Abstract
Venetoclax, a selective B cell leukemia/lymphoma-2 (BCL2) inhibitor, has recently shown activity in relapsed or refractory (R/R) acute myeloid leukemia (AML). Effective biomarkers for identifying patients most likely to respond to venetoclax-based treatment are of clinical utility. In this study, we aimed to evaluate the efficacy and safety profiles of venetoclax-based therapy in a total 40 R/R AML patients and identify the potentially predictive factors for response. Overall response rate was 50%, including 9 (22.5%) complete response (CR) or CR with incomplete hematologic recovery of either neutrophil or platelet counts (CRi). Median time to best response was 1.4 months and the median overall survival (OS) was 6.6 months. Presence of intermediate-risk cytogenetics predicted better OS compared to unfavorable-risk cytogenetics. Patients harboring NPM1, RUNX1, or SRSF2 mutations seemed to have higher CR/CRi rates and median OS was significantly longer in RUNX1-mutated patients. On the contrary, patients with FLT3-ITD, TP53, or DNMT3A mutations did not reach any objective response and had worse OS. No laboratory or clinical tumor lysis syndrome was observed and the most common adverse events were prolonged cytopenias which resulted in 67.5% of febrile neutropenia. Patients with concurrent use of azole antifungals had similar incidence of cytopenias compared with those without azole antifungals. In summary, we demonstrate that venetoclax is an effective and well-tolerated salvage option for R/R AML patients. Survival benefits were particularly remarkable in patients with intermediate-risk cytogenetics or RUNX1 mutations. In contrast, TP53, NRAS, and DNMT3A mutations as well as FLT3-ITD conferred negative impact on survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) represents a clinically and biologically heterogeneous malignancy and relapsed or refractory (R/R) AML remains the most challenging issue in clinical practice [1, 2]. The outcome for patients with R/R AML is usually dismal with a median survival of only 3–6 months [3]. There is no standard salvage therapy for R/R AML, which indicates that there is still unmet medical needs [4, 5]. Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment in the R/R setting [6]; however, only a minor proportion of this group is able to proceed to allogeneic HSCT because of failure to achieve optimal response that is prerequisite for a successful transplantation, highlighting the urgent need for novel treatment to improve the response rate.
In recent years, better delineation of molecular landscape in AML has paved the way for drug development and lead to advancement of new strategies to treat AML. The B cell leukemia/lymphoma-2 (BCL-2), an anti-apoptotic protein, has been shown to suppress mitochondrial-modulated programmed cell death and support cell survival [7, 8]. It is aberrantly overexpressed in AML cells, specifically in leukemic stem cells [9]. Enhanced BCL-2 expression mediates chemo-resistance and survival benefits in leukemic blasts [10, 11].
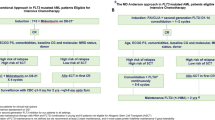
Venetoclax is a highly selective and potent oral BCL-2 inhibitor, which has shown activity in chronic lymphocytic leukemia (especially that with 17p deletion) [12,13,14] and multiple myeloma with t(11;14) [15]. The first phase II trial of venetoclax monotherapy for heavily pretreated R/R AML (n = 30) or unfit for intensive chemotherapy (n = 2) showed clinical activity with objective response rate of 19%, including 6% complete remission (CR) and 13% CR with incomplete hematologic recovery of either neutrophil or platelet counts (CRi) [16]. Subsequently, venetoclax in combination with low-dose cytarabine (LDAC) or hypomethylating agents (HMAs) in frontline setting showed rapid and durable response in a substantial portion (54–67%) of unfit elder patients [17, 18]. Till now, the activity of venetoclax-based regimen in R/R AML is not fully studied. There are few reports regarding venetoclax alone or in combination with other agents in the treatment of R/R AML and related myeloid malignancies [16, 19,20,21]. Recently, DiNardo et al. and Aldoss et al. demonstrated that venetoclax combination could be an effective salvage option in R/R AML setting. However, the treatment regimens, patient population and clinical response varied in these studies. More investigations are warranted in this regard. Furthermore, no consistent parameters predicting clinical response to venetoclax-based therapy have been identified. In this study, we aimed to evaluate the efficacy and safety profiles of venetoclax-based therapy in R/R AML patients and assess clinical, laboratory and molecular markers that could identify patients mostly likely to benefit from it.
Patients and methods
A total of 40 adult patients who were diagnosed as having R/R AML and received venetoclax-based therapy outside of clinical trials were recruited retrospectively into this study. Patients who received venetoclax < 14 days or had follow-up duration < 3 weeks were excluded. The cycle 1 venetoclax “ramp-up” schedules were designated according to the recommendation [17]. This study was approved by the National Taiwan University Hospital Institutional Review Board, in accordance with the Declaration of Helsinki. Patient characteristics were reported by median (range) values for continuous variables and frequency (percentage) for categorical variables. Statistical differences between groups were determined with using a Student’s t test for continuous data and Chi-square or Fisher’s exact test for nominal data. Mutational analyses of FLT3-ITD, CEBPA, NPM1, and RUNX1 genes were done as previously reported in all patients [22]. Molecular testing of 54 genes was also performed in 38 (95%) patients, 14 at initial diagnosis and 24, before venetoclax treatment, by targeted next-generation sequencing (NGS) using TruSight Myeloid Panel (Illumina, San Diego, CA, USA) [23]. Responses were evaluated by modified International Working Group (IWG) criteria for AML [24]. Time-to-event endpoints were evaluated by the Kaplan-Meier method, with differences between groups determined by log-rank test. All statistical analyses were conducted with Excel® 2016 for Windows and SPSS® Statistics version 20. A two-tailed value of P < 0.05 was considered as statistically significant.
Results
Patient characteristics
A total of 40 patients with R/R AML who underwent salvage therapy with venetoclax-based regimen were consecutively included in this retrospective observational study. At the time of analysis, patients received a median of 2 cycles of treatment (range, 1–8) and the median treatment duration was 2.2 months (range, 0.5–12.2). Patient demographics and disease characteristics of this heavily pretreated cohort are shown in Table 1. The median age was 63 years (range 20–88 years) and 42.5% of them were more than 65 years old. Twenty-five (62.5%) of the patients had de novo AML, 13 (32.5%) patients had secondary AML transformed from myelodysplastic syndrome (MDS) or myeloproliferative neoplasm (MPN) and two (5%), therapy-related AML. Median prior treatment lines were 3 (range, 1–9), and 6 (15%) patients received the treatment as first salvage setting. Thirteen (32.5%) patients had received allogeneic HSCT prior to venetoclax-based treatment. Chromosome data were available in 37 patients at enrollment; 25 (67.6%) patients had intermediate-risk cytogenetics and 11 (29.7%), unfavorable-risk cytogenetics based on the MRC classification [25]. According to the 2017 ELN recommendation [2], 12.5% of patients were in the favorable-risk group; 17.5%, the intermediate-risk group; and 70%, the unfavorable-risk group.
The median number of gene mutations was 2 (range 0–5) (Fig. 1). The most prevalent gene mutation was RUNX1 (n = 11, 27.5%), followed by ASXL1 (n = 9, 23.7%) and SRSF2 mutations (n = 5, 13.2%). Of note, only three (7.5%) patients had FLT3-ITD, three had NPM1 mutations and four (10.5%) had IDH2 mutations. Additional mutations and their frequencies are summarized in Supplementary Fig. 1.
Treatment characteristics and outcome
Eight (20%) patients received venetoclax as monotherapy and 32 received combination regimens, in whom 21 (52.5%) received azacitidine, 10 (25%) low-dose cytarabine (LDAC) and one (2.5%) fludarabine, cytarabine, and granulocyte colony-stimulating factor (FLAG). Twenty-five (62.5%) patients received venetoclax and azole antifungals concurrently, in whom venetoclax dose adjustment is strongly recommended due to CYP3A4 inhibition caused by azole antifungals. Among them, venetoclax was administered at a median dose of 100 mg (100–200 mg) in combination with posaconazole (n = 9, 36%) or voriconazole (n = 13, 52%) and 400 mg (100–600 mg) in combination with fluconazole (n = 3, 12%). In total cohort, the median dose of venetoclax was 150 mg (range, 100–600 mg).
With a median follow-up duration of 6.9 months (range, 0.7–16.3 months), the overall response rate (ORR) by IWG criteria was achieved in 20 (50%) patients, including 5 (12.5%) CR, 4 (10%) CRi, 5 (12.5%) morphologic leukemia-free state (MLFS) and 6 (15%) partial response (PR). All patients who achieved CR/CRi became transfusion independent. Six responding patients (30%) were bridged to allogeneic HSCT (Table 2). Among the patients obtaining CR/CRi, five (55.6%) patients also reached minimal residual disease negativity as shown by flow cytometry. Twenty patients with at least PR had received a median of 3 (range, 1–9) prior lines of therapy and all these patients responded within 1 cycle of venetoclax therapy (Table 2). The median time to first response was 0.95 month (range, 0.5–2.5) and the median time to best response was 1.4 month (range, 0.5–5.5). Seventeen (85%) of the 20 responsive patients received venetoclax combination therapy, including 10 (50%) with azacitidine, six (30%) LDAC and one (5%) FLAG. Eighteen (75%) of the 24 patients without prior HMA exposure were treated with azacitidine and venetoclax, and ten (55.6%) of them achieved clinical response; in contrast, three (18.8%) of the 16 patients with previous exposure to HMA [azacitidine (n = 15) or SGI-110 (n = 1)] received azacitidine combination therapy and none obtained clinical response.
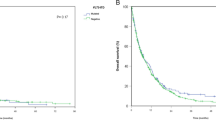
Seventeen (68%) of 25 patients with intermediate-risk cytogenetics achieved an objective response; in contrast, three (27.3%) of 11 patients with unfavorable-risk cytogenetics did so (P = 0.034). However, we could not find statistical difference in ORR or CR/CRi between patients with primary and secondary/therapy-related AML, ELN intermediate- and unfavorable-risk groups, and those with prior HMA treatment/HSCT and without. The median overall survival (OS) was 6.6 months (range, 0.7–16.3) and survival rate in 6 months was 58.2% (Fig. 2a). The median OS was not reached in patients obtaining CR/CRi compared with remaining patients without (P = 0.014, Fig. 2b). Four (44.4%) of nine patients achieving CR/CRi were bridged to allogeneic HSCT and all remained disease free and alive through the study period. There was statistically significant difference of OS among different cytogenetic groups (P = 0.037, Fig. 2c). A trend of better OS could be found in patients receiving venetoclax in combination with HMA than those with LDAC (median 7.4 months vs. 5.8 months, P = 0.155).
Prognostic relevance of gene mutations in venetoclax-based therapy
Among the 40 R/R AML patients, ORR was 100% for patients with FLT3-TKD (n = 2), SRSF2 (n = 5), NPM1 (n = 3), or U2AF1 (n = 2) mutations, 77.8% for those with ASXL1 mutations (n = 9), 75% for those with IDH2 (n = 4), or STAG2 mutations (n = 4) as well as 54.5% for those with RUNX1 mutations (n = 9, Table 2). Of note, patients with mutations in NPM1 (66.8%), SRSF2 (40%), and RUNX1 (36.4%) had higher than average CR/CRi rates if we considered only those genes detected in three or more patients.
Among the 11 patients harboring RUNX1 mutations, six (54.5%) reached ORR, including 2 CR, 2 CRi, and 2 PR. Intriguingly, RUNX1-mutated patients had better OS than RUNX1-wild patients (P = 0.014, Fig. 3a). All five SRSF2-mutated patients, all harboring ASXL1 mutations concurrently, responded to venetoclax-based therapy, including one CR (20%), one CRi (20%), and three PR (60%) (Table 2). Of the four patients harboring IDH2 mutations, one reached CR and then proceeded to allogeneic HSCT smoothly, two obtained PR, and the remaining one received allogeneic HSCT after achieving blast reduction in peripheral blood, but disease relapsed rapidly 2 months later. On the contrary, all patients harboring TP53 mutations (n = 4), DNMT3A mutations (n = 3), or FLT3-ITD (n = 3) did not have objective response to venetoclax-based therapy. All three patients with FLT3-ITD received FLT3 inhibitors, including two of midostaurin and one of sorafenib prior to venetoclax-based regimen. The poor response also translated into significantly worse OS (Fig. 3b–d). Besides, presence of NRAS or SETBP1 mutations predicted shorter OS (Fig. 3e–f). Mutations in other genes showed no implication on survival.
Safety profiles
Tumor lysis syndrome (TLS) prophylaxis with febuxostat 40 mg/day and hydration was universally administered at least on the day of initiation of venetoclax and till the risks of TLS diminished [26]. All patients had a white blood cell (WBC) count less than 25 ×109/L before venetoclax treatment and no patients developed laboratory or clinical TLS.
The majority of patients had an ECOG performance status of 2. The 30-day early mortality was 7.5% and 6 (15%) deaths occurred at ≤ 60 days. Prior to treatment initiation, 55% of patients (n = 22) had grade 4 neutropenia and 70% (n = 28) had grade ≥ 3 thrombocytopenia due to uncontrolled hematologic diseases. Twenty (50%) patients had documented infections prior treatment initiation, including 12 (60%) of invasive fungal infection and 3 (15%) of Mycobacterium infection. Irrespective of causes, 16 (40%) patients had persistent grade 4 neutropenia and 23 (57.5%) patients had persistent grade ≥ 3 thrombocytopenia through the study period (Table 3). The median time of neutrophil or platelet count recovery was 40 days (range, 6–90) and 31 days (range, 6–67), respectively. During treatment, neutropenic fever was reported in 27 (67.5%) of patients and 18 (45%) patients developed documented infections, including blood stream infections due to gram negative (n = 7, 38.9%) or gram positive (n = 3, 16.7%) bacteria, Candida tropicalis fungemia (n = 1, 5.6%), Mycobacterium kansasii (n = 1, 5.6%), and invasive fungal infection (n = 2, 11.1%). This resulted in 5 (25%) deaths caused by infection in patients achieving ORR. Nine (22.5%) patients received G-CSF support at any time during venetoclax treatment.
Thirteen (50%) of 26 patients who had grade III or more hematologic adverse events (AEs) had venetoclax dose interruption. Reduced duration of venetoclax administration occurred in six patients with three patients to 21 days and 3 to 14 days. Five patients had a delay of cycle treatment to allow for hemogram recovery. Overall, treatment was discontinued in 32 (80%) patients, with no response or progressive disease (n = 16, 50%) being the most common reason; others included bridging to allogeneic HSCT (n = 9, 28.1%), grade 4 neutropenia or thrombocytopenia (n = 4, 12.5%), and grade 4 infection (n = 3, 9.4%).
Twelve (48%) of the 25 patients with azole antifungals administration concomitantly had persistent neutropenia, and 17 (68%) had persistent thrombocytopenia. However, there was no statistically significant difference in incidence of persistent neutropenia or thrombocytopenia between patients taking azole antifungals and those without (P = 0.143 and P = 0.168, respectively).
Discussion
We reported a real-world experience of venetoclax-based therapy in a relatively larger cohort of patients with R/R AML. There have been limited reports regarding the response of venetoclax-based therapy in R/R AML. The ORR reported in these studies varied from 11.6 to 51.5% (Table 4) probably due to different patient cohorts, mutation patterns, and treatment modalities (either monotherapy or combination therapy). In this study, we showed that the ORR was 50% and nine (22.5%) patients could reach CR or CRi among the heavily pretreated and high-risk patients who had a median prior treatment lines of 3, ELN adverse-risk group of 70%, and prior allogeneic HSCT in around one-third patients. Importantly, we identified cytogenetic and molecular markers that might help stratify R/R AML patients into groups with different response rates and OS.
The median OS was 6.6 months in total cohort and not reached in patients achieving CR/CRi, longer than those reported by Konopleva et al. [17, 18] and DiNardo et al. [17, 18] (Table 4). This was possibly because ten (25%) patients were bridged to allogeneic HSCT smoothly in this study, compared to only one patient in the study of Konopleva et al. [17, 18] and two, in the study of DiNardo et al. [17, 18]. These findings are consistent with the concept that allogeneic HSCT is the only potentially curative treatment in R/R AML patients if they can achieve optimal response before transplantation.
All the response to venetoclax-based therapy was observed within 1 cycle, and patients reaching CR/CRi had significantly better survival, compared to others without CR/CRi, which were consistent with previous findings [16, 19, 20]. In contrast to HMA treatment alone, in which optimal response can be obtained only after a sufficient number of cycles [27, 28], a CR/CRi can be achieved with venetoclax-based therapy within 1–2 cycles.
Given the limited number of patients reported in literature, the markers that can predict response to venetoclax-based therapy remain unclear. More studies are warranted to identify predictors of clinical benefits. In this study, high-risk cytogenetics had negative impact on outcomes as previously described [19]. Nevertheless, the findings regarding prognostic impact of molecular mutations on response to venetoclax-based therapy in R/R AML were not consistent. This study was aimed to comprehensively investigate the mutation pattern and its prognostic relevance in R/R AML patients receiving venetoclax-based therapy. Consistent with previous studies [16,17,18,19,20], patients with NPM1 or IDH mutations appeared to have promising response to venetoclax-based therapy. In a previous report of DiNardo et al., RUNX1-mutated R/R AML patients were shown for the first time to have higher ORR to venetoclax-based treatment, in whom 50% (4/8) achieved an objective response, compared with 21% in total cohort; however, no survival impact was reported [20]. Similarly, in the current study, six (54.5%) of 11 RUNX1-mutated patients obtained an objective response, including 4 CR/CRi and 2 PR. Furthermore, we identified that RUNX1 mutation was a significantly favorable prognostic factor for OS, suggesting that venetoclax-based therapy may be able to overcome the poor prognosis of RUNX1 mutation besides allogeneic HSCT [29,30,31]. Other interesting findings were that all SRSF2-mutated patients had an objective response to venetoclax-based therapy and these patients had ASXL1 mutations concurrently. These findings might partially explain why there was no significantly survival difference among different ELN risk groups since venetoclax-based therapy improved outcome of patients with adverse-risk genotypes, such as RUNX1 and ASXL1 mutations. It merits further studies for not only validation in a larger molecularly-based cohort but also exploration of the underlying mechanism. On the other hand, we showed for the first time that FLT3-ITD, TP53, and DNMT3A mutations were significantly unfavorable predictors for ORR, and mutations in TP53, DNMT3A, NRAS, and SETBP1 and FLT3-ITD conferred shorter OS in R/R AML patients treated with venetoclax-based therapy. The median OS was less than 4 months in patients with these mutations.
Regarding the safety profiles of venetoclax-based therapy in R/R AML, the most commonly observed complications were related to prolonged cytopenias. Prior to treatment initiation, the majority of patients presented with grade ≥ 3 cytopenias due to the nature of underlying diseases and over 50% patients remained prolonged and profound cytopenias through the study period, which often led to grade ≥ 3 infections, including bacteremia or invasive fungal infections. Despite of the high incidence of severe infection, with adequate treatment, the 30-day mortality rate was only 7.5%, slightly lower than the previous report (12%) [20]. There was no laboratory or clinical TLS observed through the study period while all patients were under febuxostat and hydration prophylaxis [16, 20]. Over 50% patients had azole antifungal administration concomitantly with venetoclax, and the dose of venetoclax was adjusted accordingly as previously recommended [32]. There was no significant difference in incidence of cytopenias between patients having concurrent antifungals or not, suggesting that venetoclax with dose adjustment for drug interactions with antifungals was well tolerated in R/R AML settings.
This study has several limitations. First, due to the retrospective nature of this study, many factors could not be exactly assessed as in a perspective clinical trial, such as timing of bone marrow study and sampling of mutations by NGS. However, a complete mutational screen of 54 genes were performed in 95% of patients and 63.2% of them was done before venetoclax treatment. We clearly demonstrated that mutations could predict treatment outcome in R/R AML patients. Second, relatively short duration of follow-up precludes the assessment of long-term efficacy and safety of venetoclax-based therapy. Further large-scale prospective trials are warranted to validate these findings.
In summary, the present study provides experience of venetoclax-based therapy in a relatively larger R/R AML cohort, demonstrating an efficient and well-tolerated salvage option for this poor-risk population. Treatment benefits were particularly notable in patients with intermediate-risk cytogenetics, NPM1, IDH2, or RUNX1 mutations. In contrast, TP53, NRAS, DNMT3A, and SETBP1 mutations as well as FLT3-ITD conferred negative impact on survival.
References
Dohner H, Weisdorf DJ, Bloomfield CD (2015) Acute Myeloid Leukemia. N Engl J Med 373(12):1136–1152. https://doi.org/10.1056/NEJMra1406184
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Lowenberg B, Bloomfield CD (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129(4):424–447. https://doi.org/10.1182/blood-2016-08-733196
Shah A, Andersson TM, Rachet B, Bjorkholm M, Lambert PC (2013) Survival and cure of acute myeloid leukaemia in England, 1971-2006: a population-based study. Br J Haematol 162(4):509–516. https://doi.org/10.1111/bjh.12425
Thol F, Schlenk RF, Heuser M, Ganser A (2015) How I treat refractory and early relapsed acute myeloid leukemia. Blood 126(3):319–327. https://doi.org/10.1182/blood-2014-10-551911
Dombret H, Gardin C (2016) An update of current treatments for adult acute myeloid leukemia. Blood 127(1):53–61. https://doi.org/10.1182/blood-2015-08-604520
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, Kamble R, Copelan E, de Lima M, Gupta V, Keating A, Lazarus HM, Litzow MR, Marks DI, Maziarz RT, Rizzieri DA, Schiller G, Schultz KR, Tallman MS, Weisdorf D (2010) Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol 28(23):3730–3738. https://doi.org/10.1200/JCO.2010.28.8852
Certo M, Del Gaizo MV, Nishino M, Wei G, Korsmeyer S, Armstrong SA, Letai A (2006) Mitochondria primed by death signals determine cellular addiction to antiapoptotic BCL-2 family members. Cancer Cell 9(5):351–365. https://doi.org/10.1016/j.ccr.2006.03.027
Chao DT, Korsmeyer SJ (1998) BCL-2 family: regulators of cell death. Annu Rev Immunol 16:395–419. https://doi.org/10.1146/annurev.immunol.16.1.395
Campos L, Rouault JP, Sabido O, Oriol P, Roubi N, Vasselon C, Archimbaud E, Magaud JP, Guyotat D (1993) High expression of bcl-2 protein in acute myeloid leukemia cells is associated with poor response to chemotherapy. Blood 81(11):3091–3096
Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ, Minhajuddin M, Ashton JM, Pei S, Grose V, O'Dwyer KM, Liesveld JL, Brookes PS, Becker MW, Jordan CT (2013) BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell 12(3):329–341. https://doi.org/10.1016/j.stem.2012.12.013
Konopleva M, Zhao S, Hu W, Jiang S, Snell V, Weidner D, Jackson CE, Zhang X, Champlin R, Estey E, Reed JC, Andreeff M (2002) The anti-apoptotic genes Bcl-X(L) and Bcl-2 are over-expressed and contribute to chemoresistance of non-proliferating leukaemic CD34+ cells. Br J Haematol 118(2):521–534. https://doi.org/10.1046/j.1365-2141.2002.03637.x
Roberts AW, Davids MS, Pagel JM, Kahl BS, Puvvada SD, Gerecitano JF, Kipps TJ, Anderson MA, Brown JR, Gressick L, Wong S, Dunbar M, Zhu M, Desai MB, Cerri E, Heitner Enschede S, Humerickhouse RA, Wierda WG, Seymour JF (2016) Targeting BCL2 with Venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med 374(4):311–322. https://doi.org/10.1056/NEJMoa1513257
Seymour JF, Kipps TJ, Eichhorst B, Hillmen P, D'Rozario J, Assouline S, Owen C, Gerecitano J, Robak T, De la Serna J, Jaeger U, Cartron G, Montillo M, Humerickhouse R, Punnoose EA, Li Y, Boyer M, Humphrey K, Mobasher M, Kater AP (2018) Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med 378(12):1107–1120. https://doi.org/10.1056/NEJMoa1713976
Stilgenbauer S, Eichhorst B, Schetelig J, Coutre S, Seymour JF, Munir T, Puvvada SD, Wendtner CM, Roberts AW, Jurczak W, Mulligan SP, Bottcher S, Mobasher M, Zhu M, Desai M, Chyla B, Verdugo M, Enschede SH, Cerri E, Humerickhouse R, Gordon G, Hallek M, Wierda WG (2016) Venetoclax in relapsed or refractory chronic lymphocytic leukaemia with 17p deletion: a multicentre, open-label, phase 2 study. Lancet Oncol 17(6):768–778. https://doi.org/10.1016/S1470-2045(16)30019-5
Kumar S, Kaufman JL, Gasparetto C, Mikhael J, Vij R, Pegourie B, Benboubker L, Facon T, Amiot M, Moreau P, Punnoose EA, Alzate S, Dunbar M, Xu T, Agarwal SK, Enschede SH, Leverson JD, Ross JA, Maciag PC, Verdugo M, Touzeau C (2017) Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood 130(22):2401–2409. https://doi.org/10.1182/blood-2017-06-788786
Konopleva M, Pollyea DA, Potluri J, Chyla B, Hogdal L, Busman T, McKeegan E, Salem AH, Zhu M, Ricker JL, Blum W, DiNardo CD, Kadia T, Dunbar M, Kirby R, Falotico N, Leverson J, Humerickhouse R, Mabry M, Stone R, Kantarjian H, Letai A (2016) Efficacy and biological correlates of response in a phase II study of Venetoclax Monotherapy in patients with acute Myelogenous leukemia. Cancer Discov 6(10):1106–1117. https://doi.org/10.1158/2159-8290.CD-16-0313
DiNardo CD, Pratz K, Pullarkat V, Jonas BA, Arellano M, Becker PS, Frankfurt O, Konopleva M, Wei AH, Kantarjian HM, Xu T, Hong WJ, Chyla B, Potluri J, Pollyea DA, Letai A (2019) Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 133(1):7–17. https://doi.org/10.1182/blood-2018-08-868752
Wei AH, Strickland SA Jr, Hou JZ, Fiedler W, Lin TL, Walter RB, Enjeti A, Tiong IS, Savona M, Lee S, Chyla B, Popovic R, Salem AH, Agarwal S, Xu T, Fakouhi KM, Humerickhouse R, Hong WJ, Hayslip J, Roboz GJ (2019) Venetoclax combined with low-dose Cytarabine for previously untreated patients with acute myeloid leukemia: results from a phase Ib/II study. J Clin Oncol 37(15):1277–1284. https://doi.org/10.1200/JCO.18.01600
Aldoss I, Yang D, Aribi A, Ali H, Sandhu K, Al Malki MM, Mei M, Salhotra A, Khaled S, Nakamura R, Snyder D, O'Donnell M, Stein AS, Forman SJ, Marcucci G, Pullarkat V (2018) Efficacy of the combination of venetoclax and hypomethylating agents in relapsed/refractory acute myeloid leukemia. Haematologica 103(9):e404–e407. https://doi.org/10.3324/haematol.2018.188094
DiNardo CD, Rausch CR, Benton C, Kadia T, Jain N, Pemmaraju N, Daver N, Covert W, Marx KR, Mace M, Jabbour E, Cortes J, Garcia-Manero G, Ravandi F, Bhalla KN, Kantarjian H, Konopleva M (2018) Clinical experience with the BCL2-inhibitor venetoclax in combination therapy for relapsed and refractory acute myeloid leukemia and related myeloid malignancies. Am J Hematol 93(3):401–407. https://doi.org/10.1002/ajh.25000
Ram R, Amit O, Zuckerman T, Gurion R, Raanani P, Bar-On Y, Avivi I, Wolach O (2019) Venetoclax in patients with acute myeloid leukemia refractory to hypomethylating agents-a multicenter historical prospective study. Ann Hematol 98(8):1927–1932. https://doi.org/10.1007/s00277-019-03719-6
Hou HA, Lin CC, Chou WC, Liu CY, Chen CY, Tang JL, Lai YJ, Tseng MH, Huang CF, Chiang YC, Lee FY, Kuo YY, Lee MC, Liu MC, Liu CW, Lin LI, Yao M, Huang SY, Ko BS, Hsu SC, Wu SJ, Tsay W, Chen YC, Tien HF (2014) Integration of cytogenetic and molecular alterations in risk stratification of 318 patients with de novo non-M3 acute myeloid leukemia. Leukemia 28(1):50–58. https://doi.org/10.1038/leu.2013.236
Tien FM, Hou HA, Tsai CH, Tang JL, Chiu YC, Chen CY, Kuo YY, Tseng MH, Peng YL, Liu MC, Liu CW, Liao XW, Lin LI, Lin CT, Wu SJ, Ko BS, Hsu SC, Huang SY, Yao M, Chou WC, Tien HF (2018) GATA2 zinc finger 1 mutations are associated with distinct clinico-biological features and outcomes different from GATA2 zinc finger 2 mutations in adult acute myeloid leukemia. Blood Cancer J 8(9):87. https://doi.org/10.1038/s41408-018-0123-2
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, Schiffer CA, Doehner H, Tallman MS, Lister TA, Lo-Coco F, Willemze R, Biondi A, Hiddemann W, Larson RA, Lowenberg B, Sanz MA, Head DR, Ohno R, Bloomfield CD, International Working Group for Diagnosis SoRCTO, Reporting Standards for Therapeutic Trials in Acute Myeloid L (2003) Revised recommendations of the international working Group for Diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol 21(24):4642–4649. https://doi.org/10.1200/JCO.2003.04.036
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A (1998) The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council adult and Children's Leukaemia working parties. Blood 92(7):2322–2333
Coiffier B, Altman A, Pui CH, Younes A, Cairo MS (2008) Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review. J Clin Oncol 26(16):2767–2778. https://doi.org/10.1200/JCO.2007.15.0177
Andriani A, Montanaro M, Voso MT, Villiva N, Ciccone F, Andrizzi C, De Gregoris C, Di Veroli A, Maurillo L, Alimena G, Latagliata R (2015) Azacytidine for the treatment of retrospective analysis from the Gruppo Laziale for the study of Ph-negative MPN. Leuk Res 39(8):801–804. https://doi.org/10.1016/j.leukres.2015.03.001
Ivanoff S, Gruson B, Chantepie SP, Lemasle E, Merlusca L, Harrivel V, Charbonnier A, Votte P, Royer B, Marolleau JP (2013) 5-Azacytidine treatment for relapsed or refractory acute myeloid leukemia after intensive chemotherapy. Am J Hematol 88(7):601–605. https://doi.org/10.1002/ajh.23464
Chou SC, Tang JL, Hou HA, Chou WC, Hu FC, Chen CY, Yao M, Ko BS, Huang SY, Tsay W, Chen YC, Tien HF (2014) Prognostic implication of gene mutations on overall survival in the adult acute myeloid leukemia patients receiving or not receiving allogeneic hematopoietic stem cell transplantations. Leuk Res 38(11):1278–1284. https://doi.org/10.1016/j.leukres.2014.08.012
Tang JL, Hou HA, Chen CY, Liu CY, Chou WC, Tseng MH, Huang CF, Lee FY, Liu MC, Yao M, Huang SY, Ko BS, Hsu SC, Wu SJ, Tsay W, Chen YC, Lin LI, Tien HF (2009) AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: prognostic implication and interaction with other gene alterations. Blood 114(26):5352–5361. https://doi.org/10.1182/blood-2009-05-223784
Gaidzik VI, Bullinger L, Schlenk RF, Zimmermann AS, Rock J, Paschka P, Corbacioglu A, Krauter J, Schlegelberger B, Ganser A, Spath D, Kundgen A, Schmidt-Wolf IG, Gotze K, Nachbaur D, Pfreundschuh M, Horst HA, Dohner H, Dohner K (2011) RUNX1 mutations in acute myeloid leukemia: results from a comprehensive genetic and clinical analysis from the AML study group. J Clin Oncol 29(10):1364–1372. https://doi.org/10.1200/JCO.2010.30.7926
Agarwal SK, DiNardo CD, Potluri J, Dunbar M, Kantarjian HM, Humerickhouse RA, Wong SL, Menon RM, Konopleva MY, Salem AH (2017) Management of Venetoclax-Posaconazole Interaction in acute myeloid leukemia patients: evaluation of dose adjustments. Clin Ther 39(2):359–367. https://doi.org/10.1016/j.clinthera.2017.01.003
Acknowledgments
We would like to acknowledge the service provided by the DNA Sequencing Core of the First Core Laboratory, National Taiwan University College of Medicine.
Funding
This study was funded by MOST 104-2314-B-002-128-MY4 and 106-2314-B-002-226-MY3 from the Ministry of Science and Technology (Taiwan) and MOHW 107-TDU-B-211-114009 from the Ministry of Health and Welfare (Taiwan).
Author information
Authors and Affiliations
Contributions
Y.-W.W. was responsible for data management and interpretation, statistical analysis, and manuscript writing; C.-H.T. and F.-M.T. were responsible for mutation analysis and interpretation; C.-C.L., Y.-W.C., H-Y.L., M.Y., Y.-C.L., C.-T.C., T.-C.L., J.-L.T., and W.-C.C. contributed patient samples and clinical data; H.-A.H. designed, planned, and coordinated the study over the entire period, analyzed and interpreted data, and wrote the manuscript. H.-F.T. planned and coordinated the study over the entire period and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Author Yu-Wen Wang declares that she has no conflict of interest. Author Cheng-Hong Tsai declares that he has no conflict of interest. Author Chien-Chin Lin declares that he has no conflict of interest. Author Yu-Wen Chen declares that she has no conflict of interest. Author Hsing-Yu Lin declares that she has no conflict of interest. Author Ming Yao declares that he has no conflict of interest. Author Yun-Chu Lin declares that she has no conflict of interest. Author Chien-Ting Lin declares that he has no conflict of interest. Author Chieh-Lung Cheng declares that he has no conflict of interest. Author Jih-Luh Tang declares that he has no conflict of interest. Author Wen-Chien Chou declares that he has no conflict of interest. Author Hsin-An Hou has received research grants from Celgene Corporation. Author Hwei-Feng Tien has received research grants from Celgene Corporation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 55 kb)
Rights and permissions
About this article
Cite this article
Wang, YW., Tsai, CH., Lin, CC. et al. Cytogenetics and mutations could predict outcome in relapsed and refractory acute myeloid leukemia patients receiving BCL-2 inhibitor venetoclax. Ann Hematol 99, 501–511 (2020). https://doi.org/10.1007/s00277-020-03911-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-03911-z