Abstract
Previous randomized trials have demonstrated that rituximab maintenance (R-maintenance) can prolong time to progressive disease in patients with follicular lymphoma (FL). The phase IIIb MAXIMA study (NCT00430352) was a large prospective evaluation of R-maintenance in a daily care setting. The primary objective was safety. Secondary objectives included progression-free survival, overall survival, time to next lymphoma treatment, and partial response (PR) to complete response/unconfirmed (CR/CRu) conversion rate. Patients (n = 545) with first-line or relapsed FL who responded to 8 cycles of rituximab-based induction received R-maintenance every 2 months for 2 years. At study entry, 380 patients had CR or CRu, and 165 had PR. The median age was 57.0 years. The most common non-hematologic adverse events (AEs, excluding infusion-related reactions) were cough (9.9 % of patients), fatigue (7.5 %), nasopharyngitis (7.1 %), back pain (6.5 %), diarrhea (6.9 %), arthralgia (6.0 %), headache and hypertension (5.2 % each), and pyrexia (5.1 %). The majority of AEs were grade 1 or 2. Grade 3, 4, and 5 infections occurred in 21 (3.9 %), 2 (0.4 %), and 1 (0.2 %) patient, respectively. Fifty-one hematologic AEs occurred in 6.6 % (n = 35) of patients. Grade 3/4 prolonged neutropenia and hypogammaglobulinemia occurred in 13 (2.4 %) and 5 (0.9 %) patients, respectively. All cases of prolonged neutropenia or hypogammaglobulinemia were manageable and resolved. Fast infusion did not alter the safety profile. Efficacy was comparable with results from previous trials. R-maintenance is safe in a daily care setting for patients with first-line or relapsed FL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Follicular lymphoma (FL) is the most common indolent non-Hodgkin’s lymphoma [1]. Although rituximab (MabThera/Rituxan; F. Hoffmann-La Roche Ltd, Basel, Switzerland), a chimeric monoclonal antibody, plus chemotherapy improves survival in first-line and relapsed disease [2–4], FL remains incurable. Most patients undergo multiple cycles of relapse and remission, with shorter remission periods between each successive treatment [5].
Rituximab maintenance (R-maintenance) improves progression-free survival (PFS) in patients with FL [6–11]. Consequently, responders to first-line therapy either observed or received maintenance treatment [12]. Prolonged exposure to anticancer drugs, however, can increase the risk of experiencing an adverse event (AE). Although R-maintenance has a favorable safety profile in trials with ≤5 years of follow-up [7–11], rates of neutropenia and infections can be higher in treated patients [7–9]. Thus, there are concerns that R-maintenance, which depletes B cells, may increase the rate of infectious complications.
Methods
Study design
The single-arm, phase IIIb Maintenance Rituximab in Follicular Lymphoma (MAXIMA; NCT00430352) study evaluated the safety and effectiveness of R-maintenance in patients with first-line or relapsed FL who responded to rituximab-containing induction. It also sought to confirm the effectiveness of R-maintenance in clinical trials [6–10, 13, 14]. The primary objective was the incidence of all-grade and grade 3/4 AEs. Secondary objectives included PFS, overall survival (OS), time to next lymphoma treatment (TNLT), and partial response (PR) to complete response/unconfirmed (CR/CRu) conversion rate.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Patients
Patients aged ≥18 years had first-line or relapsed (>6 months after previous therapy), histologically confirmed, grade 1–3a, CD20-positive FL, with documented CR/CRu or PR (per International Workshop criteria [15]) after induction with ≥8 cycles of rituximab (375 mg/m2) with or without chemotherapy. Chemotherapy choice during induction was per investigator’s discretion. Patients also had to have adequate hematologic function within 28 days prior to first R-maintenance infusion, immunoglobulin G levels ≥2 g/L, and Eastern Cooperative Oncology Group performance status (ECOG PS) of 0–2.
Treatment
Patients received ≤12 R-maintenance infusions (375 mg/m2) every 2 months for 2 years or until progressive disease (PD), relapse, start of new treatment, death, or unacceptable toxicity. Pharmacokinetic analyses showed that infusions were needed every 2 months to maintain serum levels >25 μg/mL in all patients [13]. The first R-maintenance dose was given 8 to 12 weeks after day 1 of the last induction cycle. Patients were followed every 3 months for 1 year after the last R-maintenance infusion and then per local practice until study end for OS, disease status, rituximab-related serious AEs (SAEs), and initiation of new lymphoma treatment. Rituximab could be infused at the standard rate (initially at 50 mg/h, with increases of 50 mg/h every 30 min to 400 mg/h in the absence of hypersensitivity or infusion-related reactions) or rapidly (over ≥90 min no faster than 600 mg/h) per local standard practice.
Assessments
AEs were assessed at baseline, every 8 weeks, and at premature discontinuation, follow-up visits, and study end as per National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), v3.0 [16]. Laboratory and physical examinations were performed at baseline, every 8 weeks, and at premature discontinuation and follow-up visits. Clinicians reported SAEs within 1 working day of initial observation.
Response was assessed at study entry, every 8 weeks, and at follow-up visits and study end by the investigator as per International Workshop criteria [15]. Clinical assessment of disease status should be made at all visits by investigators according to local practice. If imaging was performed, this was documented in the eCRF. During this study, bone marrow assessments were at the investigator's discretion.
Statistics
The planned sample size of 500 patients resulted in an 80 % probability of detecting any SAE that had occurred in ≥0.32 % of patients. The safety population included all patients who received ≥1 dose of R-maintenance. The intent-to-treat (ITT) population included all enrolled patients with a baseline assessment, regardless of whether R-maintenance was received. The ITT population was used for baseline characteristics and efficacy outcomes. All data are presented descriptively.
Results
Patient disposition
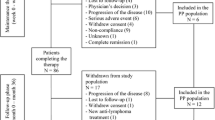
Beginning in 2006, 560 patients who achieved at least PR to induction were screened across 139 centers in 24 countries. Of these, 545 completed the baseline visit and had ≥1 further assessment (ITT population). Geographically, 27 patients (5.0 %) were recruited in Australia, 101 (18.5 %) in Central and Northern Europe, 60 (11.0 %) in Central and South America, 146 (26.8 %) in Eastern and Southeastern Europe, 29 (5.3 %) in the Middle East, and 182 (33.4 %) in Southern Europe. A total of 534 patients received ≥1 dose of R-maintenance (safety population).
Of the 534 patients in the safety population, 407 (76.2 %) received 12 infusions. Overall, 138 (25.3 %) of the 545 patients prematurely withdrew from the study or treatment, and 127 (23.8 %) of the 534 patients in the safety population prematurely discontinued. The early withdrawal rate was ~25 %; the most common reason for withdrawal was PD. Overall, 16 patients (2.9 %) were withdrawn from treatment because of AEs/SAEs; toxicity was the primary reason for discontinuation (Table 1).
Patient demographics
The median age of patients was 57.0 years, with 11.6 % (n = 63) aged ≥70 years (Table 2). The median age was lower than that described in FL epidemiology but comparable to clinical trials in this setting. Most had grade 1 or 2 FL and an ECOG PS of 0. A total of 395 patients (72.5 %) were treatment-naive before induction therapy, 99 patients (18.2 %) had used one previous line of treatment, 23 (4.2 %) had used two previous lines, and 28 patients (5.1 %) had used three or more lines. For the 150 patients who were previously treated, the following were used (multiple entries possible): rituximab (n = 84, 15.4 %), anthracycline-based regimen (e.g., CHOP [cyclophosphamide, doxorubicin, vincristine, and prednisone] or CHOP-like regimens; n = 89, 16.3 %), alkylating agent-based regimen (e.g., cyclophosphamide, vincristine, and prednisone; n = 63, 11.6 %), purine analog-based regimen (e.g., fludarabine, mitoxantrone, dexamethasone; n = 16, 2.9 %), high-dose chemotherapy and stem cell transplantation (n = 8, 1.5 %), and other(n = 30, 5.5 %). As part of this trial, most patients had received rituximab-based combination therapy as induction (519/545; 95.2 %), with anthracyclines being the most common chemotherapy partner. At study entry, most patients had CR/CRu (380/545; 69.7 %).
Hematologic AEs
Of the 534 patients evaluable for safety, 35 experienced (6.6 %) 51 hematologic AEs (Table 3). Eleven (2.1 %) experienced a grade 3 event and seven (1.3 %) reported a grade 4 event. The most common hematologic event was neutropenia, with 13 patients reporting 14 grade 3/4 neutropenia events. The same rates of any and higher-grade hematologic toxicity were seen in untreated and pretreated patients (see “Electronic supplementary material” Table 1). Treatment-related neutropenia occurred in five patients (0.9 %). A total of four (0.7 %) and three (0.6 %) patients had grade 3/4 neutropenia and febrile neutropenia, respectively, that were reported as SAEs. One patient died of immune thrombocytopenia, which was possibly related to treatment.
Prolonged neutropenia
Thirty-five (6.6 %) patients had prolonged neutropenia/leukopenia (lasting ≥14 days). Most (30/35; 85.7 %) received concomitant medication, with six (17.1 %) receiving colony-stimulating factors. Of the 13 patients with prolonged neutropenia grade 3/4, seven had one line of treatment, three had two lines, two had three lines, and one had four lines. Of these 13 patients with prolonged grade 3/4 neutropenia, six reported 12 infectious episodes (all grade 1/2). The most frequently occurring infections in this group were similar to those reported for the total study cohort. All cases resolved.
Infections
Overall, 193 patients (36.1 %) reported 422 infectious episodes (see Table 3). Nasopharyngitis, bronchitis, sinusitis, upper respiratory tract infection, and influenza were the most frequent events, each occurring in ≥3.7 %. Grade 3/4 events occurred in 4.3 % (grade 3, n = 21; grade 4, n = 2) of patients. The most frequent grade 3/4 infection was pneumonia (n = 4, 0.7 %), with one death from pneumonia. Serious infections related to rituximab were pneumonia (n = 3, 0.6 %), sinusitis, bacterial arthritis, bronchiolitis, herpes zoster, pulmonary tuberculosis, and respiratory tract infection (n = 1 each). No case of progressive multifocal leukoencephalopathy (PML) was observed.
Hypogammaglobulinemia
Decreased immunoglobulin G, M, and A blood levels were reported in 21 (3.9 %), 16 (3.0 %), and 4 (0.7 %) patients, respectively. Grade 3 reductions were reported for immunoglobulins G and M in two and three patients, respectively. No grade 4 reduction was observed.
Prolonged hypoimmunoglobulinemia (lasting ≥14 days) was reported in 32 patients. Among patients with prolonged immunoglobulin decrease, 13 (40.6 %) experienced 36 infectious episodes of any grade. Among the five patients with grade 3 or higher protracted immunoglobulinemia, three (60.0 %) reported 15 infectious episodes of any grade, with the most frequent being similar to those for the entire patient population. Of five patients with prolonged hypogammaglobulinaemia, three had one line of treatment, one had three lines, and one had four lines. Of the 32 patients with prolonged immunoglobulin decrease, five (15.6 %) received concomitant normal human or specific immunoglobulins. In summary, relevant hypogammaglobulinemia remains a rare event during R-maintenance. Immunoglobulin substitution per local practice is an option, and physicians may want to consider measuring immunoglobulin levels, particularly in patients with recurrent infections.
Infusion-related events
Of the 534 evaluable patients, 82 (15.4 %) received only rapid infusions, 370 (69.3 %) received only standard infusions, and 82 (15.4 %) received both. Fifty infusion-related AEs in 31 patients (5.8 %) were observed (see Table 3). Two patients experienced a grade 3 event; one experienced a grade 4 event. The most frequent infusion-related AE was hypotension, with five patients reporting five events. There was one infusion-related SAE, a grade 4 cerebrovascular event. The incidence of infusion-related AEs was similar among patients receiving all standard (5.4 %) or all rapid infusions (4.9 %).
Overall incidence of other AEs and SAEs (excluding those that were infusion-related)
Overall, 360 (67.4 %) patients had 1,864 non-infusion-related AEs. A total of 193 (36.1 %) patients had ≥1 AE due to infections and infestations, followed by 131 (24.5 %) who had ≥1 AE from gastrointestinal disorders; 130 (24.3 %) who had ≥1 AE from musculoskeletal and connective tissue disorders; 112 (21.0 %) who had ≥1 AE from general disorders and administrative site conditions; 93 (17.4 %) who had ≥1 AE from respiratory, thoracic, and mediastinal disorders; 80 (15.0 %) who had ≥1 AE from skin and subcutaneous tissue disorders; and 76 (14.2 %) who had ≥1 AE from nervous system disorders. The most commonly reported other AEs (≥5 % patients) were cough (49, 9.9 % of patients), fatigue (40, 7.5 %), nasopharyngitis (38, 7.1 %), back pain (35, 6.5 %), diarrhea (33, 6.9 %), arthralgia (32, 6.0 %), headache and hypertension (28, 5.2 % each), and pyrexia (27, 5.1 %). The majority of other AEs were grade 1 or 2.
Other AEs by CTCAE grading
With regard to other AEs by NCI CTCAE grading, of the 360 (67.4 %) patients who had ≥1 AE, 294 (55.1 %) had ≥1 grade 1 event (number of events = 1,212), 200 (37.5 %) had ≥1 grade 2 event (n = 490), 91 (17.0 %) had ≥1 grade 3 event (n = 121), 27 (5.1 %) had ≥1 grade 4 event (n = 29), and 11 (2.1 %) had ≥1 grade 5 event (n = 11).
Furthermore, 349 patients (65.4 %) had 1,734 AEs that were observed during the treatment period (treatment-emergent AEs [TEAEs]); 288 (53.9 %) of these patients had ≥1 grade 1 event (n = 1,155), 188 (35.2 %) had ≥1 grade 2 event (n = 452), 74 (13.9 %) had ≥1 grade 3 event (n = 92), 26 (4.9 %) had ≥1 grade 4 event (n = 27), and eight (1.5 %) had a grade 5 event (n = 8). The most frequently reported TEAEs (≥5 % patients) were cough (49, 9.2 % of patients), fatigue (39, 7.3 %), nasopharyngitis (36, 6.7 %), back pain (34, 6.4 %), diarrhea (31, 5.8 %), and arthralgia (30, 5.6 %).
In total, 150 other SAEs occurred, including 70 grade 3 reactions, 26 grade 4 reactions, and 11 deaths. Twenty-one events were considered to be related to treatment. The incidences of other AEs (63.9–77.5 %) and SAEs (20.2–20.3 %) were similar for standard and rapid infusions.
Death
A total of 40 patients died. Four patients (0.7 %) died during maintenance therapy; the investigator considered one patient’s death to be related to rituximab treatment, and the other three deaths were due to concurrent illness. Ten patients (1.9 %) died after maintenance therapy and before any further antineoplastic treatment (concurrent nonmalignant diseases, n = 2; other cancers, n = 3; lymphoma, n = 3; other, n = 2). After the initiation of new lymphoma treatment, there were 26 (4.9 %) additional deaths attributed to lymphoma (n = 18), other (n = 5), toxicity of additional treatment (n = 2), and concurrent illness (n = 1).
Efficacy
Kaplan–Meier survival estimates for PFS and OS by number of previous treatment lines are shown in Fig. 1. Median PFS, TNLT, and OS had not been reached at the time of evaluation. The number of patients experiencing PD did not appear to differ when patients were stratified by the number of previous lines of treatment, particularly the Kaplan–Meier curves for untreated and second-line patients. With regard to OS, only a few events, independent of the number of lines of previous treatment, proved lethal during and after R-maintenance. Surprisingly, the TNLT was also comparable among patients regardless of the number of lines of previous treatment.
Response status remained unchanged between the end of the induction and the maintenance periods for 467 patients (87.5 %). Of the 380 patients with postinduction CR/CRu, 342 (90.0 %) maintained CR/CRu, 31 (8.2 %) developed PD, and 7 (1.8 %) received no maintenance infusions. Of the 165 patients who achieved PR upon induction therapy, 10 (6.2 %) converted to CR/CRu, 25 (15.5 %) developed PD, and 4 (2.4 %) received no maintenance infusions (Fig. 2). When stratified by first-line versus relapsed treatment, response status remained unchanged from induction end to maintenance end for a similar percentage of patients (87.7 versus 86.9 %, respectively), with 91.0 % of first-line patients and 87.1 % of relapsed patients maintaining CR/CRu. Relative to relapsed patients, a higher percentage of first-line patients converted from PR to CR/CRu after R-maintenance (7.8 versus 2.2 %).
Response to R-maintenance among patients with PR to induction: a all patients, b first-line patients, and c relapsed patients (ITT population). CR/CRu complete response/unconfirmed complete response, ITT intent-to-treat, PD progressive disease, PR partial response, R-maintenance rituximab maintenance
Discussion
The present trial has demonstrated that R-maintenance administered every 2 months for 2 years in real-life clinical practice to patients after first-line induction or to those with relapsed FL is well tolerated and is not associated with undue treatment-related toxicity. Infections were reported in 36.1 % of patients, with 4.3 % experiencing grade 3/4 infections. Only 2.9 % of patients discontinued R-maintenance because of toxicity. Infection rates in patients experiencing prolonged neutropenia/leukopenia (42.9 %) or prolonged hypoimmunoglobulinemia (40.6 %) were comparable with those reported in the total trial population. No uncommon infections were reported in patients with prolonged neutropenia/leukopenia or with prolonged hypogammaglobulinemia. No case of PML was observed.
These data are consistent with previous reports on the safety of R-maintenance. The events were manageable and generally mild to moderate, with few treatment discontinuations [7–10]. Mild or moderate AEs, like cough, fatigue, or bronchitis, are relatively frequent and require the attention of the treating physician. Prolonged neutropenia and hypogammaglobulinemia, however, are rare events that are manageable and resolve. Physicians may want to measure immunoglobulin levels in those patients experiencing recurrent infections, even low-grade infections, and may want to consider immunoglobulin substitution according to local practice. The withdrawal rate from R-maintenance due to toxicity was low. Overall, this trial, which was conducted in a daily care setting in countries across the globe, confirms the safety profile seen with R-maintenance in efficacy-driven, randomized phase III trials [7, 8].
Previous trials have demonstrated that R-maintenance can extend PFS and event-free survival and delay TNLT [7–11]. In PRIMA, R-maintenance significantly improved PFS compared with observation (hazard ratio, 0.55; 95 % confidence interval, 0.44–0.68; p < 0.0001) [7]. The present study had a slightly higher rate (71/395; 17.9 %) of untreated patients with stage I/II compared with the PRIMA trial where 10 % of the entire study population were stage I/II. The authors believe that the patient populations still remain comparable. The present trial was single-armed, but outcomes for PFS, OS, and TNLT were comparable with those observed in previously reported randomized trials [7, 8], which suggests that R-maintenance can also improve patient outcomes in real-life clinical practice. Interestingly, we did not observe substantial differences among patients receiving first-line versus subsequent lines of treatment in the reduction of the risk of progression, survival, or TNLT with respect to the administration of R-maintenance.
The percentage of patients who maintained CR after induction was high. Conversion rates from PR to CR/CRu during maintenance were lower in this trial (10/165, 6.2 %) than those previously reported [7, 8]. In daily care, not all patients receive rituximab by standard infusion; rapid infusion is used in several countries. Our findings are consistent with other clinical trials, which have shown that rapid rituximab infusion is safe and well tolerated [17, 18]. The findings of the present trial are compatible with data from previous randomized phase III studies that demonstrated that R-maintenance (every 2 months) can be safely and effectively administered to patients with FL who are undergoing first-line induction or re-treatment in a daily care setting across the globe.
References
Cheson BD, Coiffier B (2008) Non-Hodgkin lymphoma. In: Armitage JO (ed) Atlas of clinical hematology, 2nd edn. Current Medicine Group, Philadelphia
Marcus R, Imrie K, Belch A, Cunningham D, Flores E, Catalano J et al (2005) CVP chemotherapy plus rituximab compared with CVP as first-line treatment for advanced follicular lymphoma. Blood 105(4):1417–1423
Forstpointner R, Dreyling M, Repp R, Hermann S, Hänel A, Metzner B et al (2004) The addition of rituximab to a combination of fludarabine, cyclophosphamide, mitoxantrone (FCM) significantly increases the response rate and prolongs survival as compared with FCM alone in patients with relapsed and refractory follicular and mantle cell lymphomas: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 104(10):3064–3071
Hiddemann W, Kneba M, Dreyling M, Schmitz N, Lengfelder E, Schmits R et al (2005) Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 106(12):3725–3732
Johnson PW, Rohatiner AZ, Whelan JS, Price CG, Love S, Lim J, Matthews J et al (1995) Patterns of survival in patients with recurrent follicular lymphoma: a 20-year study from a single center. J Clin Oncol 13(1):140–147
van Oers MH, Klasa R, Marcus RE, Wolf M, Kimby E, Gascoyne RD et al (2006) Rituximab maintenance improves clinical outcome of relapsed/resistant follicular non-Hodgkin lymphoma in patients both with and without rituximab during induction: results of a prospective randomized phase 3 intergroup trial. Blood 108(10):3295–3301
Salles G, Seymour JF, Offner F, López-Guillermo A, Belada D, Xerri L et al (2011) Rituximab maintenance for 2 years in patients with high tumour burden follicular lymphoma responding to rituximab plus chemotherapy (PRIMA): a phase 3, randomised controlled trial. Lancet 377(9759):42–51
van Oers MH, Van Glabbeke M, Giurgea L, Klasa R, Marcus RE, Wolf M et al (2010) Rituximab maintenance treatment of relapsed/resistant follicular non-Hodgkin's lymphoma: long-term outcome of the EORTC 20981 phase III randomized intergroup study. J Clin Oncol 28(17):2853–2858
Forstpointner R, Unterhalt M, Dreyling M, Böck HP, Repp R, Wandt H et al (2006) Maintenance therapy with rituximab leads to a significant prolongation of response duration after salvage therapy with a combination of rituximab, fludarabine, cyclophosphamide, and mitoxantrone (R-FCM) in patients with recurring and refractory follicular and mantle cell lymphomas: results of a prospective randomized study of the German Low Grade Lymphoma Study Group (GLSG). Blood 108(13):4003–4008
Martinelli G, Schmitz SF, Utiger U, Cerny T, Hess U, Bassi S et al (2010) Long-term follow-up of patients with follicular lymphoma receiving single-agent rituximab at two different schedules in trial SAKK 35/98. J Clin Oncol 28(29):4480–4484
Vidal L, Gafter-Gvili A, Leibovici L, Shpilberg O (2009) Rituximab as maintenance therapy for patients with follicular lymphoma. Cochrane Database Syst Rev 2, CD006552
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: non-Hodgkin's lymphomas. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site. Accessed 8 Jan 2014
Gordan LN, Grow WB, Pusateri A, Douglas V, Mendenhall NP, Lynch JW (2005) Phase II trial of individualized rituximab dosing for patients with CD20-positive lymphoproliferative disorders. J Clin Oncol 23(6):1096–1102
Ghielmini M, Schmitz SF, Cogliatti SB, Pichert G, Hummerjohann J, Waltzer U et al (2004) Prolonged treatment with rituximab in patients with follicular lymphoma significantly increases event-free survival and response duration compared with the standard weekly × 4 schedule. Blood 103(12):4416–4423
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM et al (1999) Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17(4):1244–1253
National Cancer Institute (NCI) Cancer Therapy Evaluation Program (CTEP) (2014) Major initiatives, common terminology criteria for adverse events (CTCAE). http://ctep.cancer.gov/MajorInitiatives/Common_Terminology_Criteria.htm. Accessed 8 Jan 2014
Sehn LH, Donaldson J, Filewich A, Fitzgerald C, Gill KK, Runzer N et al (2007) Rapid infusion rituximab in combination with corticosteroid-containing chemotherapy or as maintenance therapy is well tolerated and can safely be delivered in the community setting. Blood 109(10):4171–4173
Al Zahrani A, Ibrahim N, Al Eid A (2009) Rapid infusion rituximab changing practice for patient care. J Oncol Pharm Pract 15(3):183–186
Disclosures
All authors have provided substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; and provided final approval of the version to be published. Informed consent was obtained from all patients for being included in the study.
Conflict of interest
Dr. Mathias Witzens-Harig and Dr. Alice di Rocco have received funding from F. Hoffmann-La Roche Ltd. Dr. Andrej Vranovsky has received lecture and consulting fees from F. Hoffmann-La Roche Ltd. Dr. Dan Thurley and Dr. Stephan Oertel are salaried employees of and own stock in F. Hoffmann-La Roche Ltd. All remaining authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Witzens-Harig, M., Foá, R., Di Rocco, A. et al. Maintenance with rituximab is safe and not associated with severe or uncommon infections in patients with follicular lymphoma: results from the phase IIIb MAXIMA study. Ann Hematol 93, 1717–1724 (2014). https://doi.org/10.1007/s00277-014-2103-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2103-3