of Hypnorm (Janssen Pharmaceutica, Beerse, Belgium) diluted 1:1 in milli-Q water. M-action potentials and H-action potentials were generated by electrical stimulation of the peripheral nerves at the sciatic notch and the ankle of the left hind limb using percutaneous needle electrodes. A pair of superficial silver/silver chloride electrodes applied to the sole and dorsum of the left hind limb was used to record the M-waves and H-waves in the plantar muscles. Conduction time in the peripheral sensory nerve was calculated from the H-wave latency after distal stimulation minus the H-wave latency after proximal stimulation. Conduction time in the central monosynaptic spinal reflex arc was calculated from the H-wave latency after proximal stimulation minus the M-wave latency after proximal stimulation. Conduction time in the peripheral motor nerve was calculated from the M-wave latency after proximal stimulation minus the M-wave latency after distal stimulation. Time of distal motor neurotransmission was taken from the M-wave latency after distal stimulation. Sensory nerve conduction velocity was calculated by dividing the distance between the proximal and distal stimulation sites by the difference in H-wave latency between the proximal and distal stimulation sites. Motor nerve conduction velocity was calculated by dividing the distance between the proximal and distal stimulation sites by the difference in M-wave latency between the proximal and distal stimulation sites. It was not possible to study the recovery of neuropathy in the post-treatment period because of the previously described delayed-onset peritoneal reactions and mortality occurring after repeated i.p. oxaliplatin treatment [10, 26].
DRG morphometry
One week after the conclusion of the 8-week dosing period, following the nerve conduction studies, animals were killed using 0.9 ml of 3 mg/ml pentobarbitone (Chemstock Animal Health, Christchurch, New Zealand). Subsequent to anaesthesia, the animals were perfused by administering 60 ml of 0.9% sodium chloride (Baxter Healthcare) followed by 60 ml of 4% paraformaldehyde in 0.1 M phosphate buffer into the left ventricle of the heart. L5 DRG were carefully dissected from each animal and stored in 4% paraformaldehyde until processing. DRG were processed by washing in water, dehydrating through a series of alcohols, and cleared in xylene prior to being embedded in paraffin wax. DRG were cut by a microtome into 6-μm sections, which were mounted onto glass slides with DPX mounting medium (Scharlau Chemie, Barcelona, Spain) and stained with haematoxylin and eosin. Each DRG produced approximately 80–130 sections. A total of five sections were picked at regular intervals from each DRG, and the cell body area was measured for each cell containing a nucleus or nucleolus to generate a histogram of cell body size. DRG cells were divided into three size categories: small (cell body area <750 μm2), medium (750–1750 μm2) and large (>1750 μm2), as previously documented in similar studies [5, 38, 48].
Stereology
The volume of the DRG was estimated using the Cavalieri method [23]. The cross-sectional areas of 10–15 equally spaced sections were measured and the mean value was calculated. DRG volume was then calculated by multiplying the mean cross-sectional area by the mean section thickness and the number of sections.
Cell counting was performed using the physical disector principle [37, 45]. An unbiased counting frame with an area of 40,036 μm2 was randomly assigned to each sampled section. Cells with nuclei or nucleoli were counted if they were found within the counting frame but not touching the top or left side borders. Only cells present in the reference section that were not present in the corresponding look-up section, separated from each reference section by 6 μm, were counted. The sum of all cells counted from 20 equally spaced reference sections was divided by the summed volume of all the physical disectors, which in turn was calculated from the area of the reference section multiplied by the section thickness, to give the number of cells per unit volume. Finally, to generate the total number of cells in each DRG, the number of cells per unit volume was multiplied by the volume of the ganglion. All morphometric parameters were analysed by light microscopy. Microscopic images were digitally photographed using an Axiocam camera (Carl Zeiss Vision, Hallbergmoos, Germany) and morphometric analysis was performed using AxioVision 3.0 software (Carl Zeiss Software, Hallbergmoos, Germany).
Immunohistochemistry
DRG were perfused and dissected as described above. Dissected DRG were post-fixed in 4% PFA for 2–6 h then stored in 30% sucrose in PBS solution until the tissues sunk. Once sunken, the DRG were frozen with Tissue-Tek OCT compound (Sakura Finetek, Torrance, Calif.) and stored at −80°C prior to cutting on the cryostat. Each DRG was sectioned in the cryostat at a thickness of 10 μm and transferred to poly-lysine coated slides, which were then stored at −80°C.
For immunostaining, frozen tissue slides were warmed to room temperature and washed in PBS containing 0.2% Triton X-100. The slides were then incubated in 1% H2O2 in 50% methanol for 10 min to prevent endogenous peroxidase activity. Subsequently, slides were rewashed in PBS, then placed in PBS containing 3% normal goat serum (Sigma) and 20 mg/ml bovine serum albumin (Sigma) for 1 h to block non-specific binding. The slides were incubated overnight with either rabbit anti-parvalbumin (PVA3) primary antibody (1:1000; P. Emson, Cambridge, UK) or rabbit anti-substance P primary antibody (1:20,000; Watpa Enterprises, Auckland, New Zealand) at room temperature. Following several washes in PBS containing 0.2% Triton X-100, slides were incubated with a biotinylated secondary anti-rabbit antibody (1:500; Sigma) for 2.5 h at room temperature. After further washes in PBS, slides were incubated for 3 h at room temperature in extravidin-peroxidase conjugate (1:500; Sigma). Finally, slides were washed in PBS, before staining was visualized with 0.5 mg/ml 3,3′-diaminobenzidine tetrahydrochloride (AppliChem, Darmstadt, Germany) and 0.01% H2O2 in 0.4 M phosphate buffer for 10 min. After further washes in PBS, slides were dehydrated through a series of alcohols, cleared in xylene and coverslipped with DPX mounting medium.
For DRG analysis, slides were analysed by light microscopy and AxioVision 3.0 software. DRG cells stained for parvalbumin or substance P containing nuclei or nucleoli were counted and their cross-sectional areas were measured. Each cell in the DRG cross-section was also counted, regardless of immunostaining, to generate the frequency of cells containing parvalbumin or substance P immunostaining.
Statistical analysis
The statistical significance of differences between means was assessed using unpaired t-tests and two-way analysis of variance (ANOVA). Differences in cell size distribution were analysed by the Wilcoxon Rank-Sum test. In all statistical tests a P value of <0.05 indicated statistical significance. Neurophysiological and morphological parameters were corrected for individual body weight but this correction did not substantially alter any of the relative differences between mean values or their statistical significance. Therefore, data are presented uncorrected for body weight.
Results
Body weight and general toxicity
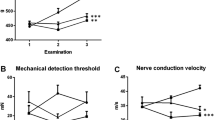
A total of 60 adult female rats were treated with 1.85 mg/kg oxaliplatin or the drug vehicle by i.p. injection twice per week for 8 weeks. No mortality occurred during the treatment period, but oxaliplatin significantly reduced the rate of body weight gain compared to vehicle-treated controls (44.8±2.7 g vs 74.5±2.3 g over 8 weeks; P<0.0001, unpaired t-test; Fig. 1). There were no signs of toxicity during the treatment period but ascites was present in several oxaliplatin-treated rats at dissection despite their healthy pre-mortem appearance. Nerve conduction and L5 DRG were studied 1 week after the completion of treatment.
Nerve conduction studies
Nerve conduction studies were carried out in the left hind-limb. The peripheral nerve was stimulated electrically at distal and proximal sites, i.e., at the ankle and sciatic notch. The time delay between stimulation and arrival of M and H action potentials in the plantar muscles was recorded and used to derive conduction times and velocities in different parts of the reflex arc (Table 1). The conduction time in the peripheral sensory nerve was significantly slowed by oxaliplatin (+12% change relative to control, P<0.005, unpaired t-test). However, conduction times in the central monosynaptic spinal reflex arc, peripheral motor nerve and distal motor neurotransmission were unchanged. Conduction velocity was unchanged in the peripheral motor nerves but significantly reduced in sensory nerves (−5.4 m/s absolute change relative to control; P<0.005, unpaired t-test).
L5 DRG morphometry and cell size distribution
To determine the basis for the altered nerve conduction, the cell bodies of the peripheral sensory neurons, which are located within the DRG, were studied. DRG volume, total cell number per DRG and neuronal size profiles were determined. Oxaliplatin significantly reduced DRG volume (−36.3% change relative to control; P<0.05, unpaired t-test), but had no effect on the total number of neurons per DRG (Table 2). The size distribution of DRG neurons, determined by their cross-sectional cell body areas, was significantly altered by oxaliplatin (P <0.001, Wilcoxon Rank-Sum Test). Oxaliplatin induced a leftward shift in the size distribution histogram due to a decreased frequency of larger cells and an increased frequency of smaller cells (Fig. 2). Averaged cell body area was also significantly reduced by 23.2% from 857 to 658 μm2 following oxaliplatin treatment (P<0.02; unpaired t-test). When DRG neurons were categorized on the basis of size into small (<750 μm2), medium (750–1750 μm2) and large (>1750 μm2) cells, oxaliplatin significantly reduced the relative frequency of large cells (−82.1% change relative to control; P<0.05, unpaired t-test) and increased the relative frequency of small cells (+16.9% change relative to control; P<0.005, unpaired t-test). There was no change in the relative frequency of medium-sized cells.
Parvalbumin and substance P immunohistochemistry
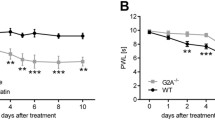
To investigate whether there was any selectivity in the oxaliplatin-induced changes in DRG neurons, rat DRG were immunostained for parvalbumin, a marker of predominantly large DRG neurons [7, 11], and substance P, a marker of predominantly small DRG neurons [25]. The size distribution and staining frequency of immunoreactive cells was determined. Oxaliplatin significantly altered the cross-sectional size distribution of parvalbumin-immunopositive DRG neurons (P<0.001, Wilcoxon Rank-Sum Test; Fig. 3a, b). Oxaliplatin induced a leftward shift in the size distribution histogram of parvalbumin-immunopositive DRG neurons by reducing the number of large cells and increasing the number of small cells staining for parvalbumin. The mean cross-sectional cell area of parvalbumin-immunoreactive cells was significantly decreased (−32.4% change relative to control, P<0.001, unpaired t-test), but there was no change in the staining frequency of parvalbumin-immunoreactive cells following oxaliplatin treatment (Table 3). When parvalbumin-immunoreactive DRG neurons were categorized on the basis of size into small (<750 μm2), medium (750–1750 μm2) and large (>1750 μm2) cells, the relative frequency of large parvalbumin-immunoreactive cells was significantly reduced by oxaliplatin (−93.0% change relative to control, P<0.02, unpaired t-test), while the relative frequency of small cells was significantly increased (+115.2% change relative to control, P<0.005, unpaired t-test). Oxaliplatin did not alter the neuronal size distribution, the mean cell body area or the staining frequency of substance P-immunoreactive DRG neurons (Fig. 3c, d).
Discussion
In the present study, we found changes in sensory nerve conduction in the hind limb of rats after multiple doses of oxaliplatin that indicated the development of a peripheral neuropathy. Peripheral neuropathy is an important clinical side effect of oxaliplatin since it is the most frequent dose-limiting toxicity encountered with the drug in cancer patients [21]. After multiple doses of oxaliplatin, patients develop progressive symptoms of impaired peripheral sensory nerve function, such as paraesthesias, dysaesthesias, motor incoordination and sensory ataxia, which are associated with reductions in the amplitude and velocity of sensory nerve conduction [8, 14, 16]. We utilized a rat model to investigate oxaliplatin neuropathy by measuring the delay in the arrival of action potentials in the plantar muscles of the hind limb after peripheral nerve stimulation. These H-reflex action potentials travel from the site of peripheral nerve stimulation proximally along sensory nerve fibres, through the monosynaptic spinal reflex arc and then distally along motor nerve fibres before reaching the plantar muscles [43]. By separating the H-reflex pathway into its components, we showed that oxaliplatin induced a delay in conduction localized to the sensory nerve fibres without affecting conduction within the motor fibres or central reflex arc. This oxaliplatin-induced alteration in conduction within the sensory component of the H-reflex arc is comparable to the previously reported changes in tail nerve conduction in oxaliplatin-treated rats [10]. In addition, this conduction delay is qualitatively similar to that associated with the development of oxaliplatin-induced peripheral neuropathy in cancer patients. Despite these similarities, caution is necessary in extrapolating the results of the current study to oxaliplatin neuropathy in patients, because of potential variations in treatment conditions, developmental status or other parameters between the experimental and clinical situations.
We then studied the L5 DRG of rats that had shown delayed conduction of H-reflex action potentials after treatment with oxaliplatin. Many of the sensory nerve fibres within the H-reflex pathway are supplied by the L5 DRG. Neuronal loss is an important mechanism in some forms of peripheral neuropathy [35], but oxaliplatin did not alter the total number of L5 DRG cells. Validated counting methods [37, 45] showed similar counts of approximately 14,000 neurons in control and oxaliplatin-exposed ganglia, which are comparable to cell numbers reported in previous L5 DRG studies in rats [22, 27, 36]. In contrast, overall ganglion size, average cell size, neuronal size distributions and the relative frequency of large cells were significantly reduced by oxaliplatin. The alterations in neuronal size profile were similar to those reported previously in the DRG of rats after chronic oxaliplatin treatment [10, 26]. So, the results of the current study show that the changes in sensory nerve conduction induced by oxaliplatin were associated with atrophy of L5 DRG neurons without any significant loss of cells.
The effect of oxaliplatin on subpopulations of DRG cells, defined by their expression of parvalbumin and substance P, was then investigated. Parvalbumin and substance P immunostaining identified distinct DRG cell populations with little or no overlap in their immunoreactivity and size profiles. In the present study, parvalbumin was expressed in about 14% of DRG neurons, consisting of predominantly medium and large-diameter cells, while substance P was expressed in about 12% of DRG neurons, which were almost exclusively small cells. Previous studies of rat lumbar DRG have shown similar size profiles, similar staining frequencies and virtually no coexisting expression of parvalbumin and substance P within the same cell [13, 28]. Oxaliplatin induced neuronal atrophy in parvalbumin-expressing cells without altering the size of substance P-expressing cells. In comparison, cisplatin has been previously reported to increase [4], decrease [40] and not alter [2] the DRG expression of substance P. However, in our study, oxaliplatin did not alter the staining frequency of either population consistent with there being no loss of cells. This indicates that neuronal atrophy was induced selectively in cells expressing parvalbumin but not in cells expressing substance P that lacked parvalbumin.
The mechanism of oxaliplatin neurotoxicity is unclear, but appears to be selective for cells that express parvalbumin, i.e., predominantly large cells. Parvalbumin is a calcium-binding protein that is expressed by distinct subpopulations of nerve cells that tend to have high electrical or metabolic activities [3]. Parvalbumin-expressing cells may require calcium-binding proteins to regulate specific calcium-dependent processes, such as the calcium-dependent activation of sodium channels. Neuronal sodium channels have been implicated in the neurotoxicity mechanism of oxaliplatin [1, 19], and different subpopulations of DRG neurons differ in their pattern of expression of specific sodium channels [6]. We therefore propose that the mechanism of oxaliplatin neuropathy might involve calcium-binding proteins, sodium channels or other targets that are coexpressed with parvalbumin. If the mechanism of oxaliplatin neuropathy involved sodium channels then a link might be provided between its acute and chronic neurotoxicities.
For DRG neurons, there is a positive correlation between cell body size and the velocity of signal conduction within their peripherally directed axons [24, 29, 47]. Larger cells have faster conducting axons because they give rise to thicker and myelinated fibres, which are associated with more rapid conduction. Small DRG cells give rise to slower conducting axons that are thin and unmyelinated. In the present study, we demonstrated a reduction in sensory nerve conduction velocity after multiple doses of oxaliplatin in the rat that was characteristic of the development of a peripheral neuropathy. Associated with these changes in nerve conduction were reductions in the size of the cell bodies of L5 DRG neurons. Since these two parameters are positively correlated, it is plausible that the reduced cell body size could have led to the reduced sensory nerve conduction velocity. Atrophy of the predominantly large DRG neurons may therefore be the morphological basis for the development of the decreased sensory nerve conduction velocity that characterizes oxaliplatin-induced neuropathy.
In conclusion, in the present study we found changes in sensory nerve conduction in the hind limb of rats after multiple doses of oxaliplatin that indicated the development of a peripheral neuropathy. This was associated with atrophy of a subpopulation of L5 DRG neurons without any significant loss of cells. Neuronal atrophy was induced selectively in parvalbumin-expressing cells suggesting a mechanism of oxaliplatin neuropathy involving calcium-binding proteins or an alternative target that is coexpressed with parvalbumin in DRG cells. Because DRG cell body size is positively related to axonal conduction velocity, neuronal atrophy may be the morphological basis for the development of the sensory nerve functional deficits that characterize oxaliplatin-induced neuropathy.
References
Adelsberger H, Quasthoff S, Grosskreutz J, Lepier A, Eckel F, Lersch C (2000) The chemotherapeutic oxaliplatin alters voltage-gated Na(+) channel kinetics on rat sensory neurons. Eur J Pharmacol 406:25–32
Apfel SC, Arezzo JC, Lipson L, Kessler JA (1992) Nerve growth factor prevents experimental cisplatin neuropathy. Ann Neurol 31:76–80
Baimbridge KG, Celio MR, Rogers JH (1992) Calcium-binding proteins in the nervous system. Trends Neurosci 15:303–308
Barajon I, Bersani M, Quartu M, Del Fiacco M, Cavaletti G, Holst JJ, Tredici G (1996) Neuropeptides and morphological changes in cisplatin-induced dorsal root ganglion neuronopathy. Exp Neurol 138:93–104
Bergman E, Ulfhake B (1998) Loss of primary sensory neurons in the very old rat: neuron number estimates using the disector method and confocal optical sectioning. J Comp Neurol 396:211–222
Black JA, Dib-Hajj S, McNabola K, Jeste S, Rizzo MA, Kocsis JD, Waxman SG (1996) Spinal sensory neurons express multiple sodium channel alpha-subunit mRNAs. Brain Res Mol Brain Res 43:117–131
Carr PA, Yamamoto T, Karmy G, Baimbridge KG, Nagy JI (1989) Analysis of parvalbumin and calbindin D28k-immunoreactive neurons in dorsal root ganglia of rat in relation to their cytochrome oxidase and carbonic anhydrase content. Neuroscience 33:363–371
Cascinu S, Catalano V, Cordella L, Labianca R, Giordani P, Baldelli AM, Beretta GD, Ubiali E, Catalano G (2002) Neuroprotective effect of reduced glutathione on oxaliplatin-based chemotherapy in advanced colorectal cancer: a randomized, double-blind, placebo-controlled trial. J Clin Oncol 20:3478–3483
Cavaletti G, Tredici G, Marmiroli P, Petruccioli MG, Barajon I, Fabbrica D (1992) Morphometric study of the sensory neuron and peripheral nerve changes induced by chronic cisplatin (DDP) administration in rats. Acta Neuropathol 84:364–371
Cavaletti G, Tredici G, Petruccioli MG, Donde E, Tredici P, Marmiroli P, Minoia C, Ronchi A, Bayssas M, Etienne GG (2001) Effects of different schedules of oxaliplatin treatment on the peripheral nervous system of the rat. Eur J Cancer 37:2457–2463
Celio MR (1990) Calbindin D-28k and parvalbumin in the rat nervous system. Neuroscience 35:375–475
de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A (2000) Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 18:2938–2947
Ernfors P, Lee KF, Kucera J, Jaenisch R (1994) Lack of neurotrophin-3 leads to deficiencies in the peripheral nervous system and loss of limb proprioceptive afferents. Cell 77:503–512
Extra JM, Marty M, Brienza S, Misset JL (1998) Pharmacokinetics and safety profile of oxaliplatin. Semin Oncol 25:13–22
Fischer SJ, McDonald ES, Gross L, Windebank AJ (2001) Alterations in cell cycle regulation underlie cisplatin induced apoptosis of dorsal root ganglion neurons in vivo. Neurobiol Dis 8:1027–1035
Garufi C, Pietrangeli A, Brienza S, Mari AA, Pace R, Giannarelli D, Mari DR, Zappala A, Vaccaro A, Mari DA, Iandolo B, Nistico C, Terzoli E (1999) Electrophysiological evaluation of oxaliplatin neurotoxicity (abstract 938). Proc Am Soc Clin Oncol 18:244a
Giacchetti S, Perpoint B, Zidani R, Le Bail N, Faggiuolo R, Focan C, Chollet P, Llory JF, Letourneau Y, Coudert B, Bertheaut-Cvitkovic F, Larregain-Fournier D, Le Rol A, Walter S, Adam R, Misset JL, Levi F (2000) Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol 18:136–147
Gill JS, Windebank AJ (1998) Cisplatin-induced apoptosis in rat dorsal root ganglion neurons is associated with attempted entry into the cell cycle. J Clin Invest 101:2842–2850
Grolleau F, Gamelin L, Boisdron-Celle M, Lapied B, Pelhate M, Gamelin E (2001) A possible explanation for a neurotoxic effect of the anticancer agent oxaliplatin on neuronal voltage-gated sodium channels. J Neurophysiol 85:2293–2297
Grothey A, Deschler B, Kroening H, Ridwelski K, Reichardt P, Kretzschmar A, Clemens M, Hirschmann W, Lorenz M, Asperger W, Buechele T, Schmoll H-J (2002) Phase III study of bolus 5-fluorouracil (5-FU)/folinic acid (FA) (Mayo) vs weekly high-dose 24h 5-FU infusion/FA + oxaliplatin (OXA) (FUFOX) in advanced colorectal cancer (ACRC) (abstract 512). Proc Am Soc Clin Oncol 21:129a
Grothey A (2003) Oxaliplatin-safety profile: neurotoxicity. Semin Oncol 30:5–13
Groves MJ, An SF, Giometto B, Scaravilli F (1999) Inhibition of sensory neuron apoptosis and prevention of loss by NT-3 administration following axotomy. Exp Neurol 155:284–294
Gundersen HJ, Jensen EB (1987) The efficiency of systematic sampling in stereology and its prediction. J Microsc 147:229–263
Harper AA, Lawson SN (1985) Conduction velocity is related to morphological cell type in rat dorsal root ganglion neurones. J Physiol 359:31–46
Hokfelt T, Kellerth JO, Nilsson G, Pernow B (1975) Substance P: localization in the central nervous system and in some primary sensory neurons. Science 190:889–890
Holmes J, Stanko J, Varchenko M, Ding H, Madden VJ, Bagnell CR, Wyrick SD, Chaney SG (1998) Comparative neurotoxicity of oxaliplatin, cisplatin, and ormaplatin in a Wistar rat model. Toxicol Sci 46:342–351
Kishi M, Tanabe J, Schmelzer JD, Low PA (2002) Morphometry of dorsal root ganglion in chronic experimental diabetic neuropathy. Diabetes 51:819–824
Lawson SN (1992) Morphological and biochemical cell types of sensory neurons. In: Scott SA (ed) Sensory neurons: diversity, development and plasticity. Oxford University Press, New York, pp 27–59
Lee KH, Chung K, Chung JM, Coggeshall RE (1986) Correlation of cell body size, axon size, and signal conduction velocity for individually labelled dorsal root ganglion cells in the cat. J Comp Neurol 243:335–346
Lehky TJ, Leonard GD, Wilson RH, Grem JL, Floeter MK (2004) Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve 29:387–392
McKeage MJ, Boxall FE, Jones M, Harrap KR (1994) Lack of neurotoxicity of oral bisacetatoamminedichlorocyclohexylamine-platinum(IV) in comparison to cisplatin and tetraplatin in the rat. Cancer Res 54:629–631
McKeage MJ, Hsu T, Screnci D, Haddad G, Baguley BC (2001) Nucleolar damage correlates with neurotoxicity induced by different platinum drugs. Br J Cancer 85:1219–1225
Muller LJ, Gerritsen van der Hoop R, Moorer-van Delft CM, Gispen WH, Roubos EW (1990) Morphological and electrophysiological study of the effects of cisplatin and ORG.2766 on rat spinal ganglion neurons. Cancer Res 50:2437–2442
O’Dwyer PJ, Johnson SW (2003) Current status of oxaliplatin in colorectal cancer. Semin Oncol 30:78–87
Peltier AC, Russell JW (2002) Recent advances in drug-induced neuropathies. Curr Opin Neurol 15:633–638
Popken GJ, Farel PB (1997) Sensory neuron number in neonatal and adult rats estimated by means of stereologic and profile-based methods. J Comp Neurol 386:8–15
Pover CM, Coggeshall RE (1991) Verification of the disector method for counting neurons, with comments on the empirical method. Anat Rec 231:573–578
Price J (1985) An immunohistochemical and quantitative examination of dorsal root ganglion neuronal subpopulations. J Neurosci 5:2051–2059
Raymond E, Faivre S, Woynarowski JM, Chaney SG (1998) Oxaliplatin: mechanism of action and antineoplastic activity. Semin Oncol 25:4–12
Schmidt Y, Unger JW, Bartke I, Reiter R (1995) Effect of nerve growth factor on peptide neurons in dorsal root ganglia after taxol or cisplatin treatment and in diabetic (db/db) mice. Exp Neurol 132:16–23
Screnci D, Er HM, Hambley TW, Galettis P, Brouwer W, McKeage MJ (1997) Stereoselective peripheral sensory neurotoxicity of diaminocyclohexane platinum enantiomers related to ormaplatin and oxaliplatin. Br J Cancer 76:502–510
Screnci D, McKeage MJ, Galettis P, Hambley TW, Palmer BD, Baguley BC (2000) Relationships between hydrophobicity, reactivity, accumulation and peripheral nerve toxicity of a series of platinum drugs. Br J Cancer 82:966–972
Stanley EF (1981) Sensory and motor nerve conduction velocities and the latency of the H reflex during growth of the rat. Exp Neurol 71:497–506
Tomiwa K, Nolan C, Cavanagh JB (1986) The effects of cisplatin on rat spinal ganglia: a study by light and electron microscopy and by morphometry. Acta Neuropathol 69:295–308
West MJ (1999) Stereological methods for estimating the total number of neurons and synapses: issues of precision and bias. Trends Neurosci 22:51–61
Wilson RH, Lehky T, Thomas RR, Quinn MG, Floeter MK, Grem JL (2002) Acute oxaliplatin-induced peripheral nerve hyperexcitability. J Clin Oncol 20:1767–1774
Yoshida S, Matsuda Y (1979) Studies on sensory neurons of the mouse with intracellular-recording and horseradish peroxidase-injection techniques. J Neurophysiol 42:1134–1145
Zhang X, Wiesenfeld-Hallin Z, Hokfelt T (1994) Effect of peripheral axotomy on expression of neuropeptide Y receptor mRNA in rat lumbar dorsal root ganglia. Eur J Neurosci 6:43–57
Acknowledgements
This study was supported by a grant from the Cancer Society of New Zealand. Stephen Jamieson is the recipient of a University of Auckland Doctoral Scholarship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jamieson, S., Liu, J., Connor, B. et al. Oxaliplatin causes selective atrophy of a subpopulation of dorsal root ganglion neurons without inducing cell loss. Cancer Chemother Pharmacol 56, 391–399 (2005). https://doi.org/10.1007/s00280-004-0953-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-004-0953-4