Abstract
In most cases of relapsed/refractory mantle cell lymphoma (MCL), patients respond to salvage therapy, though typically responses are partial and/or transient followed by disease progression, even with newer agents (e.g., ibrutinib). In this multicenter, open-label, single-arm, phase II study, patients with relapsed/refractory non-blastoid MCL received bendamustine 90 mg/m2 (days 1 and 2) and rituximab 375 mg/m2 (day 1) for 6 planned 28-day cycles. Functional imaging with 18-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) was conducted at baseline and after cycle 6. Forty-five patients were enrolled (median age, 70 years; 82 % stage IV disease; median number of prior chemotherapies, 2 [range, 1–4]), showing an overall response rate (ORR; primary efficacy measure) of 82 % (complete response [CR], 40 %; partial response, 42 %). In the 32 patients with complete 18F-FDG PET/CT data, 75 % achieved a complete metabolic response. Median duration of response was 1.6 years, 1-year progression-free survival was 67 %, and 3-year overall survival was 55 %. Main non-hematologic adverse events were nausea (69 %), fatigue (56 %), decreased appetite (42 %), constipation (38 %), diarrhea (36 %), vomiting (36 %), and decreased weight (31 %). Grade 3/4 neutropenia and lymphopenia occurred in 44 and 89 % of patients, respectively. ORR and CR rate compared favorably with single-agent ibrutinib (ORR, 67 %; CR, 23 %); bendamustine-rituximab is an effective therapy with manageable toxicity in relapsed/refractory MCL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mantle cell lymphoma (MCL) accounts for about 6–9 % of all new cases of non-Hodgkin lymphoma (NHL) in Europe and the USA [1, 2]. Most patients with MCL relapse after induction therapy followed by autologous stem cell transplant, usually with poor or short response to conventional chemotherapy [3]. In the relapsed/refractory setting, several novel therapies (bortezomib, ibrutinib, and lenalidomide) have been approved (three in the USA and two in Europe), and although these may lead to durable responses, in most cases, patients have transient partial responses and eventually show progression of disease. In addition, patients with relapsed/refractory MCL are either older (median age at initial diagnosis mid-late 60s) and/or carry comorbid conditions and therefore have typically limited options [4].
Bendamustine in combination with rituximab (B-R) has been shown to be an effective therapy with manageable toxicity in patients with relapsed/refractory indolent NHL and MCL [5–7] and in patients with untreated indolent NHL and MCL [8, 9]. Multiple ongoing clinical trials built on B-R backbone in combination with a number of targeted agents (e.g., lenalidomide, temsirolimus, ofatumumab, bortezomib, mitoxantrone, and ibrutinib) in B-cell NHL are currently underway [10, 11].
Though a small number of patients with MCL have been enrolled as part of the phase II clinical development of B-R, the purpose of the current study was to evaluate the efficacy and safety of B-R in a population of patients with relapsed/refractory MCL.
Methods
Study design and patient population
The current study was a 24-week, multicenter, open-label, single-arm, phase II clinical trial in men and women aged ≥18 years with relapsed or refractory CD20-positive B-cell MCL who had received ≤3 previous standard chemotherapy regimens. Relapsed disease was defined as progression after having achieved a complete response (CR) with a previous therapy but demonstrating recurrent disease >6 months after the last dose of therapy. Refractory disease was defined as failure to achieve a CR with previous therapy or progression within 6 months after achieving a CR.
Patients had histopathologically confirmed non-blastoid-type MCL; adequate hematologic function (unless abnormalities were related to lymphoma); serum creatinine of ≤2.0 mg/dL or creatinine clearance ≥30 mL/min; adequate hepatic function (alanine transaminase and aspartate transaminase levels ≤2.5 times the upper limit of normal and ≤1.5 times the upper limit of normal for total bilirubin [unless due to Gilbert’s disease]); bidimensionally measurable disease (≥1 lesion measuring ≥2.0 cm in a single dimension); Eastern Cooperative Oncology Group performance status ≤2; and an estimated life expectancy of ≥3 months. History of autologous stem cell transplantation was permitted.
Patients who had blastoid-type MCL or prior high-dose chemotherapy with allogeneic stem cell support were excluded from the study, as were those with other active malignancy within 3 years (with the exception of controlled prostate cancer without bone metastases, localized bladder cancer, cervical carcinoma in situ, and non-melanoma skin cancer). Patients requiring palliative radiation were to be withdrawn from the study because urgent radiotherapy was likely to signify progressive disease. Other exclusion criteria included the use of investigational agents, chemotherapy, or corticosteroids within 28 days (with the exception of corticosteroids that were chronically administered for indications other than lymphoma or lymphoma-related complications) and mitomycin C within 6 weeks.
All patients provided written informed consent, and the study was conducted in accordance with the Good Clinical Practice Consolidated Guideline approved by the International Conference on Harmonisation.
Drug administration
Bendamustine was administered as an intravenous (IV) infusion of 90 mg/m2 on days 1 and 2 of a 28-day cycle, and rituximab was administered as an IV infusion of 375 mg/m2 on day 1. The treatment period consisted of 6 cycles; however, patients could receive up to 8 cycles if they had not achieved CR and did not have disease progression.
Patients with an absolute lymphocyte count >5 × 109/L received rituximab (at the dose during cycle 1) across 3 days and bendamustine on days 3 and 4 in cycle 1. Analgesics/antipyretics were administered prior to each rituximab dose.
PET imaging data
18F-FDG PET/CT was performed at screening and 30 days following completion of therapy. Combined PET/CT units provided nearly simultaneous acquisition of both metabolic and anatomic data. Patients fasted 4–6 h prior to imaging with a target fasting glucose <150 mg/dL. Hydration during the uptake period was encouraged, with voiding prior to imaging. Each patient’s pre- and post-therapy imaging was performed from skull vertex through pelvis using the same instrument, with consistent arm positioning. All scans were centrally reviewed for consistent metabolic response grading using maximum standardized uptake value corrected to body weight and a five-point Deauville scale, with lesion uptake greater than liver considered as representing disease [12, 13].
Assessments
The primary efficacy measure was overall response rate (ORR) or CR plus partial response (PR) at the end of cycles 3 and 6; responses were determined using 2007 International Working Group (IWG) guidelines [12].
Secondary efficacy measures included progression-free survival (PFS), duration of response (DOR), overall survival (OS), and rate of conversion from 18F-FDG PET/CT positive to 18F-FDG PET/CT negative disease or complete metabolic response (CMR).
Safety measures included laboratory findings and adverse events (AEs) by National Cancer Institute Common Terminology Criteria for Adverse Events, version 3.0 criteria. All patients who received ≥1 dose of bendamustine were monitored during a minimum 3-year follow-up for disease progression or relapse, new lymphoma treatment, other malignancies, and/or death from any cause. Follow-up occurred every 4 months for 1 year and then every 6 months for the remainder of the follow-up period to document disease progression and survival. Disease progression was assessed by CT at every follow-up visit. The study ended when the last patient had been in follow-up for 3 years.
Statistical analysis
ORR and CR were calculated in all enrolled patients treated with ≥1 dose of B-R. Two-sided 95 % confidence intervals (CIs; 1-sided α of 5 %) of ORR and CR rates were based on exact binomial distributions. PFS, DOR, and OS were estimated by the Kaplan–Meier method.
To test the study hypothesis that B-R will result in an ORR ≥65 % (absolute increase of approximately 21 % in ORR from the historical level of 44 % for bortezomib in relapsed/refractory MCL), the original planned sample size was 52 patients, which would have provided a power of 90 % to reject the null hypothesis at a one-sided α of 5 %. However, study enrollment was terminated early by the sponsor for non-clinical reasons (business decision not to develop bendamustine further for this indication), which resulted in a smaller sample size and affected the statistical power.
Results
Patient disposition and demographics
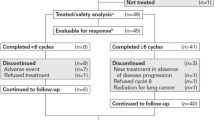
Forty-five patients were enrolled; all had received ≥1 dose of the study regimen and were evaluable for the safety analysis (Table 1). Three patients had received four prior lines of chemotherapy, but none of the deviations were considered to adversely affect the results.
Thirty-nine patients completed at least 6 planned treatment cycles, 1 patient completed 5 treatment cycles, no patient completed 4 treatment cycles, and 5 patients completed <4 treatment cycles. Seven patients discontinued study treatment early (two each in cycles 2 and 3, and one each in cycles 1, 5, and 7) due to consent withdrawal (n = 2; 1 each in cycles 1 and 2), disease progression (n = 3; 2 in cycle 3 and 1 in cycle 5), and AEs (n = 2; thrombocytopenia and hematochezia in the patient who completed 7 cycles; death due to myocardial infarction, pneumonia, and respiratory failure in another patient who completed 2 cycles).
Efficacy
At the assessment point of cycle 6, the ORR, the primary efficacy measure, was 82 % (two-sided 95 % CI, 68 to 92 %); the rates of CR and PR were 40 and 42 %, respectively (Table 2).
Median follow-up from the last date of treatment was approximately 1.6 years. Median PFS was 17.2 months (range, 0.03–45.37 months), and 1-year PFS was 67 %; median DOR was 18.9 months (range, 2.76–42.77 months) (Fig. 1). The rate of OS at 3 years of follow-up was 55 %.
Complete image-based metabolic datasets were available for 32 patients. The rate of PET conversion from positive to negative (CMR) for B-R was 75 % (24/32; Table 2; Fig. 2). At last follow-up among patients with CMR (n = 24), 16 were alive, 7 had died (4 from disease progression, 1 from “lymphoma,” 2 from other/unknown cause), and 1 was lost to follow-up. Among patients without CMR, 3 were alive and 15 had died. Kaplan–Meier estimates of OS demonstrated that CMR is a good predictor of survival (Fig. 3).
Complete metabolic response demonstrated by 18F-FDG PET/CT. Patient was a 63-year-old male, refractory to 2 prior regimens, beginning B-R treatment in April 2010. Baseline evaluation in March 2010 (top panels) was positive at numerous sites above and below the diaphragm (>6 lesions, Deauville 5, SUVmax 11.7). Following 6 B-R treatment cycles (last dose August 24, 2010), 18F-FDG PET/CT (bottom panels) was negative (0 positive lesions, Deauville 2, SUVmax 2.0) and the patient was graded as CR. 18F-FDG PET/CT 18-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography, B-R bendamustine in combination with rituximab, CR complete response, SUV max maximum standardized uptake value
Assessment of ORR by baseline characteristics was an exploratory analysis and showed that the 21 patients with relapsed MCL had an ORR of 90 % (CR, 76 %), and the 24 patients with MCL refractory to rituximab had an ORR of 75 % (CR, 21 %). By MCL International Prognostic Index (MIPI) score category, 24 patients had a score of ≤3 and an ORR of 92 % (CR, 58 %); 12 patients had a score of 4–5 and an ORR of 92 % (CR, 42 %; Fig. 4).
Dosing and dose intensities, delays, and reductions
The median overall cumulative dose was 1,080 mg/m2 (range, 180–1,524 mg/m2) for bendamustine and 2,253 mg/m2 (range, 388–3,120 mg/m2) for rituximab. The median absolute and relative dose intensities were 44 mg/m2/week (range, 16–47 mg/m2/week) and 98 % (range, 36–105 %) for bendamustine and 92 mg/m2/week (range, 68–98 mg/m2/week) and 99 % (range, 73–105 %) for rituximab, respectively. Eleven of 45 (24 %) patients required a dose reduction of bendamustine during any cycle, but no patient required a reduction in rituximab dose. Twenty-two patients had ≥1 dose delay with a median of 1 delay (range, 1–2). The most common reasons for dosage reductions/delays were neutropenia (n = 21) and thrombocytopenia (n = 19).
Adverse events
The most common nonhematologic treatment-emergent AEs (all grades, >30 %) were nausea (69 %), fatigue (56 %), decreased appetite (42 %), constipation (38 %), diarrhea (36 %), vomiting (36 %), and decreased weight (31 %). The most common grade 3/4 laboratory hematologic toxicities were lymphopenia (89 %), leukopenia, and neutropenia (44 % each; Table 3). The most common non-hematologic grade 3/4 AEs were hypokalemia, hypotension, muscular weakness (7 % each), and pneumonia (4 %; one additional case was grade 5; Table 3). Overall, 7 patients (16 %) developed 12 grade 3 infections—no grade 4 infections were reported; the most common were device-related and pneumonia (4 % each). Grade 3 opportunistic infections were reported in one patient who had toxoplasmosis (which was considered possibly related to the study drug treatment by the investigator) and in another patient who developed urosepsis (which was considered possibly related to the study drug treatment by the sponsor). Infusion-related reactions were all associated with rituximab (but considered unlikely to be or not associated with bendamustine), resolved with no residual effect, and occurred in four patients (grades 1–2, n = 3; grade 3, n = 1).
Serious AEs occurred in 18 patients; those occurring in ≥2 patients were pneumonia (n = 3), confusional state, or pleural effusion (n = 2 each). Three patients had AEs that led to withdrawal (myocardial infarction, pneumonia, and respiratory failure led to death in one patient; back pain and infusion-related reaction to rituximab led to discontinuation in one; and thrombocytopenia in one). Twenty-eight patients received hematopoietic growth factors (most commonly in cycles 3–5), and six patients received blood products.
Three patients died due to AEs during the study: one death due to myocardial infarction, pneumonia, and respiratory failure; one from myelodysplastic syndrome; and the other due to Burkitt’s lymphoma. These deaths were considered unlikely to be related or unrelated to B-R treatment.
Discussion
In the relapsed/refractory setting, patients with MCL have very few options due to age and/or comorbidities. Though several novel therapies have been approved over the last few years (three in the USA and two in Europe), most patients achieve transient PRs, illustrating the need for novel options in that setting [4]. The response rate to standard cytotoxics in relapsed/refractory MCL is usually poor and of short duration. Bendamustine has appeared over the last decade as an appealing option in that setting. Several studies in indolent NHL have shown promising results in patients with relapsed/refractory MCL [5–7, 14–16]. For example, two phase II studies of B-R in NHL included patients with relapsed MCL and found ORRs in the MCL subgroups of 75 and 92 % and CR rates of 50 and 59 % (including unconfirmed CR [CRu]) [5, 6]. Two retrospective analyses reported ORRs of 70 and 80 % and CR rates of 40 and 48 % in relapsed/refractory MCL [7, 17]. In addition, a retrospective analysis of 58 patients with relapsed/refractory MCL (median age, 71 years; >2/3 of patients with MIPI ≥4) treated with B-R, the ORR was 84 %, CR (plus CRu) was 53 %, and median PFS was 16 months, with lymphopenia, neutropenia, and thrombocytopenia as the most common grade 3/4 AEs [18]. Of note, although the comparator ORR was 44 %, single-agent bortezomib and lenalidomide were approved for relapsed/refractory MCL, with ORRs of 31 % (95 % CI, 24 to 39 %) and 26 % (95 % CI, 18 to 34 %), respectively [19, 20].
The goal of our study was to focus on a more homogenous population, including only relapsed/refractory MCL patients who received ≤3 prior therapies. For the 45 patients enrolled in this multicenter study, the median age was 70 years and close to half had MIPI ≥4 (Cell proliferation index Ki-67 and molecular marker SOX11, now known to have prognostic significance, were not collected during our study). The ORR assessed by IWG 2007 criteria was 82 % and treatment was manageable as shown by the limited number of dose delays and reductions. The median DOR was 18.9 months and the 1-year PFS 67 %. Median follow-up from the last date of treatment was about 1.6 years.
Furthermore, our study included prespecified 18F-FDG PET/CT analysis, which was not commonly used in studies using B-R in MCL. Though the role of PET scan in MCL is not as established as in diffuse large B-cell lymphoma or Hodgkin lymphoma, several studies have suggested that negative PET post chemotherapy correlated with a better outcome [21, 22]. In our study, complete image-based metabolic datasets were available for 32 patients; the CMR rate (PET-negative CR) was 75 % (24/32; Table 2; Fig. 2). During the last follow-up among patients with PET-negative CR (n = 24), 16 were alive, 7 had died, and 1 was lost to follow-up. Among patients without CMR, 3 were alive and 15 had died. Though numbers remain small, the subset analysis based on baseline characteristics showed very promising results. As shown in Fig. 4, high ORRs were seen across the board in relapsed/refractory patients, though lesser CR rates (more PRs) were seen in refractory patients or in those with MIPI of 5. The toxicity profile in our study was within expectations of known bendamustine-associated myelotoxicity and lymphopenia.
The safety profile, particularly in elderly MCL patients, has led B-R to become a favorite platform to build up for combination studies. Phase II studies of B-R plus another agent in relapsed/refractory MCL showed frequently promising ORRs and high CR rate. For example, B-R was combined with bortezomib [14], mitoxantrone [15], and cytarabine [23]. In the latter study, half of the patients had relapsed/refractory MCL, the other half untreated; in both cases, high response rate and very durable response make the rituximab–bendamustine–cytarabine regimen attractive in elderly patients with MCL. Multiple ongoing studies are looking at integrating other chemotherapies (e.g., B-R plus bortezomib and dexamethasone) and biological agents (e.g., B-R plus ibrutinib or lenalidomide) in the frontline or relapsed/refractory setting either in combination or sequentially as maintenance therapy, which will likely take a larger role in the management of MCL patients [24–27]. Currently, there is an ongoing phase 3 clinical trial that is evaluating B-R with the Bruton’s tyrosine kinase inhibitor (BTK) ibrutinib in newly diagnosed MCL [27].
Future directions in the relapsed/refractory setting might be to combine B-R with the BTK inhibitor ibrutinib, which as a single agent has shown the most activity in MCL compared with bortezomib, lenalidomide, and temsirolimus [28–31], and to possibly reinitiate therapy with ibrutinib at the first sign of rising minimal residual disease or alternatively, maintain response with ibrutinib. With respect to B-R, our efficacy and safety results compare favorably with those of single-agent ibrutinib, which demonstrated an ORR of 67 % and a median DOR of 17.5 months, with a high rate of serious AEs (63 %) [32]. Although both studies were restricted to the relapsed/refractory setting, the difference in response may be related to differences in the patient population.
New strategies are needed in relapsed/refractory MCL, particularly in elderly or in patients with comorbidities. Bendamustine as a single agent had shown promising activity in indolent NHL and MCL, providing a new option in combination with rituximab. Our study with B-R confirms high ORR (82 %) and PET-negative CR rate (75 %) in heavily pretreated relapsed/refractory MCL patients, including patients with high-risk MIPI. The responses were also durable (median DOR of 1.6 years) with a manageable safety profile, providing a new backbone for multiple ongoing studies, either in the frontline or relapsed/refractory setting.
References
Dreyling M, Geisler C, Hermine O et al (2014) Newly diagnosed and relapsed mantle cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):iii83–iii92
The Non-Hodgkin’s Lymphoma Classification Project (1997) A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. Blood 89(11):3909–3918
Goy A, Kahl B (2011) Mantle cell lymphoma: the promise of new treatment options. Crit Rev Oncol Hematol 80(1):69–86
Ruan J, Coleman M, Leonard JP (2009) Management of relapsed mantle cell lymphoma: still a treatment challenge. Oncology (Williston Park) 23(8):683–690
Rummel MJ, Al-Batran SE, Kim SZ et al (2005) Bendamustine plus rituximab is effective and has a favorable toxicity profile in the treatment of mantle cell and low-grade non-Hodgkin’s lymphoma. J Clin Oncol 23(15):3383–3389
Robinson KS, Williams ME, van der Jagt RH et al (2008) Phase II multicenter study of bendamustine plus rituximab in patients with relapsed indolent B-cell and mantle cell non-Hodgkin’s lymphoma. J Clin Oncol 26(27):4473–4479
Rigacci L, Puccini B, Cortelazzo S et al (2012) Bendamustine with or without rituximab for the treatment of heavily pretreated non-Hodgkin’s lymphoma patients: a multicenter retrospective study on behalf of the Italian Lymphoma Foundation (FIL). Ann Hematol 91(7):1013–1022
Rummel MJ, Niederle N, Maschmeyer G et al (2013) Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet 381(9873):1203–1210
Flinn IW, van der Jagt RH, Kahl BS et al (2014) Randomized trial of bendamustine-rituximab or R-CHOP/R-CVP in first-line treatment of indolent NHL or MCL: the BRIGHT study. Blood 123(19):2944–2952
Chang JE, Kahl BS (2012) Bendamustine: more ammunition in the battle against mantle cell lymphoma. Leuk Lymphoma 53(7):1249–1250
van der Jagt R, Laneuville P, MacDonald D, Stewart D, Christofides A, Sehn LH (2012) A Canadian perspective on bendamustine for the treatment of chronic lymphocytic leukemia and non-Hodgkin lymphoma. Curr Oncol 19(3):160–168
Cheson BD, Pfistner B, Juweid ME et al (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25(5):579–586
Meignan M, Gallamini A, Meignan M, Gallamini A, Haioun C (2009) Report on the First International Workshop on Interim-PET-scan in lymphoma. Leuk Lymphoma 50(8):1257–1260
Friedberg JW, Vose JM, Kelly JL et al (2011) The combination of bendamustine, bortezomib, and rituximab for patients with relapsed/refractory indolent and mantle cell non-Hodgkin lymphoma. Blood 117(10):2807–2812
Weide R, Hess G, Köppler H et al (2007) High anti-lymphoma activity of bendamustine/mitoxantrone/rituximab in rituximab pretreated relapsed or refractory indolent lymphomas and mantle cell lymphomas: a multicenter phase II study of the German Low Grade Lymphoma Study Group (GLSG). Leuk Lymphoma 48(7):1299–1306
Rummel MJ, Balser C, Kaiser U et al (2014) Bendamustine plus rituximab versus fludarabine plus rituximab in patients with relapsed follicular, indolent, or mantle cell lymphomas—8-year follow-up results of the randomized phase III study NHL 2-2003 on behalf of the StiL (Study Group Indolent Lymphomas, Germany). Blood 124(21):145
Warsch S, Hosein PJ, Maeda LS, Alizadeh AA, Lossos IS (2012) A retrospective study evaluating the efficacy and safety of bendamustine in the treatment of mantle cell lymphoma. Leuk Lymphoma 53(7):1299–1305
García-Noblejas A, Martínez Chamorro C, Navarro Matilla B et al (2014) Bendamustine as salvage treatment for patients with relapsed or refractory mantle cell lymphoma patients: a retrospective study of the Spanish experience. Ann Hematol 93(9):1551–1558
Kane RC, Dagher R, Farrell A et al (2007) Bortezomib for the treatment of mantle cell lymphoma. Clin Cancer Res 13(18 Pt 1):5291–5294
(2013) Revlimid [package insert]. Celgene Corporation; Summit, NJ
Mato AR, Svoboda J, Feldman T et al (2012) Post-treatment (not interim) positron emission tomography-computed tomography scan status is highly predictive of outcome in mantle cell lymphoma patients treated with R-HyperCVAD. Cancer 118(14):3565–3570
Hosein PJ, Pastorini VH, Paes FM et al (2011) Utility of positron emission tomography scans in mantle cell lymphoma. Am J Hematol 86(10):841–845
Visco C, Finotto S, Zambello R et al (2013) Combination of rituximab, bendamustine, and cytarabine for patients with mantle-cell non-Hodgkin lymphoma ineligible for intensive regimens or autologous transplantation. J Clin Oncol 31(11):1442–1449
Gressin R, Callanan M, Daguindau N et al (2014) Frontline therapy with the Ribvd regimen elicits high clinical and molecular response rates and long PFS in elderly patients mantle cell lymphoma (MCL); final results of a prospective phase II trial by the Lysa group. Blood 124(21):148
Campo E, Rule S (2015) Mantle cell lymphoma: evolving management strategies. Blood 125(1):48–55
Burger JA (2014) Bruton’s tyrosine kinase (BTK) inhibitors in clinical trials. Curr Hematol Malig Rep 9(1):44–49
A study of the Bruton’s tyrosine kinase inhibitor ibrutinib given in combination with bendamustine and rituximab in patients with newly diagnosed mantle cell lymphoma. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT01776840?term=ibrutinib+AND+phase+3+AND+mantle+cell+lymphoma&rank=2. Accessed 21 May 2015
Wang ML, Rule S, Martin P et al (2013) Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med 369(6):507–516
Fisher RI, Bernstein SH, Kahl BS et al (2006) Multicenter phase II study of bortezomib in patients with relapsed or refractory mantle cell lymphoma. J Clin Oncol 24(30):4867–4874
Goy A, Sinha R, Williams ME et al (2013) Single-agent lenalidomide in patients with mantle-cell lymphoma who relapsed or progressed after or were refractory to bortezomib: phase II MCL-001 (EMERGE) study. J Clin Oncol 31(29):3688–3695
Hess G, Herbrecht R, Romaguera J et al (2009) Phase III study to evaluate temsirolimus compared with investigator’s choice therapy for the treatment of relapsed or refractory mantle cell lymphoma. J Clin Oncol 27(23):3822–3829
Wang M, Rule S, Martin P et al (2014) Single-agent ibrutinib demonstrates safety and durability of response at 2 years follow-up in patients with relapsed or refractory mantle cell lymphoma: updated results of an international, multicenter, open-label phase 2 study. Blood 124(21):445
Acknowledgments
This research was sponsored by and conducted by Teva Branded Pharmaceutical Products R&D, Inc., Frazer, PA. Statistical support was provided by Ling Chen, PhD (Teva Branded Pharmaceutical Products R&D, Inc.). Medical writing assistance (including literature searches, editing and fact checking, graphic support, and at the request of and with guidance from the authors, assistance with the preparation of the outline and drafting of this manuscript) was provided by The Curry Rockefeller Group, LLC, Tarrytown, NY, and was funded by Teva Branded Pharmaceutical Products R&D, Inc. (Frazer, PA). Teva provided a full review of the article. We wish to thank all the site investigators who contributed to this study and their staff for their support, as well as all the patients and their families for their dedication to research and this study. A special thank you is also given to Glen Davis and Coleen Myers from Teva Branded Pharmaceutical Products R&D, Inc., for their complete dedication in ensuring the data collection was available adequately.
Conflict of interest
The authors received research funding for this study from Teva Pharmaceutical Products R&D, Inc. MSC has served as consultant to Teva Pharmaceuticals and Mundipharma, and has received an honorarium for serving as an educational meeting chairman for Mundipharma. AG has served as a member of the Board of Directors/advisory committees of Pharmacyclics, JNJ, Celgene, and Millennium; participated in the speakers’ bureaus of Pharmacyclics, JNJ, Celgene, and Millennium; and served as a consultant for and received honoraria from Celgene. He has also received research funding for clinical trials through his institution. DL and DAG declare that they have no conflict of interest. MCM is an employee and shareholder of Teva, and has owned stock/held an ownership interest in Janssen. RHvdJ has served as a consultant for, participated in speakers’ bureaus for, and has received honoraria and research funding from Teva Pharmaceuticals and Lundbeck.
Research involving human participants and/or animals
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Czuczman, M.S., Goy, A., Lamonica, D. et al. Phase II study of bendamustine combined with rituximab in relapsed/refractory mantle cell lymphoma: efficacy, tolerability, and safety findings. Ann Hematol 94, 2025–2032 (2015). https://doi.org/10.1007/s00277-015-2478-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2478-9