Abstract
Recently a major research effort has been focused on the development of anticancer drugs by targeting the components of a biochemical pathway to induce apoptosis in cancerous cells. Some of the natural products (e.g. paclitaxel) have been proven to be useful in inducing apoptosis in cancer cells with limited specificity. Pancratistatin, a natural product isolated and characterized over a decade ago, has been shown to be cytostatic and antineoplastic. We investigated the specificity and biochemical mechanism of action of pancratistatin. Pancratistatin seemed to show more specificity than VP-16 or paclitaxel as an efficient inducer of apoptosis in human lymphoma (Jurkat) cells, with minimal effect on normal nucleated blood cells. Caspase-3 activation and exposure of phosphatidyl serine on the outer leaflet of the plasma membrane were earlier events than the generation of ROS and DNA fragmentation observed following pancratistatin treatment. This indicates a possible involvement of caspase-3 and plasma membrane proteins in the induction phase of apoptosis. Our results indicate that pancratistatin does not cause DNA double-strand breaks or DNA damage prior to the execution phase of apoptosis in cancer cells. Parallel experimentation with VP-16, a currently used medication for cancer treatment, indicated that VP-16 causes substantial DNA damage in normal non-cancerous blood cells, while pancratistatin does not cause any DNA double-strand breaks or DNA damage in non-cancerous cells. Taken together, our finding that pancratistatin induces apoptosis in cancer cells using non-genomic targets, and more importantly does not seem to have any affect non-cancerous cells, presents a significant platform to develop non-toxic anticancer therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite an extensive research effort to conquer cancer, this disease remains irremediable. The research effort towards cancer has become centralized around the mechanism of apoptosis since its discovery [15]. Apoptosis is a physiological process involving a cell suicide program that is essential in normal development and tissue homeostasis [8, 10]. This process is characterized by cell shrinkage and nuclear condensation [13]. The biochemical pathways involved in apoptosis offer a variety of targets for inducing the cell suicide program that eliminates cancer cells. Several research groups have been successful in inducing apoptosis by targeting specific components of the cell [11].
Most of the currently used anticancer treatments, including chemotherapeutics and radiotherapies, are capable of triggering apoptotic cell death in cancer cells by causing DNA damage. Unfortunately, these treatments come with the consequence of causing toxicity to normal cells due to the fact that cancer cells tend to differ from normal cells in their DNA replication mechanism and rate of proliferation. For example, etoposide (VP-16), a topoisomerase II inhibitor, is known to be a genotoxic anticancer drug [5] that may exhibit this toxicity against normal cells. This damage to normal cells is most relevant in the recurrence of cancer in patients because mutations caused by these therapies may predispose normal cells to become cancerous. There are very few anticancer drugs that are capable of targeting receptors or other components of the cell without producing any genotoxic effects.
Current therapies thought to be non-genotoxic include paclitaxel and tamoxifen [1, 6]. Since the discovery of the potent anticancer activity of the natural product paclitaxel, scientific efforts have been made to find other natural products capable of specifically targeting cancerous cells. Although it was believed that paclitaxel induces non-genotoxic apoptosis by stabilizing tubulin, it has only recently been shown to be genotoxic [9]. Recently, natural products such as N-thiolated β-lactam and a labdane diterpene have been found to specifically target cancer cells in inducing apoptosis. However, the concentrations of these compounds required to induce apoptosis are high and their toxicity against normal blood cells is not known [14, 25]. Pancratistatin is a natural compound first isolated in 1992 from the spider lily [22]. It has been shown to have antineoplastic and cytostatic activity [18, 22], but its biochemical mechanism of action is still unknown. The critical evaluation of the specificity and efficacy of pancratistatin in targeting cancer cells and its toxicity against normal non-cancerous cells are yet to be established.
In the present work, we evaluated the efficacy of pancratistatin in inducing apoptosis in Jurkat cells and its effect on normal non-cancerous counterparts. Since blood is one of the body’s first lines of defense and all blood cells get exposed to any drug administered, it was important for us to determine the toxicity of pancratistatin against normal nucleated blood cells (lymphocytes). We report an interesting and exciting finding that pancratistatin is capable of effectively inducing apoptosis specifically in cancerous cells within a short period of time at a very low concentration. Interestingly, in all experiments, no toxic effect of pancratistatin treatment was found in normal blood cells. More importantly, no DNA damage was detected following pancratistatin treatment of these cells. On the other hand, VP-16 was clearly genotoxic to cancerous as well as normal blood cells. We further studied the mechanism of action of pancratistatin by investigating the effects of pancratistatin on caspase-3 activation, ROS production and DNA damage by sensitive procedures. The results of these experiments were further compared with those of experiments with the currently used chemotherapeutic agent, VP-16.
An interesting observation made with regard to the mechanism of action of pancratistatin in cancer cells was the rapid activation of caspase-3 and flipping of phosphatidyl serine to the outer leaflet of the plasma membrane in the pathway of apoptosis. These results collectively suggest that pancratistatin could be a very effective and nontoxic alternative for anticancer therapy.
Materials and methods
Cell cultures
A human lymphoma cell line (Jurkat cells) was purchased from ATCC (Manassas, Va.). These cells were grown and maintained in an incubator set at 37°C with an atmosphere containing 5% CO2 and of 95% humidity. These cells were cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS) and 40 μg/ml gentamicin (Life Technologies, Mississauga, Ontario).
Human nucleated blood cells were purified from whole blood obtained from healthy male and female volunteers as approved by the University of Windsor ethical committee, REB# 04-060. Whole blood (7 ml) was collected into a BD Vacutainer CPT tube (Cell Preparation Tube) obtained from Becton Dickinson (Franklin Lakes, N.J.). The whole blood was spun down in a table-top low-speed centrifuge at 2900 g for 30 min at 25°C. The red blood cells went through the polyester gel and the top layer containing mononuclear cells, platelets and plasma was collected. These cells were kept in the same incubator as the Jurkat cells (37°C, 5% CO2 and 95% humidity).
Cell treatment
For the induction of apoptosis by treatment with pancratistatin, Jurkat cells were grown to 70% confluence and then treated for varying periods of time. Pancratistatin was isolated from Hymenocallis following the literature scheme (99% pure) [22]. Jurkat cells were directly treated with pancratistatin at a concentration of 1 μM or as indicated. Normal nucleated blood cells were treated in a similar manner after being purified from whole blood. In a parallel set of separate experiments involving VP-16 treatments, VP-16 (Sigma Chemical Company, Mississauga, Ontario) was also directly added to the culture medium, but to a final concentration of 10 μM (which is the concentration currently used clinically).
Cellular staining and viability assay
To examine the viability of Jurkat cells after treatment, a cell suspension was added to 20 μl of 0.4% trypan blue stain (Life Technologies). Using a hemacytometer (Fisher Scientific, Horsham, Pa.), both dead (trypan blue-positive) and live cells were counted four times. The results were then calculated and tabulated as percentage of dead cells using Microsoft Excel 6.0 software.
To examine apoptotic morphology changes, the Jurkat cells and lymphocytes were grown and treated, and then stained with cell-permeable Hoechst 33342 (Molecular Probes, Eugene, Ore.) at a final concentration of 10 μM and incubated for 5 min at 37°C. The cells were then examined under a fluorescent microscope (Leica DM IRB, Germany) and both phase-contrast and fluorescent pictures were taken. Five fields of fluorescent pictures taken at 100x magnification were used to count apoptotic versus live cells (where brightly stained cells with condensed nuclei were considered apoptotic). These results were then calculated and tabulated as percentage of apoptotic cells using Microsoft Excel 6.0 software. The pictures at higher magnification were compiled using Adobe Photoshop 7.0 software.
Comet assay
The comet assay was performed using a slight modification of a previously published method [21]. Briefly, the slides were precoated with 0.10% agarose and left to dry for at least 30 min. The desired cell suspension was added to 50 μl of 0.75% warm low-melting point agarose and immediately spread over the precoated slide. The slides were placed at 4°C for 5 min to solidify, and then immersed in cold lysis buffer comprising 2.5 mM NaCl, 100 mM Na2EDTA, 10 mM Tris at pH 10, 1% Triton X-100, and 10% DMSO for 1 h at 4°C. Following incubation, slides were washed in alkaline electrophoresis buffer comprising 0.3 M NaOH and 1 mM Na2EDTA at pH >13. The DNA was electrophoresed at 300 mA (0.8 V/cm) for 30 min, washed in neutralizing buffer (0.4 M Tris, pH 7.5) and stained with 10 μM Hoechst 33342. The cells were examined under a fluorescent microscope (Leica DM IRB) and fluorescence pictures were taken. All pictures were processed using Adobe Photoshop 7.0 software.
Annexin-V binding assay
After treating Jurkat cells and lymphocytes, the annexin-V binding assay was conducted using a purchased kit and the manufacturer’s protocol (catalog no. A13201, Molecular Probes). After treatment, cells were washed in phosphate-buffered saline (PBS) and resuspended in annexin-V binding buffer (10 mM HEPES/NaOH pH 7.5, 140 mM NaCl, 2.5 mM CaCl2), containing 1:50 annexin-V Alexa Fluor 488 conjugate for 15 min at room temperature. Cells were then examined under a fluorescent microscope (Leica DM IRB), and fluorescence pictures were taken. All pictures were processed using Adobe Photoshop 7.0 software.
Caspase-3 activity
The caspase-3 assay was performed using a previously published method [21]. To determine the caspase-3 activity, the total protein from Jurkat or lymphocyte cell lysates was incubated with a fluorogenic substrate (DEVD-AFC), a tetrapeptide sequence corresponding to the substrate cleavage site. The caspase assay was carried out according to the manufacturer’s protocol (Enzyme System Products, USA). The fluorescence was measured at an excitation wavelength of 400 nm and emission wavelength of 505 nm using a Spectra Max Gemini XS (Molecular Devices, Sunnyvale, Calif.). Caspase-3 activity was calculated per microgram of protein, and protein concentration was determined with BioRad protein assay reagent (BioRad, Mississauga, Ontario) using bovine serum albumin as a standard. Microsoft Excel 6.0 software was used for data representation and statistical analysis.
Mitochondrial membrane potential
Control and treated Jurkat cells were stained with 0.5 μM Mitotracker CM-XH2-Ros dye (Molecular Probes) to determine mitochondrial membrane potential. After 30 min at 37°C, Jurkat cells were spun down and resuspended in PBS. The cells were examined under a fluorescent microscope (Leica DM IRB). Fluorescence pictures were taken; all pictures were processed using Adobe Photoshop 7.0 software.
Measurement of total ROS generation
After cells were treated, production of total reactive oxygen species (ROS) in Jurkat cells and lymphocytes was measured using the membrane permeable dye 2’,7’-dichlorofluorescein diacetate (DCFDA) (Molecular Probes) and a slight modification of a previously published procedure [24]. The cells were incubated in DCFDA at 37°C for 30 min, and fluorescence was measured at an excitation wavelength of 500 nm and emission wavelength of 524 nm using a Spectra Max Gemini XS multiwell plate fluorescence reader (Molecular Devices). Fluorescence readings were expressed in terms of the total cell count per well, determined using trypan blue staining. Microsoft Excel 6.0 software was used for data representation and statistical analysis.
H2AX staining
Jurkat cells and lymphocytes were grown and treated, and the pellet was resuspended in 4% paraformaldehyde and incubated. The cell suspension was added to a slide precoated with 0.01% poly-l-lysine (Sigma) and allowed to dry on the slide. The slides were washed with PBS three times for 5 min each time and incubated in 70% ethanol for 5 min. The slides were washed again and then incubated in 10% FBS in PBS for 1 h followed by an additional washing with PBS. After incubation for 1 h with the primary antibody, 1:300 anti-phosphohistone H2AX (Upstate Biotechnology, Lake Placid, N.Y.), the slides were washed again with PBS. The cells were then incubated in secondary antibody, 1:200 anti-mouse IgG-conjugated to FITC (Sigma) for 1 h and washed with PBS. The slides were stained with Hoechst 33342 and washed again with PBS. A glass coverslip was mounted over the dried slides using Cytoseal mounting medium (VWR, Mississauga, Ontario). The slides were examined under a confocal microscope (BioRad MRC600) using oil immersion and pictures were taken. All pictures were processed using Adobe Photoshop 7.0 software.
Results
Induction of apoptosis by pancratistatin in Jurkat cells
In order to evaluate the efficacy of pancratistatin in inducing cell death in cancer cells, we carried out experiments to determine the concentration- and time-dependent effects of pancratistatin on Jurkat cells. Jurkat cells were treated with different concentrations of pancratistatin for 6 h and stained with Hoechst dye, and apoptotic cells were counted as described in “Materials and methods”. At a concentration as low as 500 nM, pancratistatin was efficient in causing approximately a third of the cells to undergo apoptosis (Fig. 1a). At 1.0 μM, however, more than 70% of the Jurkat cells were apoptotic, meaning that apoptosis was effectively being induced. Hence, in all following experiments, this effective concentration of 1.0 μM was used.
a Induction of apoptosis in Jurkat cells treated with different concentrations of pancratistatin. Jurkat cells were treated with various concentrations of pancratistatin as indicated. After 6 h of treatment, the cells were stained with Hoechst dye and the percentage of apoptotic cells (the apoptotic index) determined. A minimum of five different fields at 100x magnification were counted and an average was taken for each experiment. The standard error was calculated using the data from three separate sets of experiments. b Induction of apoptosis over time in Jurkat and normal blood cells treated with pancratistatin. Jurkat or normal blood cells were treated with 1.0 μM pancratistatin for the indicated times. The apoptotic index was calculated as described above using a minimum of five different fields per experiment at 100x magnification. The standard error was calculated using the data from three separate sets of experiments. c Trypan blue staining for dead and live Jurkat cells treated with pancratistatin. Jurkat cells were treated with pancratistatin for the indicated times. The cells were then stained with trypan blue dye so that the number of dead cells could be determined. The results are presented as the percentage of permeabilized (dead) cells. A minimum of eight different fields at 100x magnification were counted and an average was taken for each experiment. The standard error was calculated using the data from three separate sets of experiments. d Nuclear and cellular morphology of Jurkat cells treated with pancratistatin. The cells were treated with pancratistatin at 1.0 μM for the indicated times. Cells were then stained with Hoechst to examine nuclear morphology. Phase-contrast and fluorescence pictures were taken as described in “Materials and methods”. Pictures were taken at 400x magnification. Apoptosis is evident in cells with bright, condensed and rounded nuclei. e DNA degradation in Jurkat cells treated with pancratistatin as indicated by the comet assay. Jurkat cells were treated with either solvent (control, 0.001% DMSO) or 1.0 μM pancratistatin for 24 h. The comet assay was then performed as described in “Materials and methods”. Pictures were taken at 400x magnification. DNA degradation is indicated by the comet-like images due to migration of damaged DNA during electrophoresis. f Induction of the flipping of phosphatidyl serine in the plasma membrane of Jurkat cells by pancratistatin treatment. After the treatment with pancratistatin at 1.0 μM for the indicated times, the annexin-V binding assay was performed as described in “Materials and methods”. Fluorescence indicates the flipping of phosphatidyl serine to the outer leaflet of the plasma membrane. Pictures were taken at 400x magnification
Further examination of the time kinetics of cell death triggered by 1.0 μM pancratistatin indicated that apoptosis was detected as early as within 1 h of treatment (Fig. 1b). More than 90% of the Jurkat cells displayed apoptotic morphology after 24 h of treatment whereas normal blood cells remained unaffected (Fig. 1b). Results of trypan blue staining to determine the number of permeabilized cells (Fig. 1c) indicated that apoptotic cells were eventually becoming necrotic. This is evident by a higher percentage of apoptotic cells than dead cells within a short time of treatment, as seen by comparing data from Fig. 1b and c.
Apoptotic characteristics including cellular and nuclear morphology and biochemical features were studied in Jurkat cells with various times of pancratistatin treatment. Hoechst staining clearly indicated typical nuclear morphological changes induced by apoptosis, such as increased brightness of the nuclei and nuclear condensation (Fig. 1d). DNA fragmentation is another key feature of apoptosis that was examined by using the comet assay as previously described [21]. The presence of a comet after 24 h indicated that massive apoptotic DNA fragmentation had occurred in most of the Jurkat cells (Fig. 1e).
A specific biochemical characteristic of apoptosis is the flipping of phosphatidyl serine from the inner leaflet of the plasma membrane to the outer leaflet. This change can be observed as an increase in fluorescence due to the binding of the annexin-V Alexa Fluor conjugate to phosphatidyl serine. As shown in Fig. 1f, annexin-V binding was obvious after 1 h of pancratistatin treatment in Jurkat cells, indicating early activation of the pathway of apoptosis. These results collectively illustrate that pancratistatin is a very potent inducer of apoptosis in Jurkat cells.
Normal nucleated blood cells including lymphocytes are not affected by pancratistatin
Normal lymphocytes purified from a healthy person are the best candidates to determine the effect of pancratistatin on non-cancerous cells in comparison to the effect on cancerous Jurkat cells. These cells respond differently than Jurkat cells when subjected to pancratistatin treatment under similar conditions. We investigated the sensitivity of nucleated blood cells including lymphocytes to pancratistatin by quantifying the degree of apoptosis as with Jurkat cells. Unlike the Jurkat cells, the apoptotic index of the pancratistatin-treated lymphocytes did not increase over a significant amount of time (up to 24 h, Fig. 1b). Furthermore, the nuclear blebbing and brightness detected in Jurkat cells were not visible in the normal lymphocytes (Fig. 2a). This suggests that apoptosis was not being induced in normal non-cancerous blood cells. Moreover, there was no increase in fluorescence following the annexin-V binding assay (Fig. 2b), implying that this apoptotic event was not present following treatment of lymphocytes with pancratistatin. The pathway of apoptosis is therefore not activated by pancratistatin in normal lymphocytes as it is in Jurkat cells.
a Nuclear morphology of Jurkat and normal blood cells treated with pancratistatin. Cells were treated with solvent (control, 0.001% DMSO) or 1.0 μM pancratistatin and incubated for 24 h. Pictures were taken at 400x magnification. Apoptosis is evident in cells with bright, condensed and rounded nuclei. b Specific induction of the flipping of phosphatidyl serine in the plasma membrane of Jurkat cells by pancratistatin treatment. After 3 h of treatment with 1.0 μM pancratistatin, the annexin-V binding assay was performed as described in “Materials and methods”. Fluorescence indicates the flipping of phosphatidyl serine to the outer leaflet of the plasma membrane only in Jurkat cells, not in normal blood cells. Pictures were taken at 400x magnification
Pancratistatin provokes early activation of caspase-3 in Jurkat cells, but not in normal lymphocytes
Caspase-3 is a required component of the apoptotic machinery which is activated specifically in the pathway of apoptosis. To determine whether pancratistatin treatment caused caspase-3 activation, the activity of caspase-3 was assayed in cell extracts prepared at different times after pancratistatin treatment. There was an early increase in caspase-3 activity upon treatment of Jurkat cells (Fig. 3) indicating that caspase-3 might be involved in the early phase of apoptosis induced by pancratistatin in Jurkat cells. This increase in activity was not evident in lymphocytes, again illustrating that pancratistatin does not induce apoptosis in lymphocytes (data not shown).
Early activation of caspase-3 in Jurkat cells treated with pancratistatin. The caspase-3 assay was performed as described in “Materials and methods”. The average of nine readings was used to determine the reading for each well. A minimum of three wells were run per experiment and the average was taken for each experiment. The results were calculated per microgram of protein and the standard error was calculated using the data from three separate sets of experiments
Role of mitochondria in pancratistatin-induced apoptosis in Jurkat cells
The collapse of the mitochondrial membrane potential is a common event in the apoptotic pathway that leads to mitochondrial dysfunction and production of ROS. Mitotracker Red staining was carried out as described in “Materials and methods” to assess the mitochondrial membrane potential. Figure 4a clearly illustrates that the mitochondrial membrane potential in Jurkat cells was not lost prior to activation of caspase-3 by pancratistatin treatment. Furthermore, total cellular ROS was measured using the redox-sensitive fluorescent dye DCFDA, and the readings further confirmed that the production of ROS occurred after activation of caspase-3 (Fig. 4b). Little ROS production relative to Jurkat cells was also observed in normal blood cells (data not shown).
a The effect of pancratistatin treatment on the mitochondrial membrane potential of Jurkat cells. Jurkat cells were treated with solvent (control, 0.001% DMSO) or 1.0 μM pancratistatin for 30 min and stained with Mitotracker Red as described in “Materials and methods”. fluorescence indicates that the mitochondrial membrane potential is intact. Pictures were taken at 400x magnification. b Generation of ROS in Jurkat cells treated with pancratistatin. ROS production was determined using DCFDA as described in “Materials and methods”. The average of nine readings was used to determine the reading for each well. A minimum of three wells were run per experiment and the average was taken for each experiment. The results were calculated per 10,000 cells and the standard error was calculated using the data from three separate sets of experiments
Pancratistatin is a non-genotoxic inducer of apoptosis as compared to VP-16
Pancratistatin treatment of Jurkat cells caused caspase-3 activation and ROS production within 3 h, but no comet had been produced at this time. This indicates that DNA degradation is not an early event in the pathway of apoptosis induced by pancratistatin in Jurkat cells. On the other hand, VP-16 had clearly produced comets at this time (Fig. 5a). This absence of DNA degradation by pancratistatin at an early phase, and its presence in a later phase indicates that DNA degradation is a result of the apoptotic mechanism. With VP-16, the DNA damage was detected very early, which indicates that apoptosis was caused by DNA damage. These results signify that pancratistatin is a non-genotoxic inducer of apoptosis in Jurkat cells in contrast to VP-16 which is a known genotoxic anticancer drug.
a Detection of DNA degradation at an early phase of treatment in Jurkat cells. Jurkat cells were treated with solvent (control, 0.001% DMSO), 1.0 μM pancratistatin or 10 μM VP-16 for 3 h. The comet assay was then performed as described in “Materials and methods”. Pictures were taken at 400x magnification. DNA degradation is indicated by the comet-like images due to migration of damaged DNA during electrophoresis. b Detection of DNA DSB by H2AX staining. Cells were treated with solvent (control, 0.001% DMSO), 1.0 μM pancratistatin or 10 μM VP-16 for various times as indicated. Bright fluorescence indicates the presence of DNA DSB. Pictures were taken at a magnification of 600x using oil immersion
In order to rule out the possibility of DNA double-strand breaks (DSB) caused by pancratistatin, we performed antiphosphohistone H2AX immunostaining. This assay is one of the most sensitive methods of detecting DNA fragmentation in mammalian cells [23]. Phosphorylation of the histone H2AX, symbolized by γ-H2AX, is one of the earliest events of DNA repair in response to DSB. Hence a positive staining indicates the presence of DSB [4, 12, 19]. As shown in Fig. 5b, pancratistatin did not stain for H2AX at the early time point of 3 h. This illustrates that indeed pancratistatin does not induce DSB in Jurkat cells; however we cannot rule out the possibility of single-strand breaks. A positive staining in VP-16-treated cells confirms that this drug truly is a genotoxic anticancer drug.
VP-16 induces genotoxicity in normal cells
Although it has clearly been proven that VP-16 (a topoisomerase-II inhibitor) is genotoxic to cancerous cells [5], we decided to test its effect on the DNA of normal blood cells. VP-16 treatment caused DNA damage as seen by comet formation, demonstrating its genotoxic effect on lymphocytes (Fig. 6a). The absence of comets in normal blood cells (lymphocytes) treated with pancratistatin indicated that it may not cause DNA damage (Fig. 6a). These results indicate that VP-16 is genotoxic to Jurkat cells as well as normal lymphocytes whereas pancratistatin did not show any sign of genotoxicity to normal nucleated blood cells even after 24 h. This was further confirmed by the fact that no H2AX staining was observed following pancratistatin treatment, but was clearly evident following VP-16 treatment (Fig. 6b). Therefore, unlike VP-16, pancratistatin specifically induces apoptosis in Jurkat cells, but does not seem to affect lymphocytes.
a Effect of pancratistatin and VP-16 treatment on the DNA integrity of normal blood cells. Normal blood cells were treated with solvent (control, 0.001% DMSO), 1.0 μM pancratistatin or 10 μM VP-16 for 24 h. The comet assay was then performed as described in “Materials and methods”. Pictures were taken at 400x magnification. DNA degradation is indicated by the comet-like images due to migration of damaged DNA during electrophoresis. b Detection of DNA DSB in normal blood cells treated with VP-16. Cells were treated with solvent (control, 0.001% DMSO), 1.0 μM pancratistatin or 10 μM VP-16 for 3 h. Fluorescence indicates the presence of DNA DSB. Pictures were taken at a magnification of 600x using oil immersion
Discussion
We report here for the first time that pancratistatin is selective in inducing apoptosis strictly in cancerous cells (specifically Jurkat cells). Second, since the chemical structure of pancratistatin does not resemble any existing genotoxic chemicals, DNA is unlikely to be a direct target of this drug. Due to the desperation for a treatment, several genotoxic drugs are currently being used to target this disease. Unfortunately, we have found that some of these drugs, such as VP-16 and paclitaxel are toxic to normal blood cells.
Although pancratistatin has been studied for many years, most of the research done on this drug has been in the field of organic chemistry [16, 17, 20]. For this reason, little information is available regarding its biochemical activity. However, it has been found that the pharmacophore of this drug is capable of specifically killing cancerous cells by inducing apoptosis.
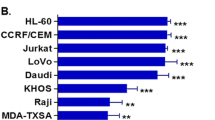
The rapid and efficient induction of classical apoptosis by a very low concentration of pancratistatin in human lymphoma cells illustrates that this chemical is very specifically targeting a biochemical component of the apoptotic pathway. More importantly, however, is the fact that pancratistatin left the normal blood cells unaffected both biochemically and morphologically after 24 h. We have also tested the effect of pancratistatin on other normal non-cancerous cells, including dividing human fibroblasts, and human embryonic endothelial cells, and have found that it is not effecting the population doubling or viability of these cells (McLachlan et al., unpublished results). On the other hand, VP-16, a commonly used chemotherapeutic agent, causes DNA damage in normal nucleated cells. This suggests that pancratistatin is a more specific inducer of apoptosis in cancer cells than currently used drugs such as VP-16. We have also observed that paclitaxel causes apoptosis in normal nucleated cells (data not shown). Although the efficacy of pancratistatin was highest in Jurkat cells, we have shown that it is also effective in inducing apoptosis in various cell lines, including MCF-7, rat hepatoma, neuroblastoma and skin carcinoma cells.
What is therefore the biochemical target of pancratistatin? DNA is a less likely target of pancratistatin action since is not structurally similar to any known genotoxic drugs. Our results from the comet assay further confirmed that indeed there is no early DNA degradation, but that DNA fragmentation is a late event in the apoptotic cascade resulting from pancratistatin treatment. In contrast, VP-16 caused massive DNA damage at an early phase (3 h). Furthermore, we applied H2AX staining, a sensitive technique to monitor DNA DSB. This indicated that pancratistatin did not induce DSB, whereas VP-16 caused DSB soon after treatment. These experiments imply that pancratistatin could be a non-genotoxic compound that induces apoptosis by targeting non-genomic targets.
It is commonly accepted that a mitochondrial target can trigger apoptosis. This would suggest that pancratistatin might be targeting the mitochondrial membrane. However, this possibility was ruled out because our preliminary results indicated that within a short time of treatment, there was neither depolarization of the mitochondrial membrane nor production of ROS.
Interestingly, during the first hour, the apoptotic events triggered by pancratistatin were found to be the flipping of phosphatidyl serine on the plasma membrane and the activation of caspase-3. Surprisingly, this activation of caspase-3 came before that of caspase-8 which was found to be activated only after 3 h of treatment (data not shown). This evidence leads to two possibilities: pancratistatin directly activates caspase-3 or pancratistatin is targeting an enzyme on the plasma membrane. Incubation of a cell extract from untreated Jurkat cells with pancratistatin did not result in the activation of caspase-3 thus indicating that pancratistatin was not directly interacting with caspase-3 (data not shown).
The other possible mechanism includes interaction with the plasma membrane and cytosolic proteins as a target for pancratistatin. Receptor-mediated Fas induced-apoptosis in Jurkat cells is one of the best-studied biochemical pathways [3]. It is generally believed that caspase-8 is recruited to the death-inducing signaling complex (DISC) following oligomerization of the Fas receptor. It is this initiator caspase of DISC that cleaves and activates caspase-3 as well as the Bid protein [7]. Intriguingly, it has been recently shown that caspase-3 is recruited to the DISC and processed to its active form before activation of caspase-8 or mitochondrial depolarization [2]. Recently evidence has also been found suggesting that caspase-3 may be present in the plasma membrane of the cell [2]. It is possible that pancratistatin may be directly targeting the Fas receptors on the plasma membrane of blood lymphoma cells which further activates caspase-3 followed by the activation of caspase-8. This is our hypothesis currently under investigation. Our preliminary results have indicated that indeed there is a significant increase in caspase-3 activity following pancratistatin treatment in the plasma membrane fraction of Jurkat cells (data not shown).
With this mechanism of action, why are normal cells not being affected by pancratistatin? This could be due to the expression of the Fas receptors which is found to be greater in blood lymphoma cells than normal blood cells. Furthermore, in fast-dividing cancer cells, the plasma membrane tends to run short of lipids, perhaps changing the fluidity of the membrane.
We are aggressively pursuing this hypothesized mechanism of action of pancratistatin in cancerous cells. Current investigation is underway to determine exactly what the biochemical targets of pancratistatin are on blood lymphoma cells. Given the significance of our in vitro results, pancratistatin could be a much better chemotherapeutic agent than those presently available.
References
Abal M, Andreu JM, Barasoain I (2003) Taxanes: microtubule and centrosome targets, and cell cycle dependent mechanisms of action. Curr Cancer Drug Targets 3:193–203
Aouad SM, Cohen LY, Sharif-Askari F, Haddad EK, Alam A, Sekaly RP (2004) Caspase-3 is a component of Fas death-inducing signaling complex in lipid rafts and its activity is required for complete caspase-8 activation during Fas-mediated cell death. J Immunol 172(4):2316–2323
Ashkenazi A, Dixit VM (1998) Death receptors: signaling and modulation. Science 281:1305–1308
Bassing CH, Chua KF, Sekiguchi J, Suh H, Whitlow SR, Fleming JC, Monroe BC, Ciccone DN, Yan C, Vlasakova K, Livingston DM, Ferguson DO, Scully R, Alt FW (2002) Increased ionizing radiation sensitivity and genomic instability in the absence of histone H2AX. Proc Natl Acad Sci U S A 99(12):8173–8178
Boose G, Stopper H (2000) Genotoxicity of several clinically used topoisomerase II inhibitors. Toxicol Lett 116:7–16
Bursch W, Ellinger A, Kienzl H, Torok L, Pandey S, Sikorska M, Walker R, Hermann RS (1996) Active cell death induced by the anti-estrogens tamoxifen and ICI 164 384 in human mammary carcinoma cells (MCF-7) in culture: the role of autophagy. Carcinogenesis 17(8):1595–1607
Chinnaiyan AM, O’Rourke K, Tewari M, Dixit VM (1995) FADD, a novel death domain-containing protein, interacts with the death domain of Fas and initiates apoptosis. Cell 81(4):505–512
Corcoran GB, Fix L, Jones DP, Moslen MT, Nicotera P, Oberhammer FA, Buttyan R (1994) Apoptosis: molecular control point in toxicity. Toxicol Appl Pharmacol 128:169–181
Cunha KS, Reguly ML, Graf U, Helena H (2001) Taxanes: the genetic toxicity of paclitaxel and docetaxel in somatic cells of Drosophila melanogaster. Mutagenesis 16:79–84
Green DR, Reed JC (1998) Mitochondria and apoptosis. Science 281:1309–1312
Hu W, Kavanagh JJ (2003) Anticancer therapy targeting the apoptotic pathway. Lancet Oncol 4:721–729
Huang X, Okafuji M, Traganos F, Luther E, Holden E, Darzynkiewicz Z (2004) Assessment of histone H2AX phosphorylation induced by DNA topoisomerase I and II inhibitors topotecan and mitoxantrone and by the DNA cross-linking agent cisplatin. Cytometry 58A:99–110
Jaattela M (2002) Programmed cell death: many ways for cells to die decently. Ann Med 34:480–488
Kazi A, Hill R, Long TE, Kuhn DJ, Turos E, Dou QP (2004) Novel N-thiolated β-lactam antibiotics selectively induce apoptosis in human tumor and transformed, but not normal or nontransformed, cells. Biochem Pharmacol 67:365–374
Kerr JF, Wyllie AH, Currie AR (1972) Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer 26:239–257
Khan P, Abbas S, Petit B, Caffrey R, Megram V, McGown A (1999) Development and validation of a high-performance liquid chromatographic assay using solid-phase extraction for the novel antitumor agent pancratistatin in human plasma. J Chromatogr B Biomed Sci Appl 726(1–2):249–254
Kim S, Ko H, Kim E, Kim D (2002) Stereocontrolled total synthesis of pancratistatin. Org Lett 4(8):1343–1345
Luduena RF, Roach MC, Prasad V, Pettit GR (1992) Biochem Pharmacol 43:539
Martin NMB (2001) DNA repair inhibition and cancer therapy. J Photochem Photobiol B 63:162–170
McNulty J, Mao J, Gibe R, Mo R, Wolf S, Pettit GR, Herald DL, Boyd MR (2001) Studies directed towards the refinement of the pancratistatin cytotoxic pharmacophore. Bioorg Med Chem Lett 11:169–172
Naderi J, Hung M, Pandey S (2003) Oxidative stress-induced apoptosis in dividing fibroblasts involves activation of p38 MAP kinase and over-expression of Bax: resistance of quiescent cells to oxidative stress. Apoptosis 8:91–100
Pettit GR, Pettit GR III, Backhaus RA, Boyd MR, Meerow AW (1993) Antineoplastic agents 256. Cell growth inhibitory isocarbostyrils from Hymenocallis. J Nat Prod 56:1682
Rothkamm K, Löbrich M (2003) Evidence for a lack of DNA double-strand break repair in human cells exposed to very low X-ray doses. Proc Natl Acad Sci U S A 100(9):5057–5062
Siraki AG, Pourahmad J, Chan TS, Khon S, O’Brien PJ (2002) Endogenous and endobiotic reactive oxygen species formation by isolated hepatocytes. Free Radic Biol Med 32:2–10
Souza-Fagundes EM, Brumatti G, Martins-Filho OA, Correa-Oliveira R, Zani CL, Amarante-Mendes GP (2003) Myriadenolide, a labdane diterpene isolated from Alomia myriadenia (asteraceae) induces depolarization of mitochondrial membranes and apoptosis associated with activation of caspases-8, -9 and -3 in Jurkat and THP-1 cells. Exp Cell Res 290:420–426
Acknowledgements
The authors are grateful to the volunteers for donation of normal blood cells. We gratefully acknowledge Miss Sarah McCarthy for assistance in H2AX immunostaining and Dr. Panyotis Vacratsis for critical review of the paper. This work was supported by infrastructure grants from the Canadian Foundation for Innovation (CFI) and Ontario Innovation Trust (OIT) to S.P. and an operating grant from the Natural Sciences and Engineering Research Council (NSERC) to S.P. and J.M.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kekre, N., Griffin, C., McNulty, J. et al. Pancratistatin causes early activation of caspase-3 and the flipping of phosphatidyl serine followed by rapid apoptosis specifically in human lymphoma cells. Cancer Chemother Pharmacol 56, 29–38 (2005). https://doi.org/10.1007/s00280-004-0941-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-004-0941-8