Abstract
Recent reports identify NLR (the ratio between absolute neutrophils counts, ANC, and absolute lymphocyte count, ALC), as predictor of progression-free survival (PFS) and overall survival (OS) in cancer patients. We retrospectively tested NLR and LMR (the ratio between absolute lymphocyte and monocyte counts) in newly diagnosed Hodgkin lymphoma (HL) patients treated upfront with a PET-2 risk-adapted strategy. NLR and LMR were calculated using records obtained from the complete blood count (CBC) from 180 newly diagnosed HL patients. PFS was evaluated accordingly to Kaplan-Meier method. Higher NLR was associated to advanced stage, increased absolute counts of neutrophils and reduced count of lymphocytes, and markers of systemic inflammation. After a median follow-up of 68 months, PFS at 60 months was 86.6% versus 70.1%, respectively, in patients with NLR ≥ 6 or NLR < 6. Predictors of PFS at 60 months were PET-2 scan (p < 0.0001), NLR ≥ 6.0 (p = 0.02), LMR < 2 (p = 0.048), and ANC (p = 0.0059) in univariate analysis, but only PET-2 was an independent predictor of PFS in multivariate analysis. Advanced-stage patients (N = 119) were treated according to a PET-2 risk-adapted protocol, with an early switch to BEACOPP regimen in case of PET-2 positivity. Despite this strategy, patients with positive PET-2 still had an inferior outcome, with PFS at 60 months of 84.7% versus 40.1% (negative and positive PET-2 patients, respectively, p < 0.0001). Independent predictors of PFS by multivariate analysis were PET-2 status and to a lesser extend NLR in advanced stage, while LMR maintained its significance in early stage. By focusing on PET-2 negative patients, we found that patients with NLR ≥ 6.0 or LMR < 2 had an inferior outcome compared to patients with both ratios above the cutoff (78.7 versus 91.9 months, p = 0.01). We confirm NLR as predictor of PFS in HL patients independently from stage at diagnosis. Integration of PET-2 scan, NLR and LMR can result in a meaningful prognostic system that needs to be further validated in prospective series including patients treated upfront with PET-2 adapted-risk therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical outcome in Hodgkin lymphoma (HL) is partly due to the loss of critical mediators of immune surveillance, due to expansion of dysfunctional and immune-suppressive myeloid progenitors [1,2,3]. Despite the high rate of deep and durable responses, relapses after first-line therapy can occur in 20–30% of patients with advanced-stage HL [4].
Unfortunately, current prognostic models have not been shown to be very accurate in early detection of patients at high risk of shortened survival. A major prognostic system used in advanced HL is the International Prognostic System (IPS), based on the retrospective international series of more than 5000 patients treated with ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) or ABVD-like regimens. However, IPS has scarce clinical utility because only 19% of patients with scores 4 and 5 had a probability of 7-year-progression-free survival (PFS) < 50% [5, 6].
Positive 18F-fluoro-2-deoxy-glucose (FDG) uptake in positron emission tomography (PET) scan performed early after first two cycles of chemotherapy (PET-2) [7,8,9,10] is the most reliable tool to predict outcome [11] and to base a risk-adapted strategy [11,12,13]. PET-2 is considered a surrogate test of tumor chemosensitivity and when positive indicates the persistence of the reactive microenvironment with high glycolytic activity [11, 14, 15].
Indeed, PET-2 information is available only during treatment and biological mechanisms leading to chemoresistance may be activated as early as after two cycles of treatment; thus, a warning to address patients to treatment switch to a more aggressive regimen in an escalating, risk-adapted strategy could be helpful in clinical management.
Starting from the clinical observation that the amount of tumor-associated macrophages (TAM) in the diagnostic biopsy [16] is predictive of outcome mirroring the complex network of cells and cytokines in HL microenvironment, our group previously showed the clinical impact of myeloid-derived suppressor cells and their key enzyme arginase-1 at diagnosis [1, 2].
Since MDSC count and Arg-1 represent the effect of the myeloid axis on the immune cells, we hypothesized that the ratio between absolute neutrophils (ANC) and lymphocyte count (ALC), known as NLR, could mirror the subtle relationship between the myeloid microenvironment and the lymphoid system. In this perspective, we asked if NLR could be integrated with available information at diagnosis to identify early patients with high risk of poor outcome.
Indeed, ALC as a surrogate of host immunity impairment is a prognostic factor for advanced-stage HL, being part of the international prognostic factor (IPS) [6]. In particular, T cell function is impaired in HL, with a depressed T cell-mediated response, mainly due to a defective T cell receptor CD3ζ chain expression, accumulation of Th2 cells, and immunosuppressive regulatory T cells (T-reg) [3].
The increased amount of granulocytes is common in HL, as a consequence of inflammation status, associated to a negative prognosis [2, 17] despite that it is not included in the International Prognostic Index (IPS) [6]. Our previous work showed that granulocytes in HL are dysfunctional, since they exhibit a reduced phagocytic activity despite presence of activation signaling as shown by high levels of CD11b on the surface and they are able to reduce CD3ζ expression and other activation markers on the cell surface of T lymphocytes [2]. In addition, we have demonstrated that neutrophils correlate with myeloid-derived suppressor cells (MDSC) and indeed they may represent their mature counterpart [1, 2, 18]. Therefore, the NLR ratio may be representative of both the number of immunosuppressive mediators and the ability of the host to mount an immune response against the tumor.
NLR has been reported as an independent prognostic marker in solid and hematological cancers [19], including myeloma [20] and lymphoma [21, 22].
Another easily assessable variable is the LMR (lymphocytes to monocytes ratio) that could be a projection in peripheral blood of both tumor-infiltrating lymphocytes and TAM. LMR has been identified as an independent prognostic factor for survival in patients with classical HL [19, 23]. However, the impact of both NLR and LMR on the outcome of patients treated upfront with PET-2 risk-adapted strategy and its role in PET-2 era has never been investigated in HL.
Methods
Study design
In this retrospective study, we reviewed 190 files of patients with HL newly diagnosed at our institution between January 2006 and June 2012. Ten patients were excluded because history of HIV or immune-suppression therapy. Thirty healthy subjects were included in the study to evaluate normal range of NLR and LMR.
In all patients, CBC and routine biochemical examinations were taken before start treatment. White blood cell count and types (neutrophil, lymphocyte, eosinophil, and monocyte) were determined by electrical impedance method in automatic blood counter device (Beckman Coulter LH 750).
The study was approved by the local institutional review board. All participants gave a written informed consent in accord to the Declaration of Helsinki.
Basic characteristics, treatment, and clinical outcome are summarized respectively in Tables 1 and 2.
For patients with advanced disease (Ann-Arbor stage ≥ IIB), treatment consisted of six cycles according to ABVD regimen (doxorubicin, bleomycin, vinblastine, and dacarbazine) [24, 25], followed by involved field radiotherapy if clinically indicated. PET-2 positive patients were shifted to BEACOPP regimen (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) for eight cycles and, in case of persistent disease, a bone marrow autologous transplant was performed [12]. Early-stage patients received two or four or six courses of ABVD chemotherapy plus involved field radiotherapy as clinically indicated.
Both baseline and PET-2 were performed using standard technique and a semi-quantitative Deauville score was attributed to each image [26, 27]. A minimally positive scan was defined as any scan with any residual FDG uptake outside the physiological areas of the tracer concentration (mediastinal blood pool and liver) [28].
Statistical analysis
Qualitative results were summarized in counts and percentages. Descriptive statistics were generated for analysis of results and p value under 0.05 was considered significant.
The correlation of ANC, ALC, and NLR with various parameters was assessed with Pearson’s chi-square test (or Fisher’s exact test) for categorical parameters and with Mann-Whitney or Wilcoxon signed rank test for continuous parameters.
PFS was calculated from the time of inclusion until the date of progression, relapse, death, or the date the patient was last known to be in remission; positivity of PET-2 was not considered as an event. PFS was analyzed by Kaplan-Meier test. Standard errors were calculated by the method of Greenwood; the 95% confidence intervals are computed as 1.96 times the standard error in each direction. The Cox proportional hazards model was used to evaluate NLR or LMR at diagnosis as a prognostic marker for PFS, as well as to assess and adjust with other known prognostic factors.
All calculations were performed using Graph Pad Prism version 6.00 for Windows, Graph Pad Software, San Diego, CA, USA. A stepwise multivariate regression analysis of survival was performed using MedCalc Statistical Software version 13.0.6 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2014).
Results
NLR and LMR are increased in HL
In this series, the median age was 31.7 years old (range 14.8–76.9), and half patients were males (Table 1). The median ANC, ALC, and NLR at diagnosis were 7.74 × 103/μL, 1.47 × 103/μL, and 5.00, respectively.
Median NLR was significantly higher in patients with HL than controls (5.0, range 0.6–16.2 versus 1.6, range 0.2–3.1, respectively, p < 0.001). Higher NLR was associated to advanced stage (p = 0.05), increased ANC (p < 0.0001) and reduced ALC (p < 0.0001), increased marker of systemic inflammation ESR (p = 0.004), but not C-reactive protein or ferritin.
Median LMR was significantly lower in patients with HL than controls (2.1, range 0.2–8.4 versus 3.1, range 0.6–4.0, respectively, p < 0.0001), significantly associated to lower ALC, increased ANC, AMC, and NLR (p < 0.0001), advanced stage (p = 0.002), and high IPS (p < 0.0001) as shown in Table 1.
NLR and LMR are associated to PET-2 positivity and clinical outcome
After two ABVD cycles, out of 180 patients included in the study, 25 (14%) had a positive PET-2 (10 with score 4 and 15 with score 5) and 155 (86%) a negative PET-2 (Fig. 1). PET-2 positive patients had a higher median NLR (7.4 versus 4.8, p = 0.0015, Fig. 2a), higher in patients with DS5 than DS4 or DS3 (p = 0.01, Fig. 2b), and lower median LMR (1.7 versus 2.3, p = 0.0027, Fig. 2c), lower in patients with DS5 than DS4 or DS3 (p = 0.001, Fig. 2d).
Positive PET-2 is associated to increased NLR and reduced LMR at diagnosis. Pre-treatment median NLR was increased in patients with positive PET-2 (a), higher in patients with Deauville score (DS) 5 (b)—carrying new lesion, than DS4 (residual activity). Similarly, pre-treatment median LMR was reduced in patients with positive PET-2 (c), lower in DS5 than in DS4 patients (d)
Advanced-stage PET-2 positive patients (21/119) were allocated to the escalated BEACOPP program, refused, or not completed in five cases, while 98 PET-2 negative patients continued with four additional ABVD, followed by consolidation radiotherapy on initial bulky nodal site of disease in 24 cases (Table 2). One early death for infection occurred among PET-2 advanced-stage negative patients. A third PET evaluation was performed at the end of planned treatment (PET-3) and a treatment failure within 2 years was registered in 9/97 PET-2 negative as compared to 14/21 PET-2 positive (Fig. 1).
In early-stage patients, therapy was not modified according to the PET-2 results. Based on disease extension, ABVD cycles were followed by involved field 30-Gy radiotherapy (ifRT); except in four cases in which for medical conditions and patient’s will, treatment was extended to six cycles ABVD, two of them without success and later treated with salvage regimen IGEV and autologous stem cell transplantation (Table 2).
After a median follow-up of 68 months (range 5.4–84.4 months), 136 patients (75.5%) were in continued complete remission (cCR), 23 patients (13%) progressed during therapy or immediately after (during the first 6 months), 20 relapsed (11%) within 2 years from end treatment, and one died for infection before completing the planned cycles (Table 2). Achieving and maintaining cCR were associated to lower median NLR (4.8 versus 7.7, p < 0.0001) and higher LMR (2.4 versus 1.3, p = 0.002) than treatment failure (Fig. 2e–f).
To define a cutoff point, the choice of NLR ≥ 6 was based on two strategies: (i) a value higher than mean plus two standard deviations in healthy subjects and (ii) the greatest differential to segregate cohorts, based on the Χ2 value (Χ2 = 96.6, p value < 0.0001) analyzed at different cutoff points between the 25 and 75% quartiles from the log-rank test. In addition, NLR ≥ 6 and LMR < 2 have been previously identified in large series previously published [19, 21, 23, 29, 30].
Receiver-operator characteristic curves (ROCs) were generated and area under curves (AUCs) were calculated to assess the utility of NLR and LMR to predict treatment failure at diagnosis. The AUC for NLR was 0.71 (95% CI = 0.61–0.82, p = 0.0001); using NLR ≥ 6 as cutoff, treatment failure was identified with sensitivity of 66.4% (95% CI = 58.1–74.0) and specificity of 67.6 (95% CI = 49.4–82.6). The AUC for LMR was 0.71 (95% CI = 0.61–0.82, p = 0.0001); LMR < 2 could identify treatment failure with sensitivity of 73.5% (95% CI = 55.6–87.1) and specificity of 62.3 (95% CI = 53.9–70.2).
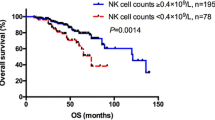
NLR and LMR can predict clinical outcome in HL patients
In the whole cohort, 5-year PFS was 79.8%, lower in patients carrying NLR ≥ 6 at diagnosis compared to NLR < 6 (86.6% versus 70.1%, p = 0.002, Fig. 3a). Similarly, 5-year PFS was lower in patients carrying LMR < 2 at diagnosis compared to LMR ≥ 2 (70.2% versus 87.7%, p = 0.004, Fig. 3b). Predictors of 5-year PFS were PET-2 scan (p < 0.0001), NLR ≥ 6.0 (p = 0.002), and LMR < 2 (p = 0.004) in univariable analysis, but only PET-2 was maintained in multivariate analysis (Table 3).
PFS in newly diagnosed HL patients based on pre-treatment NLR, LMR, stage, and PET scan after two cycles of chemotherapy. Progression-free survival in 180 newly diagnosed HL patients based on NLR ≥ 6 (a) and LMR < 2 (b). In 119 advanced-stage patients treated with a PET-2 risk-adapted strategy PET-2 status maintained its prognostic role (c). In 61 early-stage patients, LMR < 2 at diagnosis was associated to inferior outcome (d)
Advanced-stage patients with positive PET-2 had an inferior outcome, with 5-year PFS of 84.7% versus 40.1%, respectively, in negative and positive PET-2 patients, p < 0.0001, Fig. 3c). Thus, in advanced-stage patients, ALC (p = 0.017), PET-2 (p < 0.0001), and NLR ≥ 6 (p = 0.013) were predictors of 5-year PFS in univariate analysis, but only PET-2 and barely NLR were maintained in multivariate analysis (Table 3). In early-stage patients, only LMR < 2 could predict 5-year PFS in both univariate analysis (73.3 versus 90.4%, p = 0.03) and multivariate analysis (p = 0.02, Table 3, Fig. 3d).
Finally, since the heterogeneity of treatment due to a PET-2 risk-adapted strategy, we analyzed separately NLR ≥ 6 and LMR < 2 to predict clinical outcome in PET-2 negative patients (N = 155, N = 98 advanced stage and N = 57 early stage). We found that carrying NLR ≥ 6 or LMR < 2 at diagnosis was associated to inferior outcome, with 5-year PFS of 78.7 versus 91.9% in NLR < 6 and LMR ≥ 2 (HR 3.1, 95% CI 1.4–6.8, p = 0.01 Fig. 4).
Discussion
A high NLR has been reported to have a negative prognostic impact in several solid and liquid tumors [20, 30,31,32,33,34]. A recent report indicates that a NLR ≥ 6 or LMR < 2 could be considered robust and negative prognostic factor for both PFS and OS also in HL patients [19, 30]. However, in both series, a formal comparison with long-term outcome in patients treated upfront with a PET-2 risk-adapted strategy is missed.
Thus, we retrospectively evaluated the prognostic significance of NLR in newly diagnosed patients treated upfront with a PET-2 risk-adapted strategy and our findings confirmed the importance of NLR in predicting PFS, in both early- and advanced-stage patients. Since higher NLR was associated to reduced LMR and some reports in pre-PET-2 era suggested a prognostic role for LMR [23], we tested the prognostic meaning of LMR that resulted to be a significant variable in predicting PFS in univariate but not in multivariate analysis, confirming our previous observations in a similar setting [8].
In our series, advanced-stage patients with PET-2 positive scan received a more aggressive regimen, switching from ABVD to BEACOPP. Recently, three phase 3 clinical trials, the U.K. RATHL [35], the American S081626 trial [36], and Italian GITIL/FIL HD0607 (Gallamini, manuscript in press) demonstrated the clinical benefit of this escalating PET-adapted strategy.
While a PET-2-adapted strategy can improve outcome in PET-2 positive patients, a backbone of around 10% of PET-2 negative patients is still at risk of relapse. For these patients, a bio-PET has been proposed, to integrate information about immune system and cancer features [18]. NLR, more than LMR, could reflect the immunosuppressive capacity of both mature and immature myeloid cells that are elevated in the peripheral blood, secrete arginase, and are positively associated to TAM [1, 2]. Several groups identified LMR as independent prognostic factor [19, 23], but we and others have found its role in the cohort of early-stage patients only [37].
In HL microenvironment, the immune-suppressive component has prognostic meaning also when evaluated in the lymph-node biopsies, integrating the prognostic importance of PET-2 scan [18]. Especially in advanced-stage patients, the current IPS has low sensitivity and specificity, taking in account clinical parameters like hemoglobin and sex that have lost their importance in the last years thanks to supportive care improvement [38, 39]. Interestingly, in our series, the IPS was unable to provide any clear distinction in the outcomes for PFS. In contrast, the addition of NLR to PET-2 scan was the only independent variable able to identify patients with poor prognosis, giving NLR a clear and cheap means of prognostication at diagnosis.
Our study has several important limitations. First, this study is retrospective and, therefore, subject to inherent limitations and biases, including change of therapy based on PET-2 status. Thus, validation of the utility of NLR and LMR in an independent multicenter cohort of PET-2 negative patients treated with the same scheme is needed.
In conclusion, pre-treatment NLR is significantly associated with increased risk of treatment failure in advanced stage HL, while LMR in early-stage patients, even if in case of negative PET-2.
References
Romano A, Parrinello NL, Vetro C, Forte S, Chiarenza A, Figuera A, Motta G, Palumbo GA, Ippolito M, Consoli U, Raimondo FD (2015) Circulating myeloid-derived suppressor cells correlate with clinical outcome in Hodgkin lymphoma patients treated up-front with a risk-adapted strategy. Br J Haematol 168:689–700
Romano A, Parrinello NL, Vetro C, Tibullo D, Giallongo C, la Cava P, Chiarenza A, Motta G, Caruso AL, Villari L, Tripodo C, Cosentino S, Ippolito M, Consoli U, Gallamini A, Pileri S, di Raimondo F (2016) The prognostic value of the myeloid-mediated immunosuppression marker arginase-1 in classic Hodgkin lymphoma. Oncotarget 7:67333–67346
Romano A, Vetro C, Caocci G et al (2014) Immunological deregulation in classic Hodgkin lymphoma. Mediterr J Hematol Infect Dis 6:e2014039
Gallamini A, Kostakoglu L (2012) Positron emission tomography/computed tomography surveillance in patients with lymphoma: a fox hunt? Haematologica 97:797–799
Hasenclever D (2002) The disappearance of prognostic factors in Hodgkin’s disease. Ann Oncol 13(Suppl 1):75–78
Hasenclever D, Diehl VA (1998) Prognostic score for advanced Hodgkin’s disease. International prognostic factors project on advanced Hodgkin’s disease. N Engl J Med 339:1506–1514
Gallamini A, Hutchings M, Rigacci L, Specht L, Merli F, Hansen M, Patti C, Loft A, di Raimondo F, D'Amore F, Biggi A, Vitolo U, Stelitano C, Sancetta R, Trentin L, Luminari S, Iannitto E, Viviani S, Pierri I, Levis A (2007) Early interim 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography is prognostically superior to international prognostic score in advanced-stage Hodgkin’s lymphoma: a report from a joint Italian-Danish study. J Clin Oncol 25:3746–3752
Romano A, Vetro C, Donnarumma D, Forte S, Ippolito M, di Raimondo F (2012) Early interim 2-(1)fluoro-2-deoxy-D-glucose positron emission tomography is prognostically superior to peripheral blood lymphocyte/monocyte ratio at diagnosis in classical Hodgkin’s lymphoma. Haematologica 97:e21–e23 author reply e24
Gallamini A, Di Raimondo F, La Nasa G et al (2013) Standard therapies versus novel therapies in Hodgkin lymphoma. Immunol Lett 155:56–59
Oki Y, Chuang H, Chasen B, Jessop A, Pan T, Fanale M, Dabaja B, Fowler N, Romaguera J, Fayad L, Hagemeister F, Rodriguez MA, Neelapu S, Samaniego F, Kwak L, Younes A (2014) The prognostic value of interim positron emission tomography scan in patients with classical Hodgkin lymphoma. Br J Haematol 165:112–116
Gallamini A, Kostakoglu L (2012) Interim FDG-PET in Hodgkin lymphoma: a compass for a safe navigation in clinical trials? Blood 120:4913–4920
Gallamini A, Patti C, Viviani S, Rossi A, Fiore F, di Raimondo F, Cantonetti M, Stelitano C, Feldman T, Gavarotti P, Sorasio R, Mulè A, Leone M, Rambaldi A, Biggi A, Barrington S, Fallanca F, Ficola U, Chauvie S, Gianni AM, for the Gruppo Italiano Terapie Innovative nei Linfomi (GITIL) (2011) Early chemotherapy intensification with BEACOPP in advanced-stage Hodgkin lymphoma patients with an interim-PET positive after two ABVD courses. Br J Haematol 152:551–560
Zinzani PL, Broccoli A, Gioia DM, Castagnoli A, Ciccone G, Evangelista A, Santoro A, Ricardi U, Bonfichi M, Brusamolino E, Rossi G, Anastasia A, Zaja F, Vitolo U, Pavone V, Pulsoni A, Rigacci L, Gaidano G, Stelitano C, Salvi F, Rusconi C, Tani M, Freilone R, Pregno P, Borsatti E, Sacchetti GM, Argnani L, Levis A (2016) Interim positron emission tomography response-adapted therapy in advanced-stage Hodgkin lymphoma: final results of the phase II part of the HD0801 study. J Clin Oncol 34:1376–1385
Sica A, Porta C, Morlacchi S, Banfi S, Strauss L, Rimoldi M, Totaro MG, Riboldi E (2012) Origin and functions of tumor-associated myeloid cells (TAMCs). Cancer Microenviron 5:133–149
Sica A, Strauss L, Consonni FM, Travelli C, Genazzani A, Porta C (2017) Metabolic regulation of suppressive myeloid cells in cancer. Cytokine Growth Factor Rev 35:27–35
Steidl C, Lee T, Shah SP, Farinha P, Han G, Nayar T, Delaney A, Jones SJ, Iqbal J, Weisenburger DD, Bast MA, Rosenwald A, Muller-Hermelink HK, Rimsza LM, Campo E, Delabie J, Braziel RM, Cook JR, Tubbs RR, Jaffe ES, Lenz G, Connors JM, Staudt LM, Chan WC, Gascoyne RD (2010) Tumor-associated macrophages and survival in classic Hodgkin’s lymphoma. N Engl J Med 362:875–885
Schreck S, Friebel D, Buettner M, Distel L, Grabenbauer G, Young LS, Niedobitek G (2009) Prognostic impact of tumour-infiltrating Th2 and regulatory T cells in classical Hodgkin lymphoma. Hematol Oncol 27:31–39
Agostinelli C, Gallamini A, Stracqualursi L et al (2016) The combined role of biomarkers and interim PET scan in prediction of treatment outcome in classical Hodgkin's lymphoma: a retrospective, European, multicentre cohort study. Lancet Haematol 3:e467–e479
Porrata LF, Ristow K, Colgan JP, Habermann TM, Witzig TE, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, Nowakowski GS, Thompson C, Markovic SN (2012) Peripheral blood lymphocyte/monocyte ratio at diagnosis and survival in classical Hodgkin’s lymphoma. Haematologica 97:262–269
Kelkitli E, Atay H, Cilingir F et al (2014) Predicting survival for multiple myeloma patients using baseline neutrophil/lymphocyte ratio. Ann Hematol 93(5):841–846. https://doi.org/10.1007/s00277-013-1978-8
Koh YW, Kang HJ, Park C, Yoon DH, Kim S, Suh C, Kim JE, Kim CW, Huh J (2012) Prognostic significance of the ratio of absolute neutrophil count to absolute lymphocyte count in classic Hodgkin lymphoma. Am J Clin Pathol 138:846–854
Porrata LF, Ristow K, Habermann T, Inwards DJ, Micallef IN, Markovic SN (2010) Predicting survival for diffuse large B-cell lymphoma patients using baseline neutrophil/lymphocyte ratio. Am J Hematol 85:896–899
Porrata LF, Ristow KM, Habermann TM, Macon WR, Witzig TE, Colgan JP, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, Nowakowski G, Thompson CA, Markovic SN (2013) Peripheral blood absolute lymphocyte/monocyte ratio recovery during ABVD treatment cycles predicts clinical outcomes in classical Hodgkin lymphoma. Blood Cancer J 3:e110
Bonfante V, Santoro A, Viviani S et al (1992) ABVD in the treatment of Hodgkin's disease. Semin Oncol 19:38–44 discussion 44-35
Santoro A, Bonadonna G (1979) Prolonged disease-free survival in MOPP-resistant Hodgkin’s disease after treatment with adriamycin, bleomycin, vinblastine and dacarbazine (ABVD). Cancer Chemother Pharmacol 2:101–105
Barrington SF, Qian W, Somer EJ, Franceschetto A, Bagni B, Brun E, Almquist H, Loft A, Højgaard L, Federico M, Gallamini A, Smith P, Johnson P, Radford J, O’Doherty MJ (2010) Concordance between four European centres of PET reporting criteria designed for use in multicentre trials in Hodgkin lymphoma. Eur J Nucl Med Mol Imaging 37:1824–1833
Meignan M, Gallamini A, Itti E, Barrington S, Haioun C, Polliack A (2012) Report on the Third International Workshop on interim positron emission. Leuk Lymphoma 53:1876–1881
Gallamini A (2010) Positron emission tomography scanning: a new paradigm for the management of Hodgkin’s lymphoma. Haematologica 95:1046–1048
Koh YW, Kang HJ, Park C, Yoon DH, Kim S, Suh C, Go H, Kim JE, Kim CW, Huh J (2012) The ratio of the absolute lymphocyte count to the absolute monocyte count is associated with prognosis in Hodgkin’s lymphoma: correlation with tumor-associated macrophages. Oncologist 17:871–880
Marcheselli R, Bari A, Tadmor T et al (2016) Neutrophil-lymphocyte ratio at diagnosis is an independent prognostic factor in patients with nodular sclerosis Hodgkin lymphoma: results of a large multicenter study involving 990 patients. Hematol Oncol 35(4):561–566. https://doi.org/10.1002/hon.2359
Cho IR, Park JC, Park CH, Jo JH, Lee HJ, Kim S, Shim CN, Lee H, Shin SK, Lee SK, Lee YC (2014) Pre-treatment neutrophil to lymphocyte ratio as a prognostic marker to predict chemotherapeutic response and survival outcomes in metastatic advanced gastric cancer. Gastric Cancer 17:703–710
Mano Y, Shirabe K, Yamashita Y, Harimoto N, Tsujita E, Takeishi K, Aishima S, Ikegami T, Yoshizumi T, Yamanaka T, Maehara Y (2013) Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg 258:301–305
Romano A, Parrinello NL, Consoli ML, Marchionni L, Forte S, Conticello C, Pompa A, Corso A, Milone G, di Raimondo F, Borrello I (2015) Neutrophil to lymphocyte ratio (NLR) improves the risk assessment of ISS staging in newly diagnosed MM patients treated upfront with novel agents. Ann Hematol 94:1875–1883
Santoni M, De Giorgi U, Iacovelli R et al (2013) Pre-treatment neutrophil-to-lymphocyte ratio may be associated with the outcome in patients treated with everolimus for metastatic renal cell carcinoma. Br J Cancer 109:1755–1759
Johnson P, Federico M, Kirkwood A, Fosså A, Berkahn L, Carella A, d’Amore F, Enblad G, Franceschetto A, Fulham M, Luminari S, O’Doherty M, Patrick P, Roberts T, Sidra G, Stevens L, Smith P, Trotman J, Viney Z, Radford J, Barrington S (2016) Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s lymphoma. N Engl J Med 374:2419–2429
Press OW, Li H, Schoder H et al (2016) US intergroup trial of response-adapted therapy for stage III to IV Hodgkin lymphoma using early interim fluorodeoxyglucose-positron emission tomography imaging: Southwest Oncology Group S0816. J Clin Oncol 34:2020–2027
Reddy JP, Hernandez M, Gunther JR, Dabaja BS, Martin GV, Jiang W, Akhtari M, Allen PK, Atkinson BJ, Smith GL, Pinnix CC, Milgrom SA, Abou Yehia Z, Osborne EM, Oki Y, Lee H, Hagemeister F, Fanale MA (2018) Pre-treatment neutrophil/lymphocyte ratio and platelet/lymphocyte ratio are prognostic of progression in early stage classical Hodgkin lymphoma. Br J Haematol 180(4):545–549. https://doi.org/10.1111/bjh.15054
Moccia AA, Donaldson J, Chhanabhai M, Hoskins PJ, Klasa RJ, Savage KJ, Shenkier TN, Slack GW, Skinnider B, Gascoyne RD, Connors JM, Sehn LH (2012) International prognostic score in advanced-stage Hodgkin’s lymphoma: altered utility in the modern era. J Clin Oncol 30:3383–3388
Diefenbach CS, Li H, Hong F, Gordon LI, Fisher RI, Bartlett NL, Crump M, Gascoyne RD, Wagner H Jr, Stiff PJ, Cheson BD, Stewart DA, Kahl BS, Friedberg JW, Blum KA, Habermann TM, Tuscano JM, Hoppe RT, Horning SJ, Advani RH (2015) Evaluation of the international prognostic score (IPS-7) and a simpler prognostic score (IPS-3) for advanced Hodgkin lymphoma in the modern era. Br J Haematol 171:530–538
Funding
This work was supported by a grant from Ministero della Salute (Ricerca Finalizzata, 10/PE-2011-02350147, F.D.R and N.L.P.) and Fondazione Veronesi (A.R.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Romano, A., Parrinello, N.L., Vetro, C. et al. Prognostic meaning of neutrophil to lymphocyte ratio (NLR) and lymphocyte to monocyte ration (LMR) in newly diagnosed Hodgkin lymphoma patients treated upfront with a PET-2 based strategy. Ann Hematol 97, 1009–1018 (2018). https://doi.org/10.1007/s00277-018-3276-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3276-y