Abstract
To assess the efficacy and toxicity of HAA regimen (Homoharringtonine 4 mg/m2/day, days 1–3; cytarabine 150 mg/m2/day, days 1–7; aclarubicin 12 mg/m2/day, days 1–7) as a salvage therapy in the treatment of refractory and/or relapsed acute myeloid leukemia (AML), 46 patients with refractory and/or relapsed AML, median age 37 (16–65) years, participated in this clinical study. The median follow-up was 41 (10–86) months. Eighty percent of patients achieved complete remission (CR), and the first single course of re-induction HAA regimen resulted in CR rate of 76.1 %. The study protocol allowed two courses of induction. The CR rates of patients with favorable, intermediate and unfavorable cytogenetics were 90 %, 88.9 %, and 37.5 %, respectively. For all patients, the estimated 3-year overall survival (OS) rate was 42 %, and the estimated relapse free survival (RFS) at 3 years for the 36 CR cases was 49 %. The toxicities associated with HAA regimen were acceptable. HAA is a good choice in cases with refractory/relapsing AML for salvage chemotherapy, preferably with a high-efficacy and low-toxicity profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kell [1] proposed that “modern induction chemotherapy will result in complete remission (CR) in 50–90 % of patients with de novo acute myeloid leukemia (AML), but between 10 % and 25 % of patients will have primarily refractory disease and the majority of those who gain remission will relapse within 3 years of diagnosis”. Salvage chemotherapy can induce remissions in up to 50 % of patients who relapse or do not respond to initial induction chemotherapy, but their long-term prognosis remains poor. Allogeneic and autologous blood and marrow transplantation can provide long-term disease control for some of these patients, but most patients with refractory or relapsed AML will eventually succumb to their disease [2]. Thus, the development of new and more effective agents for the treatment of AML will be important in improving disease control and patient survival.
In recent years, new agents, which are modified older agents (e.g., liposomal formulations), and new combinations of conventional drugs have been developed and studied. Many new combination regimens were based on high doses of cytarabine arabinoside (Ara-c) [3, 4], or substitution of the anthracyclines mitoxantrone [4, 5] or idarubicin [6, 7] for daunorubicin, or using amsacrine [8, 9], or addition of the purine nucleotide analogue fludarabine to Ara-c [6, 7, 10]. However, these trials produced second CR rates of 10–70 % relying on historical controls [1].
Most patients have already been exposed to intensive multiagent chemotherapy and quite a few of these patients required salvage regimens, most of which can cause substantial toxicity [11–13]. The multi-center phase II study performed by the Polish Adult Leukemia Group [14] demonstrated that in 118 patients, a 58 % CR rate was achieved after one or two courses of CLAG-M, with 35 % being refractory and 7 % dying early due to severe toxicities. Yavuz et al. [15] employed fludarabine phosphate 25 mg/m2/day (d1–5), Ara-c 2 g/m2/day (d1–5), idarubicin 12 mg/m2/day (d1–3), and G-CSF which was given subcutaneously from day 6 until absolute neutrophil count (ANC) >500/mL. CR was achieved in 15 cases (44.1 %) in 34 AML patients, and the median survival time was 16 weeks. At the end of the study, only three patients were alive and two of these were in continuous remission.
Therefore, finding new agents and combination therapies that might overcome multidrug resistance and decrease toxicities has thus been actively pursued. Clinical studies for de novo AML in vivo were conducted and showed that with HAA (Homoharringtonine, Ara-c, and aclarubicin), the CR rate reached 83 % and the estimated overall survival (OS) rate at 3 years reached 75 % [16]. The toxicities associated with HAA regimen were acceptable. The encouraging results above coupled with our experience with homoharringtonine (HHT) used in AML for the past 10 years prompted us to establish HAA as a pilot salvage regimen. The goal of this study is to assess the efficacy and toxicity of HAA in refractory and relapsed AML patients.
Patients and methods
Patients
Between February 2004 and December 2009, 46 patients with refractory/relapsing acute myeloid leukemia treated at the Department of Hematology, the First Affiliated Hospital, Zhejiang University College of Medicine participated in this clinical trial. The median follow-up was 41 (10–86) months for patients alive. All the eligible patients fulfilled the following criteria: the diagnosis of AML was established according to the standard French-American-British (FAB) [17] cytological and cytochemical criteria; over 16 years old; diagnosed as having refractory/relapsed AML without major comorbidity (no evidence of cardiac disease; left ventricle ejection fraction>50 %); patients with more than one previous treatment were included; peripheral blood and bone marrow samples were evaluated by morphology, histochemistry, and immunophenotyping; serum creatinine level was ≤2 mg/dL and bilirubin was ≤2 mg/dL; Eastern Cooperative Oncology Group (ECOG) performance status score was 0–2; transaminase levels were within 2.5 times the upper limit of normal; life expectancy was ≥6 weeks; and informed consent was obtained from all patients for being included in the study. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Patients were not eligible if they had AML subtype M3 according to the FAB classification, uncontrolled infection, hepatic or renal insufficiency, uncompensated disseminated intravascular coagulation, or if they refuse to participate in the study.
Patients not responding to remission induction therapy were accepted as primarily refractory cases. Relapsing disease was defined as a response to remission induction and blast increase in peripheral blood and/or bone marrow >5 % during follow-up. A relapse developing in patients in the first 6 months after CR was considered as early relapse (ER). Late relapse (LR) was defined as relapse more than 6 months after CR1.
All patients were previously treated according to Cancer and Leukemia Group B (CALGB) [18] or the regimen proposed by Jin et al. [16], and had thus received standardized first-line treatment. According to CALGB, DA first-line therapy consisted of daunorubicine (DNR) 60 mg⁄m2 on days 1–3, Ara-c 200 mg⁄m2 on days 1–7. HAA proposed by Jin et al. was composed of HHT 4 mg/m2/day, days 1–3, Ara-c 150 mg/m2/day, days 1–7, and aclarubicin 12 mg/m2/day, days 1–7. Patients achieving CR continued to have consolidation therapy. In patients with partial remission (PR) or blast decrease in bone marrow >60 %, the same induction regimen was repeated.
Cytogenetics was assessed at both primary diagnosis of AML and diagnosis of relapse. Patients with karyotypes of t(8;21), inv(16), or t(16;16) were considered to have low-risk cytogenetics, while those with karyotypes -5, -7, del(5q), abnormal 3q or complex cytogenetics (defined as the presence of at least three unrelated cytogenetic abnormalities) were regarded to have high-risk cytogenetics. Patients with normal cytogenetics and other miscellaneous single abnormalities were defined as having intermediate-risk cytogenetics.
Treatment protocol
The HAA regimen consisted of HHT, Ara-c, and aclarubicin. HHT was administered at a dose of 4 mg/m2 by continuous infusion over 4 h daily (or 2 mg/m2 intramuscular injection twice daily) for 3 days (days 1–3). Ara-c was given at a dose of 75 mg/m2 twice daily (the daily dose was 150 mg/m2) for 7 days (days 1–7), and aclarubicin was administered at a dose of 12 mg/m2 daily by continuous infusion over 2 h for 7 days (days 1–7). HHT was administered intramuscularly to 44 patients, and 2 patients were administered by continuous infusion. All patients were treated with identical salvage chemotherapy, except for the reasons of unacceptable toxicity (grades III–IV) (i.e., cardiovascular complications with HHT or aclarubicin) or patient choice. Toxicity was graded according to the National Cancer Institute common toxicity criteria [19]. Upon recovery of the periphery blood count, a bone marrow aspirate was performed to assess the status of the response. Patients who achieved CR received consolidation therapy. For patients with PR or blast decrease in bone marrow >60 %, the same HAA regimen was repeated, whereas for patients with non-remission (NR) after the first course of re-induction therapy or with PR/NR after two courses of re-induction therapy, second line salvage chemotherapy was administered. Granulocyte colony-stimulating factor 5 μg/kg was administered subcutaneously and daily from the day when neutrophil count was <0.5 × 109/L until neutrophil count was >1 × 109 /L for 3 successive days. Antibiotic and antifungal treatment and supportive care were given according to common guidelines. Consolidation therapy including one course of the same HAA regimen as used in salvage therapy was applied 2–4 weeks after achievement of CR followed by two courses of intermediate-dose cytarabine regimen. All patients in CR who had a suitable donor were referred for allogeneic stem cell transplantation (allo-SCT), whereas those without a donor were qualified for maintenance therapy or autologous stem cell transplantation (auto-SCT). Maintenance therapy included one course of HA, two courses of AA, and one course of MA. Dose and usage of every drug were showed as following: HHT was administered at a dose of 2 mg/m2 by intramuscular injection twice daily for 3 days; Ara-c was given at a dose of 75 mg/m2 subcutaneously twice daily for 7 days; aclarubicin was administered at a dose of 12 mg/m2 daily by continuous infusion over 2 h for 7 days; mitoxantrone was given at a dose of 8 mg/m2 by intravenous infusion for 3 days.
Response criteria are as follows: (1) CR: Peripheral blood counts within normal limits (neutrophils >1.5 × 109/L, platelets >100 × 109/L, no blasts in peripheral blood) plus bone marrow blast percentage <5 %, and no extramedullary disease; (2) PR: Peripheral blood counts within normal limits plus bone marrow blast percentage between 5 % and 20 % and peripheral blood blasts >5 % with neutrophils >1.5 × 109/L, platelets >50 × 109/L, lymphoid nodes <2 cm, splenomegaly <2 cm below left costal margin, hepatomegaly <5 cm below right costal margin and considerable improvement of performance status; (3) NR was established for patients who did not fulfill the above criteria; (4) Early death (ED): Death following re-induction treatment before it was possible to assess the remission status.
All patients underwent full clinical examinations and assessment of blood counts. Liver and kidney functions were tested before each course of chemotherapy. As a routine, electrocardiograms (ECG) and blood culture were obligatory for all patients before and after each course of chemotherapy during re-induction, consolidation, and maintenance phases. Ultrasound cardiography and Holter monitoring were performed in those cases suspected to have cardiac problems after either ECG or signs of clinical manifestation. The remission status was assessed after completion of each course of salvage, consolidation, and maintenance therapy.
Statistical analysis
SPSS 12.0 pocket program has been used for statistical analysis. OS was defined as duration of the first day of salvage chemotherapy to patients deceased or alive at last follow-up (censored). Relapse-free survival (RFS) was defined as duration from the day when CR was detected to relapse, deceased or alive at last follow-up (censored).
The primary end-point of this study was the CR rate achieved after one course of HAA regimen. The overall CR rate achieved after one or two HAA courses as well as the probability of OS and RFS were secondary end-points. The Fisher's exact test was used to compare differences in percentages. OS and RFS were estimated using the Kaplan–Meier method. Log rank tests were used to evaluate the univariate effects of particular independent variables on OS and RFS. In the univariate analysis of risk factors, the following variables were evaluated: sex, age, disease status, induction therapy regimen, and risk group by karyotype as well as white blood cell (WBC), hemoglobin (Hb), platelet (PLT), and bone marrow (BM) infiltration at study entry. Continuous variables were first divided into four categories at approximately the 25th, 50th, and 75th percentiles. If the relative event rates (ratio of the observed number of events to the expected number of events in a category, assuming no variation across categories) in two or more adjacent categories were not substantially different, these categories were grouped together. If no clear pattern was observed for the outcome, the median was taken as the cut point. For multivariate analysis of factors affecting OS and RFS, Cox proportional hazard regression model was used, whereas for the analysis of CR rate, logistic regression model was applied. P value <0.05 has been accepted as meaningful.
Results
Patients
A total of 46 patients, 26 male and 20 female, with refractory and relapsing AML, were enrolled in this study. The median age was 37 years (in a range of 16–65). Eleven cases were primarily refractory and the remaining 35 patients were relapsing. Most patients had either M2 (30/46) or M5 (10/46) subtypes. All but one patient had completed cytogenetic study. Thus, karyotypes were established in 45 patients, with 10 cases having favorable cytogenetics, 27 patients having intermediate cytogenetics and 8 cases having unfavorable cytogenetics. Forty-five cases had de novo disease and one had AML secondary to myelodysplastic syndrome. Thirty-three patients received DNR and Ara-c (DA) as the first-line induction therapy, and 13 received the HAA regimen. All patients received re-induction treatment. Baseline characteristics of patients are summarized in Table 1.
Response to HAA induction therapy
A single course of HAA therapy resulted in CR rate of 76.1 % (35/46) patients, with PR and NR rate of 4.3 % (2/46) and 19.6 % (9/46), respectively. None of patients died of treatment-related toxicities during the first course. After the first course of re-induction, patients with PR or NR received another course of either the identical re-induction therapy or a second-line salvage treatment. An additional 4.3 % (2/46) of patients treated with a second HAA regimen achieved CR and thus the overall CR rate reached 80.4 % (37/46).
The CR rate was 95 % (19/20) and 100 % (2/2) for late and second relapse patients, and it was only 63.6 % (7/11) and 69.2 % (9/13) for refractory and early relapse patients, respectively. However, the difference was not significant (P = 0.103) (Table 2). There was a significant difference (P = 0.023) for CR rates in pairwise comparisons of late relapse and second relapse patients versus combined refractory and early relapse patients, but there was no significant difference in multivariable analyses. Of the 20 late relapse patients, 4 had favorable cytogenetics and 15 had intermediate cytogenetics. Of the 10 patients with favorable cytogenetics, 9 achieved CR (90 %). Of the 27 patients with intermediate cytogenetics, 24 (88.9 %) achieved CR. However, of the 8 patients with unfavorable cytogenetics, 3 (37.5 %) obtained CR. The difference was significant (P = 0.004) (Table 2). Of the 31 patients with age <45 years old, 28 (90.3 %) achieved CR, whereas of the 15 patients with age ≥45 years old, 9 (60 %) obtained CR. The difference was significant (P = 0.042) (Table 2). The type of first-line chemotherapy (DA or HAA) did not influence the probability of achieving CR after salvage HAA (Table 2).
The factors associated with increased risk of treatment failure in univariate analyses were poor karyotype, age ≥45 years old, combined group of primary refractoriness and early relapse (Table 2). There was no correlation between response rate and sex, leukocyte, platelet count, blast count in bone marrow, leukemia subtype (AML FAB subtype) (P > 0.05). The only factor associated with increased risk of treatment failure in multivariate analyses was poor karyotype (data not shown).
The median time from the initiation of the re-induction therapy to the evaluation of the remission status in patients who achieved CR after a single course was 38 (21–53) days versus 62 (57–68) days in patients who achieved CR after two courses. For all patients who achieved CR, the median time from the initiation of the salvage therapy to the evaluation of the remission status was 40 (21–68) days.
Toxicity
All patients experienced profound granulocytopenia. The most common toxicities during salvage phase were infections. Of all 46 patients, 41 (89.1 %) had various degree of infections (etiology: bacterial −22 %, fungal −9.8 %, mixed −17 %, negative culture −68.3 %), and 16 (34.8 %) had severe (grades III–IV) infections (etiology: bacterial −31.3 %, fungal −25 %, mixed −6 %, negative culture −43.8 %). Most patients with infections manifested as pneumonia, acute bronchitis, and tracheitis (31.7 %). No patient suffered severe bleedings. Ocular hemorrhage and petechia were controlled with the administration of platelet transfusions. Grade III–IV nausea and vomiting (6.5 %) and gastrointestinal toxicity (2.2 %) were entirely reversible (Table 3).
The other WHO grade I–II toxicities included transient liver dysfunction (10.9 %), drug allergic (2.2 %), and hyperglycemia (13 %). No hypotension was observed.
With re-induction therapy, severe granulocytopenia and thrombocytopenia occurred to all patients. The median minimal WBC count amounted to 0.4 (0.1–1.4) × 109/L. The interval from the start of the re-induction therapy to the day when neutrophil count began to be less than 1 × 109/L was 11 days, and the duration of neutrophil count less than 1 × 109/L was 13 days. The median minimal platelets were 5 × 109/L, and the interval from the start of the re-induction therapy to full recovery of the platelets (>100 × 109/L) was 33 days (Table 3).
Survival analysis
Of all the 46 patients, one patient was lost to follow-up who, upon achieving CR after the first re-induction therapy, refused to continue receiving further therapy. Among the 45 patients, there were nine cases in the NR group. Of these nine NR cases, three cases achieved CR after the third-line chemotherapy (FLAG or AE), but all relapsed again and died 9–21 months after relapse. The other six NR cases died 2–7 months after the first course of re-induction therapy. Among the 36 patients in CR group, there were 21 cases of relapse (one case relapsed only in central nervous system). Of the above 21 patients, 9 patients died subsequently; 5 patients received allo-SCT (of these 5 patients, 3 were still alive by the time of closeout; 1 died of GVHD; and another one relapsed and then died subsequently); 6 patients achieved CR after receiving the third-line therapy (of these 6 patients, 4 relapsed again and died finally, and another 2 were alive with sustaining CR); 1 remains alive with sustaining NR. Among the 36 CR patients, 15 patients did not relapse. Of these 15 patients, 2 received allo-SCT, but both died of pneumonia. At the time of study closeout, 18 patients were still alive without disease, and 1 was alive with sustaining NR.
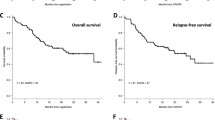
With a median follow-up of 41 months for the 45 patients, the estimated 3-year OS rate was 42 %, and the median OS for all the evaluable patients was 29 (2–86) months (Fig. 1a). For those 36 patients who achieved CR, the estimated RFS at 3 years was 49 %, and the median time of RFS was 29 (0.5–85) months (Fig. 1b). According to cytogenetic risk group, the estimated 3-year OS rate for the intermediate and favorable cytogenetic groups was 58 % and 40 %, respectively. For patients with unfavorable cytogenetics, the estimated median OS time was only 9.5 (4–41.5) months (Fig. 2a, Table 4). The estimated 3-year RFS rate for the intermediate and favorable cytogenetic groups were 57 % and 44 %, respectively, and the estimated RFS time for patients with unfavorable cytogenetics was only 3 months (Fig. 2b, Table 5). Of the 22 patients with Hb <10 g/dl, the estimated OS and RFS at 3 years were 29 % and 38 % respectively, whereas of the 23 patients with Hb ≥10 g/dl, the estimated OS and RFS at 3 years were 55 % and 57 % (Fig. 3, Table 5).
OS and RFS were influenced by leukemia-related factors (i.e., poor karyotype (Fig. 2) and Hb<10 g⁄dl (Fig. 3)) in both univariate (Tables 4 and 5) and multivariate (data not shown) analyses.
In this study, allo-SCT was performed to 7 patients and all achieved CR. However, one case died of GVHD; 2 died of pneumonia; 1 relapsed and died of disease progress; and another 3 were still alive with CR. By the time of closeout, the life expectancy time of the 3 patients after allo-SCT was 25, 13, and 2 months, respectively.
Discussion
Refractory and resistant disease to conventional induction chemotherapy and relapsed disease are considered the most important adverse prognostic factors for AML. Salvage chemotherapy can be used to achieve long-term survival and high CR rate, to provide a bridge to hematopoietic stem cell transplantation (HSCT) aimed at prolonging RFS and OS, or to temporarily prolongate life and palliate symptoms.
The concept of this study was based on previously published data that HHT had significant potentially synergistic effects on Ara-c and other agents [20, 21]. Aclarubicin, an alternative to DNR, had promising antileukemic efficacy in combination with Ara-c [22]. The efficacy of HHT in combination with Ara-c and aclarubicin in the treatment of de novo adult AML patients was proven in our previous study [16]. CR was achieved in 79 % (38/48) patients with a single HAA induction course, and toxicities associated with HAA regimen were acceptable. This present study assessed the efficacy and toxicity of HAA salvage regimen in 46 adult refractory and relapsed AML patients. As we know, in patients of comparable age treated with salvage regimen, typically only 14–60 % CR rates can be achieved [7, 23–27]. So, in this study, achieving a CR rate of 76.1 % with a single course and 80.4 % of total were quite remarkable.
It was interesting that 42 % of OS rate at 3 years and 29 months of median OS of the patients in our study were better than that reported by other studies [4, 25, 26, 28, 29]. In a clinical trial conducted by Wierzbowska et al. [14], of 118 relapsed and refractory AML patients who were observed for 4 years, 70 % relapsed or died. In our study, of 36 CR patients, there were 21 (46 %) cases that relapsed (one case relapsed only in central nervous system) after a median time of 13 months. It is difficult to compare the relapse rates between our study and the others' because of so many factors that could interfere with the results, such as age, FAB subtype, and so on. For example, our study cohort was of relatively young age and included a relatively high proportion of patients with favorable and intermediate cytogenetics. However, the study investigated by Wierzbowska et al. [14] had a higher proportion of patients with unfavorable cytogenetics and a slightly higher median age. In addition, the AML-M2 and M5 patients accounted for 86 % in our study. These two types are associated with relatively favorable cytogenetics. The above factors might shift our results to more favorable outcomes. Even so, the results were still encouraging.
It is well established that patients with refractory disease and early relapses have significantly poorer response to chemotherapy and worse overall outcome compared to patients with later relapses [30–33]. In cases of failing one course of salvage chemotherapy, the probability of CR is even lower than 1 % [34]. In our study, the difference was significant for CR rates in pairwise comparisons of late relapse and second relapse patients versus combined refractory and early relapse patients. Late relapse patients appear to respond relatively well to the study treatment. However, we did not find any significant differences in OS and RFS between the primarily refractory group and the relapsing group. For this reason, we can suggest that the HAA regimen can be effectively used in cases of refractory disease as in relapsing disease. For 11 refractory cases, the CR rate and OS at 3 years reached 63.6 % and 47 %. In the study conducted by Wierzbowska et al. [14], of 75 refractory patients, CR was seen in only 50.7 % of patients and 21 % of patients survived for ≥2 years. Based on these results, it is reasonable to say that HAA regimen might be a good choice for refractory patients. In addition, our study revealed that age over 45 years was an adverse factor for treatment failure. This result was consistent with what was mentioned in Kell's review [1].
Kell [1] proposed that cytogenetic abnormalities appeared to be less important in response rate and life time of patients. However, Breems et al. [31] found that patients with favorable cytogenetics at diagnosis continued to express more favorable prognosis at relapse. In addition, Chevallier et al. [35] addressed that high-risk cytogenetics was one of the strongest independent adverse prognostic factors for OS and EFS. Analysis of data from our study taking into account cytogenetic risk groups also showed that karyotypes at diagnosis remained important prognostic factors, which could predict CR rate and long-term perspectives. In the studies by Lee et al. [10] and Wierzbowska et al. [14], the CR rate of the patients with unfavorable cytogenetics was 46.7 % and 44.4 %. In the study by Breems et al. [31], OS at 5 years of the patients with unfavorable cytogenetics reached 4 %. But for eight patients with unfavorable cytogenetics in present study, the CR rate and OS at 3 years were 37.5 % and 0 %, that indicated HAA regimen had no superiority over other salvage therapy for patients with unfavorable cytogenetics. Poor karyotype was an adverse factor for CR rate, OS, and RFS. These results showed that the antileukemic efficacy of HAA for those patients with unfavorable cytogenetics was limited. Perhaps, a high-dose regimen or stem cell transplantation would be more effective for such patients.
We also evaluated other factors that may be predictive for prognosis such as sex, WBC, Hb, platelet count, type of the first-line chemotherapy, and blast count in bone marrow when relapsing. Hb ≥10 g/dl was predictive for higher OS and RFS. Similar observations were reported earlier by Kern et al. [33]. In our study, 33 patients were treated with DA regimen as the first-line induction therapy and 13 received HAA. It should be emphasized that the type of the first-line chemotherapy did not influence probability of achieving CR and OS after salvage HAA. In addition, the other factors also showed no significant influence to prognosis.
In addition to this encouraging response rate, the attractive regimen safety, tolerable and mostly reversible side effects, and 0 % early mortality were all notable. The relatively low intensity of the regimen, improved standards of supportive care, and decisions concerning salvage treatment at earlier stages of the disease may explain the zero mortality rates. Non-hematologic toxicity was acceptable and routine supportive therapy was sufficient to control the signs and symptoms. Severe granulocytopenia and thrombocytopenia occurred in all patients during induction therapy. The median duration of 13 days of nadir neutrophil count in the current cohort was shorter than that of 24 days reported by other investigators [14]. Therefore, the toxicities associated with HAA regimen were acceptable.
In summary, HAA regimen is a well-tolerated and effective salvage regimen for patients with refractory or relapsed AML. The CR rate especially that achieved after the first course of salvage therapy and the OS and RFS at 3 years in this study was encouraging, although the antileukemic activity in patients with unfavorable cytogenetics was limited. High response rate probably resulted from synergistic effect between HHT, Ara-c, and aclarubicin to overcome leukemic cells' resistance. Since this study was a phase II clinical trial, to provide adequate justification for the above observation, further investigation with a randomized phase III trial is still warranted.
References
Kell J (2006) Treatment of relapsed acute myeloid leukaemia. Rev Recent Clin Trials 1:103–111
Rowe JM, Li X, Cassileth PA, Appelbaum FR, Schiffer CA, Wiernik PH, Litzow MR, Cripe LD, Lazarus HM, Paietta E, Dewald GW, Weinstein HJ, Ogden AK, Woods WG, Shep-herd L, Feusner JH, Bloomfield CD, Tallman MS (2005) Very poor survival of patients with AML who relapse after achieving a first complete remission: the Eastern Cooperative Oncology Group Experience (Abstract 546). Blood 106:162a
Vogler WR, McCarley DL, Stagg M, Bartolucci AA, Moore J, Martelo O, Omura GA (1994) A phase III trial of high-dose cytosine arabinoside with or without etoposide in relapsed and refractory acute myelogenous leukemia. A Southeastern Cancer Study Group trial. Leukemia 8:1847–1853
Kern W, Aul C, Maschmeyer G, Schönrock-Nabulsi R, Ludwig WD, Bartholomäus A, Bettelheim P, Wörmann B, Büchner T, Hiddemann W (1998) Superiority of high-dose over intermediate-dose cytosine arabinoside in the treatment of patients with high-risk acute myeloid leukemia: results of an age-adjusted prospective randomized comparison. Leukemia 12:1049–1055
Karanes C, Kopecky KJ, Head DR, Grever MR, Hynes HE, Kraut EH, Vial RH, Lichtin A, Nand S, Samlowski WE, Appelbaum FR (1999) A phase III comparison of high dose ARA-C (HIDAC) versus HIDAC plus mitoxantrone in the treatment of first relapsed or refractory acute myeloid leukemia Southwest Oncology Group Study. Leuk Res 23:787–794
De la Rubia J, Regadera AI, Martin G, Cervera J, Sanz G, Martínez J, Jarque I, García I, Andreu R, Moscardó F, Jiménez C, Mollá S, Benlloch L, Sanz M (2002) FLAG-Ida regimen (fludarabine, cytarabine, idarubicin and G-CSF) in the treatment of patients with high risk myeloid malignancies. Leuk Res 26:725–730
Pastore D, Specchia G, Carluccio P, Liso A, Mestice A, Rizzi R, Greco G, Buquicchio C, Liso V (2003) FLAG-IDA in the treatment of refractory/relapsed acute myeloid leukemia: single-center experience. Ann Hematol 82:231–235
Martiat P, Ghilain JM, Ferrant A, Doyen C, Delannoy A, Chatelain C, Bosly A, Michaux JL, Sokal G (1990) High-dose cytosine arabinoside and amsacrine or mitoxantrone in relapsed and refractory acute myeloid leukaemia: a prospective randomized study. Eur J Haematol 45:164–167
Ganser A, Heil G, Seipelt G, Hofmann W, Fischer JT, Langer W, Brockhaus W, Kolbe K, Ittel TH, Brack N, Fuhr HG, Knuth P, Höffken K, Bergmann L, Hoelzer D (2000) Intensive chemotherapy with idarubicin, ara-C, etoposide, and m-AMSA followed by immunotherapy with interleukin-2 for myelodysplastic syndromes and high-risk acute myeloid leukemia (AML). Ann Hematol 79:30–35
Lee SR, Yang DH, Ahn JS, Kim YK, Lee JJ, Choi YJ, Shin HJ, Chung JS, Cho YY, Chae YS, Kim JG, Sohn SK, Kim HJ (2009) The clinical outcome of FLAG chemotherapy without idarubicin in patients with relapsed or refractory acute myeloid leukemia. J Kor Med Sci 24:498–503
Davis C, Rohatiner A, Amess J, Lim J, Lister TA (1993) The management of recurrent acute myelogenous leukemia at a single center over a fifteen year period. Br J Haematol 83:404–411
Liso V, Iacopino P, Avvisati G, Petti MC, Broccia G, Carotenuto M, Falda M, Fazzi P, Lazzarino M, Leoni P, Mirto S, Pucci G, Nobile F, Nosari AM, Specchia G, Stasi R, Tabilio A, Mandelli F (1996) Outcome of patients with acute myeloid leukemia who failed to respond to a single course of first-line induction therapy: a GIMEMA study of 218 unselected consecutive patients. Leukemia 110:1443–1452
Vignetti M, Orsini E, Petti MC, Moleti MR, Andrizzi C, Pinto RM, Amdori S, Meloni G (1996) Probability of long term disease free survival for acute myeloid leukemia patients after first relapse: a single center experience. Ann Oncol 7:933–938
Wierzbowska A, Robak T, Pluta A, Wawrzyniak E, Cebula B, Hołowiecki J, Kyrcz-Krzemień S, Grosicki S, Giebel S, Skotnicki AB, Piatkowska-Jakubas B, Kuliczkowski K, Kiełbiński M, Zawilska K, Kłoczko J, Wrzesień-Kuś A, Polish Adult Leukemia Group (2008) Cladribine combined with high doses of arabinoside cytosine, mitoxantrone, and G-CSF (CLAG-M) is a highly effective salvage regimen in patients with refractory and relapsed acute myeloid leukemia of the poor risk: a final report of the Polish Adult Leukemia Group. Eur J Haematol 80:115–126
Yavuz S, Paydas S, Disel U, Sahin B (2006) IDA-FLAG regimen for the therapy of primary refractory and relapse acute leukemia: a single-center experience. Am J Ther 13:389–393
Jin J, Jiang DZ, Mai WY, Meng HT, Qian WB, Tong HY, Huang J, Mao LP, Tong Y, Wang L, Chen ZM, Xu WL (2006) Homoharringtonine in combination with cytarabine and aclarubicin resulted in high complete remission rate after the first induction therapy in patients with de novo acute myeloid leukemia. Leukemia 20:1361–1367
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C (1985) Proposed revised criteria for the classification of acute myeloid leukemia. Ann Intern Med 103:620–625
Yates J, Glidewell O, Wiernik P, Cooper MR, Steinberg D, Dosik H, Levy R, Hoagland C, Henry P, Gottlieb A, Cornell C, Berenberg J, Hutchison JL, Raich P, Nissen N, Ellison RR, Frelick R, James GW, Falkson G, Silver RT, Haurani F, Green M, Henderson E, Leone L, Holland JF (1982) Cytosine arabinoside with daunorybicin or adriamycin therapy with acute myelocytic leukemia: a CALGB study. Blood 60:454–463
World Health Organization (1979) A Handbook for Reporting Results of Cancer Treatment. WHO Publications, Geneva
Kong XB, Fanucchi MP, Chou TC (1988) Antagonistic interactions of hexamethylene bisacetamide in combination with 1-beta-D-arabinofuranosylcytosine, adriamycin and harringtonine on the growth and differentiation of HL-60 cells in vitro. Leuk Res 12:853–859
Bian SG, Hao YS, Wang ZC (1990) Analysis of the therapeutic efficacy and prognostic factors of intensive chemotherapy in 91 patients with acute nonlymphoblastic leukemia. Chung Hua Nei Ko Tsa Chih 29:22–25
Takahashi I, Hara M, Uchida K, Takaoka K, Watanabe S, Lai M, Hamasaki K, Kohi F, Kitajima K, Kimura I, Adachi T, Yorimitsu S, Tokioka M, Sanada H (1982) Treatment of relapsed acute myelocytic leukemia with a combination of aclarubicin and cytosine arabinoside. Acta Med Okayama 36:77–80
Steinmetz HT, Schulz A, Staib P, Scheid C, Glasmacher A, Neufang A, Franklin J, Tesch H, Diehl V, Dias Wickramanayake P (1999) Phase-II trial of idarubicin, fludarabine, cytosine arabinoside, and filgrastim (Ida-FLAG) for treatment of refractory, relapsed, and secondary AML. Ann Hematol 78:418–425
Jackson G, Taylor P, Smith GM, Marcus R, Smith A, Chu P, Littlewood TJ, Duncombe A, Hutchinson M, Mehta AB, Johnson SA, Carey P, MacKie MJ, Ganly PS, Turner GE, Deane M, Schey S, Brookes J, Tollerfield SM, Wilson MP (2001) A multicenter, open, non-comparative phase II study of a combination of fludarabine phosphate, cytarabine and granulocyte colony-stimulating factor in relapsed and refractory acute myeloid leukemia and de novo refractory anemia with excess of blasts in transformation. Br J Haematol 112:127–137
List AF, Kopecky KJ, Willman CL, Head DR, Persons DL, Slovak ML, Dorr R, Karanes C, Hynes HE, Doroshow JH, Shurafa M, Appelbaum FR (2001) Benefit of cyclosporine modulation of drug resistance in patients with poor-risk acute myeloid leukemia: a Southwest Oncology Group study. Blood 98:3212–3220
Wrzesień-Kuś A, Robak T, Wierzbowska A, Lech-Marańda E, Pluta A, Wawrzyniak E, Krawczyńska A, Kuliczkowski K, Mazur G, Kiebiński M, Dmoszyńska A, Wach M, Hellmann A, Baran W, Hołowiecki J, Kyrcz-Krzemień S, Grosicki S, Polish Adult Leukemia Group (2005) A multicenter, open, noncomparative, phase II study of the combination of cladribine (2-chlorodeoxyadenosine), cytarabine, granulocyte colony-stimulating factor and mitoxantrone as induction therapy in refractory acute myeloid leukemia: a report of the Polish Adult Leukemia Group. Ann Hematol 84:557–564
Huhmann IM, Watzke HH, Geissler K, Gisslinger H, Jäger U, Knöbl P, Pabinger I, Korninger L, Mannhalter C, Mitterbauer G, Schwarzinger I, Kalhs P, Haas OA, Lechner K (1996) FLAG (fludarabine, cytosine arabinoside, G-CSF) for refractory and relapsed acute myeloid leukemia. Ann Hematol 73:265–271
Thomas X, Fenaux P, Dombret H, Delair S, Dreyfus F, Tilly H, Vekhoff A, Cony-Makhoul P, Leblond V, Troussard X, Cordonnier C, de Revel T, Simon M, Nicolini F, Stoppa AM, Janvier M, Bordessoule D, Rousselot P, Ffrench M, Marie JP, Archimbaud E (1999) Granulocyte-macrophage colony-stimulating factor (GM-CSF) to increase efficacy of intensive sequential chemotherapy with etoposide, mitoxantrone and cytarabine (EMA) in previously treated acute myeloid leukemia: a multicenter randomized placebo-controlled trial (EMA91 Trial). Leukemia 13:1214–1220
Liu Yin JA, Wheatley K, Rees JK, Burnett AK, UK MRC Adult Leukemia Working Party (2001) Comparison of 'sequential' versus 'standard' chemotherapy as re-induction treatment, with or without cyclosporine, in refractory/relapsed acute myeloid leukaemia (AML): results of the UK Medical Research Council AML-R trial. Br J Haematol 113:713–726
Weltermann A, Fonatsch C, Haas OA, Greinix HT, Kahls P, Mitterbauer G, Jäger U, Kainz B, Geissler K, Valent P, Sperr WR, Knöbl P, Schwarzinger I, Gleiss A, Lechner K (2004) Impact of cytogenetics on the prognosis of adults with de novo AML in first relapse. Leukemia 18:293–302
Breems DA, Van Putten WL, Huijgens PC, Ossenkoppele GJ, Verhoef GE, Verdonck LF, Vellenga E, De Greef GE, Jacky E, Van der Lelie J, Boogaerts MA, Löwenberg B (2005) Prognostic index for adult patients with acute myeloid leukemia in first relapse. J Clin Oncol 23:1969–1978
Ferrara F, Palmieri S, Mele G (2004) Prognostic factors and therapeutic options for relapsed or refractory acute myeloid leukemia. Haematologica 89:998–1008
Kern W, Schoch C, Haferlach T, Braess J, Unterhalt M, Wormann B, Buchner T, Hiddemann W, for the German AML Cooperative Group (2000) Multivariate analysis of prognostic factors in patients with refractory and relapsed acute myeloid leukemia undergoing sequential high-dose cytosine arabinoside and mitoxantrone (S-HAM) salvage therapy: relevance of cytogenetic abnormalities. Leukemia 14:226–231
Estey E (2000) Treatment of relapsed and refractory acute myelogenous leukemia. Leukemia 14:476–479
Chevallier P, Labopin M, Turlure P, Prebet T, Pigneux A, Hunault M, Filanovsky K, Cornillet-Lefebvre P, Luquet I, Lode L, Richebourg S, Blanchet O, Gachard N, Vey N, Ifrah N, Milpied N, Harousseau JL, Bene MC, Mohty M, Delaunay J (2011) A new Leukemia Prognostic Scoring System for refractory/relapsed adult acute myelogeneous leukaemia patients: a GOELAMS study. Leukemia 25:939–944
Acknowledgments
This work was supported by National Natural Science Foundation of China (Grant #30900641), Science Research Fundation of Health Department of Zhejiang Province (Grant #2008B063 and Grant #2009B046) and Research Fund for the Doctoral Program of Higher Education of China (Grant #20090101120112).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, W., Mao, L., Qian, J. et al. Homoharringtonine in combination with cytarabine and aclarubicin in the treatment of refractory/relapsed acute myeloid leukemia: a single-center experience. Ann Hematol 92, 1091–1100 (2013). https://doi.org/10.1007/s00277-013-1758-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1758-5