Abstract
Uremia is associated with platelet dysfunction and can cause a bleeding tendency resulting in a major bleeding event after an invasive procedure or surgery that may be aggravated by antiplatelet agents. We prospectively investigated the potential of desmopressin to improve platelet dysfunction and to lower bleeding risk after emergent invasive procedures in uremic patients taking antiplatelet drugs. Twenty-three patients were enrolled with a mean age of 60.2 ± 11.7 years. Baseline blood urea nitrogen and creatinine were 70.5 ± 29.4 and 10.02 ± 4.52 mg/dL, respectively. Twenty-one patients took aspirin. All patients were infused with desmopressin before their invasive procedures, which were a central catheter insertion for emergent hemodialysis in 13 patients, percutaneous nephrostomy in 7 patients, and angiography through arm or leg vessels in 3 patients. After desmopressin infusion, both the hematocrit and platelet count were slightly decreased without changes in prothrombin time or activated partial thrombin time. Collagen/epinephrine-closure time was significantly shortened from 252.7 ± 40.7 to 144.6 ± 51.0 s (p < 0.001). There were minimal bleeding in 20 patients and mild bleeding in 3 patients. None experienced severe bleeding event or required additional intervention for bleeding control. There were no adverse events including the decrease of serum sodium concentration. In conclusion, a single infusion of desmopressin before invasive procedures in uremic patients on antiplatelet drugs appeared to be well tolerated and improved platelet dysfunction measured by collagen/epinephrine-closure time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bleeding associated with acquired platelet dysfunction is a major cause of morbidity and mortality in uremic patients [1]. The pathogenesis of platelet dysfunction is multifactorial, including decreased platelet-vessel wall and platelet-platelet interactions [2]. Because diabetes and hypertension are common causes of chronic kidney disease (CKD), most CKD patients have concomitant cardiovascular or cerebrovascular diseases, resulting in a higher necessity of taking antiplatelet agents for secondary prevention. If uremic patients undergo surgical or other invasive procedures that may cause bleeding events, the cessation of antiplatelet therapy may be one of the possible options after consideration for the risks and benefits. Although low-dose aspirin alone does not substantially increase the risk of clinically important bleeding after invasive procedures, a 7- to 10-day interval is recommended in a healthy population between the last dose and a procedure because of irreversible effects on cyclooxygenase inhibition [3]. In emergency situations, however, delaying procedures in order to decrease the possibility of hemorrhagic complications is realistically impossible, which can be further exacerbated in uremic conditions with an underlying platelet dysfunction.
Previously, skin bleeding time was the best predictor of clinical bleeding [4], but this estimate is highly operator-dependent and poorly reproducible, indicating disadvantageous characteristics for screening primary hemostasis [5, 6]. In vitro closure time (IVCT) using a platelet function analyzer (PFA-100) is an alternative test that has shown utility in assessing abnormal primary hemostasis and monitoring antiplatelet therapy, both of which were also proven in dialysis patients [7]. Desmopressin (1-deamino-8-d-arginine vasopressin, DDAVP) is a synthetic analogue of the antidiuretic hormone vasopressin originally designed for the treatment of diabetes insipidus [8]. Owing to its hemostatic properties, desmopressin has been used prior to surgery in patients with a major risk of bleeding [9]. DDAVP shortens the skin bleeding time and significantly improves platelet dysfunction as assessed by IVCT in uremic patients [10, 5]. However, its efficacy in CKD patients taking antiplatelet agents, who have both uremia and altered platelet function due to medications, remains unknown. We therefore designed our current prospective trial to evaluate the ability of DDAVP to improve platelet dysfunction and to lower the risk of post-procedural bleeding events in uremic patients taking antiplatelet drugs.
Methods
Study design and population
This study was a single-center, prospective, observational clinical trial performed at Asan Medical Center in Seoul, South Korea, and is registered at http://clinicaltrials.gov (NCT01841515). Eligible patients were 20 to 75 years of age with stage 5 CKD who required one or more antiplatelet medications. We enrolled patients from May 1, 2011 to April 31, 2014. We selected patients whose treatment required undergoing emergent invasive procedures, such as a central catheter insertion for emergent hemodialysis, percutaneous nephrostomy, or angiography via the arm or leg. Patients with chronic liver disease, infectious disease, acute coronary syndrome, hemophilia, nephrogenic diabetes insipidus, or allergy against desmopressin were excluded. The Institutional Review Board at Asan Medical Center approved the registered protocol, and written informed consents were obtained from all patients.
Study protocol
Patients enrolled in this study promptly stopped taking antiplatelet agents, including aspirin, clopidogrel, cilostazol, or beraprost and were infused with 0.3 μg/kg DDAVP (Minirin) in 100 ml of normal saline over 30 min before their invasive procedures. There was no control group in this study, in which DDAVP was not administered, as we considered that it would be unethical not to provide DDAVP to uremic patients waiting for invasive procedures, considering its hemostatic function and potential efficacy. Baseline blood sampling was obtained immediately before the DDAVP infusion. Before and 1 h after the infusion of DDAVP, we measured a complete blood count, prothrombin time (PT), activated partial thrombin time (aPTT), and in vitro collagen/epinephrine-closure time (CEPI-CT). PT was measured using Neoplastine CL Plus (Diagnostica Stago, Asnières-sur-Seine, France), and aPTT was assessed by a STA-PTTA (Diagnostica Stago). The CEPI-CT was measured with a PFA-100 device (Dade Behring, Marburg, Germany) which functionally resembles vessels. A blood sample was aspirated from the sample reservoir through a capillary under a constant negative pressure and contacted with a membrane coated with collagen and epinephrine (CEPI). At an aperture in the membrane mimicking the injured vessel wall, platelet aggregation occurs by this biochemical reaction, resulting in the formation of a plug. Closure time (CT), the time taken to occlude the aperture and to interrupt blood flow, was recorded by the PFA-100 device. The reference range for CEPI-CT was 82–182 s on the basis of previous study data conducted in 120 healthy individuals at our center [11]. The invasive procedures were performed by experienced interventional radiologists. Severity of bleeding after an invasive procedure was classified into grades 1, 2, and 3. Grade 1 was defined as no additional surgical gauze change associated with bleeding, grade 2 as a change of one or two surgical gauze pads, and grade 3 as changes of more than three surgical gauze pads or the need of manual compression for bleeding control.
Statistical analysis
Statistical analyses were performed using commercially available software (IBM SPSS Statistics for Windows, version 21.0, Armonk, NY). The results are provided as the mean ± standard deviation. Data obtained at baseline and 1 h after DDAVP infusion were analyzed with a Wilcoxon signed-rank test. Differences were considered statistically significant at a threshold of p < 0.05.
Results
A total of 23 patients with uremia were enrolled in this trial. The mean patient age was 60.2 ± 11.7 years, and there were 16 (69.6 %) male patients. Twenty-one (91.3 %) patients took aspirin as an antiplatelet agent, and aspirin plus clopidogrel was used in six (26.1 %) patients. Triple combination therapy with aspirin, clopidogrel, and beraprost was observed in one (4.3 %) patient. Beraprost alone was administered in two (8.7 %) patients. Central catheter insertion via right internal jugular vein for emergent hemodialysis was performed in 13 (56.5 %) patients, who consisted of 11 patients for tunnel catheter and two patients for non-tunneled catheter as an invasive procedure. Seven (30.4 %) patients underwent percutaneous nephrostomy or biopsy at any site, and angiography through arm or leg vessels was conducted in three (13.0 %) patients. The mean blood urea nitrogen (BUN) level was 70.5 ± 29.4 mg/dL and the mean creatinine was 10.02 ± 4.52 mg/dL indicating an estimated glomerular filtration rate (eGFR) of 6.10 ± 3.33 mL/min/1.73 m2. The other clinical characteristics of the patients are summarized in Table 1.
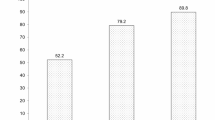
Among the laboratory parameters before and after DDVAP infusion, hematocrit was decreased from 25.7 ± 4.1 to 24.5 ± 3.2 % (p = 0.042), and platelet count was similarly decreased from 235.4 ± 40.7 × 109 to 225.3 ± 86.0 × 109/L (p = 0.086). There were no changes in PT or aPTT. CEPI-CT was significantly shortened after DDVAP infusion from 252.7 ± 40.7 to 144.6 ± 51.0 s (p < 0.001). Serum sodium concentration in 24 h after DDAVP infusion was not changed compared with that before DDAVP infusion (134.96 ± 4.9 vs. 133.65 ± 5.0, respectively, p = 0.117). In ten patients who did not undergo central catheter insertion and hemodialysis, the difference of serum sodium concentration was also not observed at before and after DDAVP infusion (134.0 ± 3.3 vs. 134.4 ± 4.6, p = 0.613). Parameters are summarized in detail in Table 2.
No severe bleeding events (grade 3) were observed, and no patients underwent additional interventions for bleeding control. Twenty (87.0 %) patients experienced minimal bleeding (grade 1), and mild bleeding (grade 2) was found in three (13.0 %) patients (Table 3). There were no significant side effects observed during or after DDAVP infusion.
Discussion
The risk of uremic hemorrhage has decreased with the advent of modern dialysis techniques that eliminate uremic toxins and the use of erythropoietin to correct anemia, but complications related to bleeding diathesis still limit invasive procedures and surgery in patients with uremia [12]. Despite the number of advanced CKD patients who are taking antiplatelet agents that can significantly increase the bleeding risk and who may experience invasive procedures, recommendations for reversal of platelet function remain uncertain. Thus, we here focused on demonstrating the efficacy of DDAVP in uremic patients to improve platelet dysfunction and to reduce post-procedural bleeding risk.
It is well-established that uremia increases the risk for bleeding complications for several reasons, including comorbid conditions predisposing to bleeding, medications that affect hemostasis, and bleeding diathesis due to uremia, which mainly results from the crucially important impairment of platelet hemostasis [12, 13]. There is still no unifying pathophysiologic mechanism to explain the platelet defects, but they are partly associated with several uremic toxins, such as urea, creatinine, phenol, phenolic acids, or guanidinosuccinic acid (GSA) [12, 14, 15]. Several therapies aimed at correcting the coagulation defect include red blood cell transfusion, dialysis, cryoprecipitate, estrogen, and DDAVP [15].
Despite the various clinical indications for the use of DDAVP, the mechanism by which this hormone analogue improves bleeding tendency remains incompletely understood [5, 8]. DDAVP increases plasma concentrations of von Willebrand factor (VWF) and factor VIII (FVIII), which may underlie its hemostatic effect [8, 9]. These changes related to clotting action have also been in the uremic condition. Lee et al. reported that VWF and FVIII are significantly increased after infusion of DDAVP, indicating that this treatment could improve platelet dysfunction in patients with uremia [5]. Administration of DDAVP also shortens the bleeding time in uremia, suggesting a temporary correction of bleeding time to prevent uremic bleeding complications [10]. Likewise, DDAVP has been used in a number of inherited and acquired hemorrhagic conditions and in patients undergoing percutaneous procedures and surgery [8, 9, 16]. Because a randomized controlled study design could be unethical considering the effectiveness of DDAVP in high-risk patients, we chose an observational clinical trial with single treatment group.
Besides its hemostatic properties, DDAVP is relatively inexpensive, is safer than blood products because it has no possibility of transmitting blood-borne viruses, and has the advantage of minimizing the exposure to alloantigens in patients who are anticipating kidney transplantation [8]. In contrast, cryoprecipitate can shorten bleeding time in uremia; however, it is rarely used in CKD patients because it is derived from blood and carries the risk of infection. Although serious side effects are uncommon, DDAVP is reported to cause facial flushing, nausea, headache, tachycardia, thrombocytopenia, water retention, and hyponatremia, which are almost always mild and transient [2, 8]. In our current study, almost the same serum sodium concentrations before and after DDAVP infusion were observed, and there was no other significant side effect associated with DDAVP. Similar results have been reported in uremic patients [5]. In study patients who had poor renal function with stage 5 CKD, subsequent hyponatremia mainly caused by water retention did not happen, indicating that the use of DDAVP may be safe in patients with near end-stage renal disease.
Previously, bleeding time (BT) was the most commonly used test for measurement of overall platelet function. However, the usefulness of BT is questionable because it is invasive and highly operator-dependent [6, 17]. CEPI-CT measured by a PFA-100 machine is an in vitro test that could substitute for BT in the diagnosis of primary hemostasis defects [17]. Recent studies have shown the utility of CEPI-CT in patients with uremia or taking antiplatelet agents [7, 18, 19]. Moreover, CEPI-CT is significantly associated with the severity of bleeding [17], and its prolongation was observed in patients with aspirin ingestion despite a normal BT [6].
Antiplatelet agents including aspirin and clopidogrel are commonly used for primary prevention of cardiovascular or cerebrovascular diseases and after a percutaneous coronary intervention with a stent. Aspirin alone is not a significant problem for the majority of surgical procedures, although there can be a modest increase in blood loss [20]. Similarly, continuing to take antiplatelet agents before a native renal biopsy did not increase the rate of major bleeding complications despite the observation that a significantly higher proportion of patients experienced a >1.0 g/dL reduction in hemoglobin after the biopsy [21]. Because there is no specific antidote for antiplatelet agents, protocols for their reversal in the setting of acute intracranial hemorrhage have proposed platelet transfusion and/or DDAVP infusion [22]. Although the clinical utility of DDAVP has not been fully assessed, several studies suggest that it can accelerate the normalization of in vitro platelet dysfunction induced by glycoprotein IIb/IIIa inhibitors and aspirin and can antagonize antiplatelet activities in healthy subjects [23–25]. However, the effects of antiplatelet agents are quite different in patients with uremia. Aspirin prolongs BT in uremic patients compared to healthy controls [26]. Aspirin and clopidogrel combination therapy is associated with a significantly increased risk of bleeding in hemodialysis patients [27].
After DDAVP infusion, both the hematocrit and platelet count were slightly decreased, showing statistical significance in the hematocrit (p = 0.042). However, because the absolute difference of hematocrit level was very small, about 1.2 % on average, clinical meanings remain unclear. Desmopressin has been shown to shorten the prolonged aPTT by the increase of factor VIII [5, 8]. However, we observed no decrease of aPTT together with maintained PT level. These results are similar to those of a previous study performed in uremic patients not taking antiplatelet agents [5].
In our present trial, we evaluated the effect of DDAVP to improve platelet dysfunction by measuring CEPI-CT following DDAVP treatment and to decrease the risk of post-procedure bleeding complications in uremic patients with antiplatelet medications who required an emergent invasive procedure, primarily central catheter insertion for hemodialysis. DDAVP administration significantly decreased CEPI-CT followed by no major bleeding events. There has been no published evidence on the effectiveness of DDAVP in uremic patients with antiplatelet drugs. To the best of our knowledge, our current study is the first to demonstrate that DDAVP accelerates normalization of platelet dysfunction induced by both antiplatelet agents and uremia, suggesting the possibilities that this pretreatment may lead to a low rate of bleeding events after invasive procedures in uremic patients.
There are several limitations to this study. First, this trial was designed as a single treatment group without controls in spite of its prospective observational method. As shown above, DDAVP can decrease the risk of bleeding in patients with uremia or antiplatelet agents. We did not assign patients to a control group without DDAVP based on ethical considerations. Second, a relatively small number of patients were enrolled. There are no clinical data on this issue, so we had planned to conduct our study with 20 patients, similar to a pilot study. Third, we did not check the levels of coagulation factors, such as VWF and FVIII whose plasma concentrations can be increased by DDAVP treatment. Fourth, various invasive procedures and combinations of antiplatelet agents which could have different bleeding risks were included. Fifth, prolonged CEPI-CT can result from a low hematocrit which was observed in our results [5, 18]. However, CEPI-CT was significantly decreased along with decrease of hematocrit following DDAVP infusion, indicating the change of CEPI-CT was not associated with hematocrit.
In conclusion, our results showed that DDAVP can improve platelet dysfunction measured by CEPI-CT in patients with uremia and current antiplatelet agents. These findings suggest that DDAVP pretreatment before invasive procedures should be considered in uremic patients taking antiplatelet drugs with prolonged CEPI-CT, with the expectation to reduce blood complication and the need for unnecessary blood transfusion. In addition, these results will be able to give beneficial information for preoperative management in uremic patients. Additional large-scale studies with a proper control group are needed to more fully evaluate the advantages of DDAVP.
References
Horl WH (2010) Other blood and immune disorders in chronic kidney disease. In: Floege J, Johnson RJ, Feehally J (eds) Comprehensive clinical nephrology, 4th edn. Elsevier, St. Louis, p 959–968
Remuzzi G, Galbusera M, Boccardo P (2009) Disorders on hemostasis in dialysis patients. In: Henrich WL (ed) Principles and practice of dialysis, 4th edn, p 489–498
Baron TH, Kamath PS, McBane RD (2013) Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med 368:2113–2124. doi:10.1056/NEJMra1206531
Mattix H, Singh AK (1999) Is the bleeding time predictive of bleeding prior to a percutaneous renal biopsy? Curr Opin Nephrol Hypertens 8:715–718
Lee HK, Kim YJ, Jeong JU, Park JS, Chi HS, Kim SB (2010) Desmopressin improves platelet dysfunction measured by in vitro closure time in uremic patients. Nephron Clin Pract 114:c248–c252
Francis J, Francis D, Larson L, Helms E, Garcia M (1999) Can the Platelet Function Analyzer (PFA)-100 test substitute for the template bleeding time in routine clinical practice? Platelets 10:132–136. doi:10.1080/09537109976194
Zupan IP, Sabovic M, Salobir B, Ponikvar JB, Cernelc P (2003) Utility of in vitro closure time test for evaluating platelet-related primary hemostasis in dialysis patients. Am J kidney Dis Off J Natl Kidney Found 42:746–751
Franchini M (2007) The use of desmopressin as a hemostatic agent: a concise review. Am J Hematol 82:731–735. doi:10.1002/ajh.20940
Manno C, Bonifati C, Torres DD, Campobasso N, Schena FP (2011) Desmopressin acetate in percutaneous ultrasound-guided kidney biopsy: a randomized controlled trial. Am J kidney Dis Off J Natl Kidney Found 57:850–855. doi:10.1053/j.ajkd.2010.12.019
Mannucci PM, Remuzzi G, Pusineri F et al (1983) Deamino-8-D-arginine vasopressin shortens the bleeding time in uremia. N Engl J Med 308:8–12
Cho YU, Jang S, Park CJ, Chi HS (2008) Variables that affect platelet function analyzer-100 (PFA-100) closure times and establishment of reference intervals in Korean adults. Ann Clin Lab Sci 38:247–253
Boccardo P, Remuzzi G, Galbusera M (2004) Platelet dysfunction in renal failure. Semin Thromb Hemost 30:579–589. doi:10.1055/s-2004-835678
Sohal AS, Gangji AS, Crowther MA, Treleaven D (2006) Uremic bleeding: pathophysiology and clinical risk factors. Thromb Res 118:417–422
Ho SJ, Gemmell R, Brighton TA (2008) Platelet function testing in uraemic patients. Hematology 13:49–58. doi:10.1179/102453308X315834
Kaw D, Malhotra D (2006) Platelet dysfunction and end-stage renal disease. Semin Dial 19:317–322
Koscielny J, von Tempelhoff GF, Ziemer S et al (2004) A practical concept for preoperative management of patients with impaired primary hemostasis. Clin Appl Thromb Hemost Off J Int Acad Clin Appl Thromb Hemost 10:155–166
Podda GM, Bucciarelli P, Lussana F, Lecchi A, Cattaneo M (2007) Usefulness of PFA-100 testing in the diagnostic screening of patients with suspected abnormalities of hemostasis: comparison with the bleeding time. J Thromb Haemost JTH 5:2393–2398. doi:10.1111/j.1538-7836.2007.02752.x
Escolar G, Cases A, Vinas M et al (1999) Evaluation of acquired platelet dysfunctions in uremic and cirrhotic patients using the platelet function analyzer (PFA-100): influence of hematocrit elevation. Haematologica 84:614–619
Crescente M, Di Castelnuovo A, Iacoviello L, Vermylen J, Cerletti C, de Gaetano G (2008) Response variability to aspirin as assessed by the platelet function analyzer (PFA)-100. A systematic review. Thromb Haemost 99:14–26. doi:10.1160/TH07-08-0530
Schulman S (2012) Pharmacologic tools to reduce bleeding in surgery. Hematol Educ Prog Am Soc Hematol Am Soc Hematol Educ Prog 2012:517–521. doi:10.1182/asheducation-2012.1.517
Mackinnon B, Fraser E, Simpson K, Fox JG, Geddes C (2008) Is it necessary to stop antiplatelet agents before a native renal biopsy? Nephrol Dial Transplant Off Publ Eur Dial Transplant Assoc Eur Ren Assoc 23:3566–3570. doi:10.1093/ndt/gfn282
Campbell PG, Sen A, Yadla S, Jabbour P, Jallo J (2010) Emergency reversal of antiplatelet agents in patients presenting with an intracranial hemorrhage: a clinical review. World Neurosurg 74:279–285. doi:10.1016/j.wneu.2010.05.030
Ranucci M, Nano G, Pazzaglia A, Bianchi P, Casana R, Tealdi DG (2007) Platelet mapping and desmopressin reversal of platelet inhibition during emergency carotid endarterectomy. J Cardiothorac Vasc Anesth 21:851–854. doi:10.1053/j.jvca.2007.05.009
Leithauser B, Zielske D, Seyfert UT, Jung F (2008) Effects of desmopressin on platelet membrane glycoproteins and platelet aggregation in volunteers on clopidogrel. Clin Hemorheol Microcirc 39:293–302
Reiter RA, Mayr F, Blazicek H et al (2003) Desmopressin antagonizes the in vitro platelet dysfunction induced by GPIIb/IIIa inhibitors and aspirin. Blood 102:4594–4599. doi:10.1182/blood-2002-11-3566
Livio M, Benigni A, Vigano G, Mecca G, Remuzzi G (1986) Moderate doses of aspirin and risk of bleeding in renal failure. Lancet 1:414–416
Kaufman JS, O’Connor TZ, Zhang JH et al (2003) Randomized controlled trial of clopidogrel plus aspirin to prevent hemodialysis access graft thrombosis. J Am Soc Nephrol JASN 14:2313–2321
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, J.H., Baek, C.H., Min, J.Y. et al. Desmopressin improves platelet function in uremic patients taking antiplatelet agents who require emergent invasive procedures. Ann Hematol 94, 1457–1461 (2015). https://doi.org/10.1007/s00277-015-2384-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2384-1