Abstract
The benefit of early admission of allogeneic stem cell transplantation (SCT) recipients to the intensive care unit (ICU) as soon as they develop organ injury is unknown. We performed a retrospective study on 92 patients admitted to the ICU to determine the impact of time from organ injury to ICU admission on outcome. The number of organ injuries prior to ICU admission was associated with an increased in-hospital mortality (OR 1.7, 95% CI 1–2.7, p = 0.04). Time between first organ injury and ICU admission was also associated with an increased in-hospital survival (OR 1.4, 95% CI 1.1–1.8, p = 0.02). A score combining these two covariates—the number of organ injuries/day (sum of days spent with each individual organ injury)—further improved the prediction of hospital survival. Patients with more organ injuries/day had significantly higher in-hospital mortality rate even after adjustment for refractory acute GVHD and the SOFA (OR 1.3, 95% CI 1–1.7, p = 0.02). Early ICU admission of allogeneic SCT recipients to the ICU as soon as they develop organ injury is associated with decreased in-hospital mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prognosis of patients with hematological malignancies admitted to the intensive care unit (ICU) has improved over the past years from nearly 90% hospital mortality in the early 90s to 50% in the most recent years [1]. A large prospective multi-centric study by Azoulay et al. recently showed that an in-hospital survival of 60.7% and a 1-year survival of 43.3% are now observed for patients with all types of hematologic malignancies admitted to the ICU [2]. Allogeneic stem cell transplantation (SCT) is the only curative treatment for many hematologic diseases. Even though complications associated with this procedure have decreased in the past years, organ failures still occur and admission to intensive care unit may be required in 9 to 20% of all allogeneic SCT recipients [3,4,5,6,7]. After admission to the ICU, in-hospital survival of these patients ranges from 25 to 32% with a 1-year survival of 15 to 22%, far lower than the general overall survival of 53% in allogeneic SCT recipients [3,4,5,6,7,8,9,10,11]. We recently showed that the number of organ support required was the most important prognostic factor for early (ICU and hospital) mortality after admission to the ICU. Acute graft-versus-host disease (GVHD) had an impact on in-hospital survival but not ICU survival and only when it was refractory to steroid therapy [12]. Despite some improvement, survival remains dismal in this setting and admission of these patients to the ICU is still controversial [1].
It has been advocated that patients with hematological malignancies might benefit from early ICU admission. Indeed, the introduction of an early warning system (EWS) and the early involvement of ICU teams in one institution enabled the admission of less injured patients and an improved survival despite more patients requiring mechanical ventilation (MV). This early admission policy mostly benefited SCT recipients [13]. This must be specifically confirmed in allogeneic SCT recipients for whom there is the most reluctance for ICU admission due to the perception that they have a dismal outcome. It must be determined if allogeneic SCT recipients should be admitted to the ICU as soon as they develop organ injury or if they should be admitted later on when they present with organ failure and require organ support. Despite a lack of evidence, some advocate that early admission to the ICU might improve survival [2].
We reanalyzed our previously published cohort with special interest on the number of organ injuries prior to ICU admission and on the timing between organ injury and ICU referral. These two parameters were significantly associated with in-hospital survival. We developed a score combining these two parameters—number of organ injuries/day—which further improved the prediction of in-hospital survival.
Patients and methods
Patients and setting
All patients included in our previous study who received allogeneic SCT between 2002 and 2013 in our center and were admitted to the ICU during this time period were included [12]. In case of multiple ICU admissions, only the first admission was considered. Our University Hospital includes a 15-bed intensive hematology ward with either laminar air-flow or filtered air rooms where graft procedures are performed and a 24-bed ICU. Our stem cell transplant ward is dedicated to carrying out graft procedures and managing organ injury resulting from these procedures. No organ support, including high flux oxygenation or dopamine, is performed in the ward. The decision to admit a patient in the ICU was decided by both the attending hematologist and the on-call intensivist when organ injury was thought to require organ support. Once in the ICU, a regular reappraisal of the patient’s situation was performed by hematologists and intensivists.
Data collection
Data regarding patients was extracted from the minimal essential data (MED-A form) submitted from our center to the EBMT (European Society for Blood and Marrow Transplantation) central registry and carefully checked. Details on patients, graft procedures, GVHD, ICU admission, and outcome were collected from individual medical records. We report organ injuries as any disturbance in organ function. To define these disturbances, we chose clinical definitions used in the Early Warning System (oxygen requirement, low blood-pressure, altered mental status) and biological definitions used in the KDIGO or the SOFA. Organ injuries were therefore defined as: the need for oxygen therapy defined respiratory injury, low blood pressure (systolic arterial pressure < 90 mmHg) defined hemodynamic injury, altered mental status defined neurological injury, elevated serum creatinine (≥ 1.5 times baseline or ≥ 0.3 mg/dL increase) defined renal injury, and total bilirubin (> 34 μmol/l) defined liver injury [13,14,15]. Each organ failure was defined as the requirement for organ support, and liver failure was defined as a total bilirubin level greater than 34 μmol/l which is the equivalent to a score of 2 out of 4 in the Sequential Organ Failure Assessment (SOFA). Our institution did not use dopamine or high flux oxygenation during the study period, either on the ward or in the ICU. The SOFA was calculated as previously described (Supplementary Table 1) [15].
Time from organ injury to ICU admission was defined as follows: < 1 day (less than 24 h from organ injury to ICU admission), 1 day (24 to 48 h after organ injury), and > 1 day (more than 48 h from organ injury to ICU admission). To integrate the number of organ injuries and time spent from first organ injury to ICU admission, we built a score incorporating both covariates: the number of organ injury/day. For example, a patient with respiratory injury for 2 days and hemodynamic injury for 1 day had 3 organ injuries/day. Also, a patient with renal injury for 3 days and altered mental status for 2 days had 5 organ injuries/day.
End points
In-hospital mortality was defined as death from any cause in the hospital before discharge. This included patients who died in the ICU or in a conventional care ward after being discharged alive from the ICU. Overall survival (OS) was defined as the time from stem cell reinjection to death or last follow-up.
Statistical analysis
Categorical variables were presented as numbers with proportions and compared using the Chi2 test or the Fisher’s exact test, according to the size number. Continuous variables were presented as medians with interquartile range (IQR) and compared using the non-parametric Mann and Whitney test. The impact of organ injuries prior to ICU admission on hospital mortality was explored by logistic regression analysis. A logistic regression model was used to adjust for potential confounding factors (severity of organ injury at the time of ICU admission as assessed by the SOFA and refractory acute GVHD). Results were all expressed as odds ratios (OR) with 95% confidence intervals (95% CI). The Kaplan-Meier method was used to estimate median OS, and survival curves were compared using the log-rank test. All tests were two-sided with a significant level p < 0.05. Statistical analysis was performed with SPSS software version 20 (SPSS Inc., Chicago, IL).
Results
Patient characteristics
Of 349 patients who underwent ASCT during the study period, 92 patients (26%) were admitted to the ICU. Median follow-up for all patients was 63 days (IQR: 15–270 days). Median time from transplantation to ICU admission was 53 days (IQR 15–253 days). Patient characteristics and data relative to graft procedure are summarized in Table 1. Median age was 52 (IQR 38–58). Most patients (82%) had controlled disease at the time of allogeneic SCT and received allogeneic SCT for acute leukemia (45%). Forty-two patients (46%) received reduced-intensity conditioning (RIC) and 25 patients (27%) received sequential treatment with chemotherapy and RIC. Donors of allogeneic procedures were mostly unrelated (59%) and graft source was mostly peripheral blood stem cells (78%). Thirty-eight patients (41%) were admitted to the ICU more than 100 days after allograft whereas 23 (25%) were admitted before engraftment, and 31 (34%) were admitted after engraftment but before day 100 after allograft. Thirty-eight patients (41%) admitted to the ICU presented with acute GVHD. Most patients had grade III–IV acute GVHD (30/38 patients, 33% of total), and 12/38 patients (13% of total) had refractory acute GVHD. Sixty-three patients (69%) had an infectious complication after ICU admission with 41 being of bacterial origin. Twelve patients (13%) were admitted less than 2 days in the ICU, five because of early death in the ICU.
Number of organ injuries prior to ICU admission
Patients presented with a median of one organ injury prior to ICU admission. Ten patients were transferred to the ICU with no organ injury mainly for observation following at-risk procedures (lobectomy, bronchoalveolar lavage) or to manage hydroelectrolytic disorders. A few patients (13%) had three or four organ injuries prior to ICU admission (Table 2). The number of organ injuries prior to ICU admission was associated with increased hospital mortality (OR 1.7, 95% CI 1–2.7, p = 0.04). There was a clear survival difference between patients with 0 to 2 organ injuries and those with three or four organ injuries (Supplementary Fig. 1A). This was confirmed after adjustment for refractory acute GVHD (OR 2, 95% CI 1.1–3.5, p = 0.02) but not for the SOFA (OR 1.3, 95% CI 0.7–2.4, p = 0.35). At the time of referral to the ICU, 12 patients had 3 or 4 organ injuries and only 1 of these patients (8%) could be discharged alive from the hospital versus 39/78 patients (50%) with 0 to 2 organ injuries (p = 0.01).
We considered patients with zero to two organ injuries as a single subgroup and compared them with patients with three or four organ injuries. Patients who presented with 3 or 4 organ injuries prior to ICU admission were older, were most likely to have AML or MPN rather than a lymphoproliferative disorder, had more comorbidities, and were more likely to have benefitted from allogeneic SCT later on during their disease course (Supplementary Table 2). They had a higher SOFA at admission to the ICU and they required more organ support (Supplementary Fig. 2A). Patients with more than two organ injuries had a median OS of 35 days versus 384 days for those with less than two organ injuries (Supplementary Fig. 3a).
Time between first organ injury and ICU admission
The median time between first organ injury and ICU admission was 1 day with 68% of patients admitted to the ICU in the day following the first organ injury (Table 2). Each day spent with one or more organ injury worsens hospital survival of patients once they were admitted to the ICU even after adjustment for both refractory acute GVHD and the SOFA at ICU admission (OR 1.4, 95% CI 1.1–1.8, p = 0.02). Patients who were admitted to the ICU more than 1 day following the first signs of organ injury were more likely to die in the hospital (20/28 patients, 71%) than those who were admitted on the day following the first organ injury (30/62 patients, 48%) (p = 0.03) (Supplementary Fig. 1B). Median time from hospital admission to ICU admission was 17 days (IQR 4–32 days) and had no impact on hospital survival (OR 1, p = 0.53).
We considered patients who were admitted until 1 day after first organ injury as a single subgroup and compared their clinical characteristics with patients who were admitted more than 1 day after first organ injury. Patients who were admitted later on to the ICU had a longer interval between diagnosis and allogeneic SCT, received more lines of treatment before allogeneic SCT, and were most likely to have received a RIC regimen (Supplementary Table 3). Although they had similar SOFA at admission to the ICU, patients with a longer time between first organ injury and ICU admission were more likely to have multi-organ failure (Supplementary Fig. 2B). Patients who spent more than 1 day with organ injury before ICU admission has a median OS of 64 days versus 118 days for those who spent less than 1 day (Supplementary Fig. 3b).
Elaboration of a prognostic score: number of organ injuries/day
A model with both clinical covariates—number of organ injuries and time between first organ injury and ICU admission—grouped into three groups was constructed. In this model, patients with > 2 organ injuries prior to ICU admission and time > 1 day between first organ injury and ICU admission had the greatest odds of in-hospital mortality (Table 3). The group with 0 or 1 organ injury prior to ICU admission was the reference category for the number of organ injuries; the group with less than 1 day between first organ injury and ICU admission was the reference category for time between first organ injury and ICU admission. Intermediate groups for both covariates did not significantly differ from the reference group. The group of patients with > 2 organ injuries had significant higher in-hospital mortality whereas patients who were admitted to the ICU > 1 day after first organ injury had non-significant higher in-hospital mortality. For further model understanding, we constructed a graph (Fig. 1) to show the joint effect of the number of organ injuries and time between first organ injury and ICU admission. Patients in the group with two organ injuries with admission more than 1 day after first organ injury had the highest risk of in-hospital survival compared with their respective reference groups.
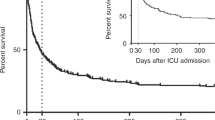
When integrating these two covariates, it appears that patients with higher organ injuries/day had significantly higher in-hospital mortality rate even after adjustment for refractory acute GVHD and the SOFA (OR 1.3, 95% CI 1–1.7, p = 0.02). There was a clear cut-off in in-hospital mortality for those with more than two organ injuries/day (Fig.2). After excluding patients who died in the ICU, there was a trend for those with more than two organ injuries/day to have a longer length of stay in the ICU (9 vs 5 days, p = 0.14). These patients were more heavily pretreated and thus had a greater interval from diagnosis to allogeneic SCT (Table 4). Patients with more than two organ injury/day had a median OS of 156 days versus 384 days for those with less than two organ injury/day (Fig. 3).
In-hospital mortality according to the number of organ injuries/day. This score is equivalent to the sum of days spent with each individual organ injury. For example, a patient with respiratory injury for 2 days and hemodynamic injury for 1 day had three organ injuries/day. Also, a patient with renal injury for 3 days and altered mental status for 2 days had five organ injuries/day
Discussion
In our extension study, we showed that allogeneic SCT recipients admitted earlier on to the ICU as soon as they show signs of organ injury fared better. Patients who were admitted later on following the first organ injury (> 1 day) or with more organ injuries (> 2 organ injuries) had a worst outcome. The development of a score combining these two parameters—the number of organ injuries/day—further improved the prediction of in-hospital survival after ICU admission.
It has been previously shown that in the general hospitalized population, patients who spend more time in the hospital before admission to the ICU had higher mortality [16]. Based on the identification of organ injuries, it might be possible to establish which patients would benefit from early admission to the ICU before severe organ failures occur [17, 18]. This has been demonstrated in patients with malignancies admitted to the ICU but not specifically in allogeneic SCT recipients [2, 17, 19, 20]. A previous study evaluating the implementation of an early ICU admission policy of patients with hematological disorders showed that despite an increase in MV in the latter period, 6-month survival was improved in patients who were admitted earlier on. This improvement was even more prominent in HSCT patients (19% in 2004 versus 36% in 2006–2008) [13].
Our findings suggest that early admission to the ICU might benefit allogeneic SCT patients. The perceived worst outcome of allogeneic SCT recipients might be responsible for delayed ICU admission. Late ICU admission might be responsible for increased organ injury and increased requirement for organ support. Patients who stayed longer on the hospital ward with one or more organ injuries were more likely to die in the hospital than those who were admitted immediately after the first sign of organ injury (OR 1.4, 95% CI 1.1–1.8, p = 0.02). Similar outcomes were found with patients accumulating organ injuries at the time of admission to the ICU (OR 1.7, 95% CI 1–2.7, p = 0.04). This last parameter was less relevant as these patients had a higher SOFA at ICU admission. With this parameter, we selected patients who were more likely to have multi-organ failure and thus have a worst outcome. By developing a score combining these covariates—the number of organ injuries/day—we could improve the prediction value of early ICU admission on hospital survival. Indeed, patients with higher organ injuries/day had significantly higher in-hospital mortality rate even after adjustment for refractory acute GVHD and the SOFA (OR 1.3, 95% CI 1–1.7, p = 0.02). Median overall survival was increased from 156 to 384 days in patients admitted earlier on with less organ injuries. These results compare favorably with previous work where allogeneic SCT recipients admitted to the ICU had a median overall survival of roughly 1 month [6, 13].
As in previous studies incorporating tack and trigger warning systems (TTs), we chose the alteration of physiological parameters for defining organ injuries except for the need of oxygen therapy which defined respiratory injury [13]. Even though our criteria for organ injury identified less severely injured patients, in comparison to other studies, our criteria were more readily usable on a general ward [21]. Mokart and colleagues advocate that oxygen requirement should be a trigger sign for ICU referral which may have two benefits: intensive diagnostic strategy and optimized organ support [22]. This may include invasive microbial diagnostic techniques such as bronchoalveolar lavage, mechanical ventilation—invasive or not—or hemodynamic monitoring to improve fluid resuscitation and vasopressor administration. This can translate into earlier stabilization and prevention of multi-organ failure which is the most important prognostic factor of allogeneic SCT recipients admitted to the ICU [12, 21]. Unfortunately, these TTs cannot identify patients deteriorating most rapidly who are not infrequent [23]. Prospective studies recording physiological parameters regularly are warranted to develop robust TTs for early admission to the ICU. It will be of interest to compare the EWS score to the score described herein.
The effect of early admission to the ICU is difficult to interpret as patients admitted early or later have different characteristics. As in another study, patients who were admitted later on were more heavily pretreated and had therefore a poorer prognosis (greater number of previous lines of treatment, longer time between diagnosis and graft procedure) [22]. Also, patients with more organ injuries prior to ICU admission were older and had a higher comorbidity score. Older age, comorbidities, and potential toxicity from previous lines of treatment can be responsible for diminished organ function, higher organ injury, and increased mortality after ICU admission. This might confound the impact of early ICU admission. In addition, the reason for delayed intervention could not be evaluated in our retrospective cohort. In a previous study evaluating the outcome of patients considered for ICU admission, whether they were admitted or not, showed that there was reluctance to admit patients with poor health status and not being in remission from their malignancy [24]. Due to poorer outcomes, there might be reluctance to admit patients with allogeneic SCT who may require MV [4]. Thiery and colleagues showed that some patients were admitted later on to the ICU because they were initially considered too well to benefit from intensive care. Interestingly, these patients had a worst outcome than patients who were admitted earlier on further advocating for early ICU admission [24].
Given its retrospective nature, our study could not include patients who presented with organ injury but were not admitted to the ICU and so outcome of these patients is unknown. Thus, patients who died or those who improved their organ injury without ICU admission were not analyzed. It will be important to include these patients in future studies to clearly describe the evolution from organ injury to organ failure and the impact ICU admission can have. We therefore cannot draw definitive conclusions regarding the benefit of early ICU admission to all patients with organ injury. Also, the small number of patients does not enable extensive multivariate analysis. Multicenter studies with large number of patients are therefore warranted to validate our score. Our study was conducted at a single institution with a specialized ICU for critically ill cancer patients, which may limit the generalizability of our findings to other centers. However, we give for the first time some insight on the early admission of exclusively allogeneic SCT recipients admitted to the ICU. Early ICU admission of critically ill allogeneic SCT recipients as soon as they develop organ injury might exceed ICU capacity and might even be responsible for specific complications such as infections due to invasive procedures. The implementation of intermediate level care such as dopamine or high flux oxygenation on the general ward could also be of interest. The feasibility and the cost-effectiveness of such a policy must be evaluated prospectively.
In conclusion, we show that early admission to the ICU benefits allogeneic SCT recipients. Time from first organ injury to ICU admission and the number of organ injuries prior to the admission to the ICU are associated with worse survival. The development of a score incorporating these two covariates—the number of organ injuries/day—further improved the prediction value of early admission on hospital survival.
References
Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, Afessa B (2011) Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care 1(1):5
Azoulay E, Mokart D, Pene F, Lambert J, Kouatchet A, Mayaux J, Vincent F, Nyunga M, Bruneel F, Laisne LM et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol 31(22):2810–2818
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, Martin PJ, Sandmaier BM, Marr KA, Appelbaum FR et al (2010) Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med 363(22):2091–2101
Pene F, Aubron C, Azoulay E, Blot F, Thiery G, Raynard B, Schlemmer B, Nitenberg G, Buzyn A, Arnaud P et al (2006) Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol 24(4):643–649
Gilli K, Remberger M, Hjelmqvist H, Ringden O, Mattsson J (2010) Sequential organ failure assessment predicts the outcome of SCT recipients admitted to intensive care unit. Bone Marrow Transplant 45(4):682–688
Bayraktar UD, Shpall EJ, Liu P, Ciurea SO, Rondon G, de Lima M, Cardenas-Turanzas M, Price KJ, Champlin RE, Nates JL (2013) Hematopoietic cell transplantation-specific comorbidity index predicts inpatient mortality and survival in patients who received allogeneic transplantation admitted to the intensive care unit. J Clin Oncol 31(33):4207–4214
Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G (2014) Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant 49(1):62–65
Soubani AO, Kseibi E, Bander JJ, Klein JL, Khanchandani G, Ahmed HP, Guzman JA (2004) Outcome and prognostic factors of hematopoietic stem cell transplantation recipients admitted to a medical ICU. Chest 126(5):1604–1611
Depuydt P, Kerre T, Noens L, Nollet J, Offner F, Decruyenaere J, Benoit D (2011) Outcome in critically ill patients with allogeneic BM or peripheral haematopoietic SCT: a single-centre experience. Bone Marrow Transplant 46(9):1186–1191
Townsend WM, Holroyd A, Pearce R, Mackinnon S, Naik P, Goldstone AH, Linch DC, Peggs KS, Thomson KJ, Singer M et al (2013) Improved intensive care unit survival for critically ill allogeneic haematopoietic stem cell transplant recipients following reduced intensity conditioning. Br J Haematol 161(4):578–586
Moreau AS, Seguin A, Lemiale V, Yakoub-Agha I, Girardie P, Robriquet L, Mangalaboyi J, Fourrier F, Jourdain M (2014) Survival and prognostic factors of allogeneic hematopoietic stem cell transplant recipients admitted to intensive care unit. Leuk Lymphoma 55(6):1417–1420
Orvain C, Beloncle F, Hamel JF, Thépot S, Mercier M, Kouatchet A, Farhi J, Francois S, Guardiola P, Asfar P et al (2016) Different impact of the number of organ failures and graft-versus-host disease on the outcome of allogeneic stem cell transplantation recipients requiring intensive care. Transplantation
Bokhari SW, Munir T, Memon S, Byrne JL, Russell NH, Beed M (2010) Impact of critical care reconfiguration and track-and-trigger outreach team intervention on outcomes of haematology patients requiring intensive care admission. Ann Hematol 89(5):505–512
Kellum JA, Lameire N, Group KAGW (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care 17(1):204
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine Crit Care Med 26(11):1793–1800
Goldhill DR, McNarry AF, Hadjianastassiou VG, Tekkis PP (2004) The longer patients are in hospital before intensive care admission the higher their mortality. Intensive Care Med 30(10):1908–1913
Song JU, Suh GY, Park HY, Lim SY, Han SG, Kang YR, Kwon OJ, Woo S, Jeon K (2012) Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med 38(9):1505–1513
Lee DS, Suh GY, Ryu JA, Chung CR, Yang JH, Park CM, Jeon K (2015) Effect of early intervention on long-term outcomes of critically ill Cancer patients admitted to ICUs. Crit Care Med 43(7):1439–1448
Lengliné E, Raffoux E, Lemiale V, Darmon M, Canet E, Boissel N, Schlemmer B, Dombret H, Azoulay E (2012) Intensive care unit management of patients with newly diagnosed acute myeloid leukemia with no organ failure. Leuk Lymphoma 53(7):1352–1359
de Montmollin E, Tandjaoui-Lambiotte Y, Legrand M, Lambert J, Mokart D, Kouatchet A, Lemiale V, Pène F, Bruneel F, Vincent F et al (2013) Outcomes in critically ill cancer patients with septic shock of pulmonary origin. Shock 39(3):250–254
Hayani O, Al-Beihany A, Zarychanski R, Chou A, Kharaba A, Baxter A, Patel R, Allan DS (2011) Impact of critical care outreach on hematopoietic stem cell transplant recipients: a cohort study. Bone Marrow Transplant 46(8):1138–1144
Mokart D, Lambert J, Schnell D, Fouché L, Rabbat A, Kouatchet A, Lemiale V, Vincent F, Lengliné E, Bruneel F et al (2013) Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk Lymphoma 54(8):1724–1729
Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, Esmonde L, Goldhill DR, Parry GJ, Rashidian A et al (2007) Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med 33(4):667–679
Thiery G, Azoulay E, Darmon M, Ciroldi M, De Miranda S, Levy V, Fieux F, Moreau D, Le Gall JR, Schlemmer B (2005) Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 23(19):4406–4413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 350 kb)
Rights and permissions
About this article
Cite this article
Orvain, C., Beloncle, F., Hamel, JF. et al. Allogeneic stem cell transplantation recipients requiring intensive care: time is of the essence. Ann Hematol 97, 1601–1609 (2018). https://doi.org/10.1007/s00277-018-3320-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3320-y