Abstract
High-dose chemotherapy (HDT) followed by autologous stem cell transplantation (ASCT) is considered standard in the treatment of patients with relapsed or refractory aggressive peripheral T cell lymphoma (PTCL). However, the optimal salvage regimen before ASCT has not yet been established. We retrospectively analyzed 31 patients with relapsed or refractory aggressive PTCL after anthracycline-based first-line chemotherapy who received either DexaBEAM (dexamethasone, carmustine, etoposide, cytarabine, and melphalan; n = 16) or ICE (ifosfamide, carboplatin, and etoposide; n = 15) regimen as first salvage chemotherapy followed by HDT/ASCT. The overall response rate (OR) was significantly higher for patients treated with DexaBEAM (69 %; 95 % confidence interval 46.0–91.5 %) as compared to the ICE group (20 %; 95 % confidence interval −0.2–40.2 %; P = 0.01), with higher complete response (CR; 38 %; 95 % confidence interval 13.8–61.2 %; vs. 7 %; 95 % confidence interval −6.0–19.6 %) as well as partial response (PR; 31 vs. 13 %) rate. Changing regimen due to failure of first salvage therapy, 12 patients initially receiving ICE still achieved an OR of 58 % (33 % CR, 25 % PR) with DexaBEAM as second salvage therapy, whereas in three patients receiving ICE after DexaBEAM failure, only one achieved an OR (1 PR). Median progression-free survival was significantly higher in the DexaBEAM group (6.4 vs. 2 months; P = 0.01). Major adverse event in both groups was myelosuppression with higher but tolerable treatment-related toxicity for patients in the DexaBEAM group. For all patients proceeding to HDT/ASCT, a 3-year overall survival was 50 %. Together, considering the limitations of the retrospective design of the evaluation and the small sample size, our data suggest that DexaBEAM salvage chemotherapy is superior to ICE for patients with relapsed or refractory aggressive PTCL for remission induction prior to autologous transplantation, with higher but manageable treatment-related toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral T cell lymphomas (PTCL) are a heterogeneous group of aggressive lymphomas. The most common subtypes of this entity are PTCL not otherwise specified (NOS), angioimmunoblastic type (AITL), anaplastic large-cell lymphoma (ALCL), adult T cell leukemia/T cell lymphoma as well as enteropathy-associated T cell lymphoma (EATCL) [1–3]. In aggressive B cell lymphoma, during the last decade, the addition of the anti-CD20 monoclonal antibody rituximab to various chemotherapy regimens has dramatically improved response rates as well as event-free and overall survival [4–6] However, with the exception of ALK+ ALCL, which has 40–50 % long-term survival after anthracycline-based chemotherapy, prognosis of PTCL remains poor with high rates of relapse or refractory disease and a 5-year overall survival usually less than 30 % [7–10]. Due to the lack of sustained success with frontline chemotherapy regimens [3], the majority of PTCL patients will experience progressive disease and require additional therapy. Since the value of high-dose chemotherapy (HDT) and autologous stem cell transplantation (ASCT) in the first initial remission is still controversial in these patients [7], as with aggressive B cell NHL, a general approach to refractory or relapsed PTCL is second-line salvage chemotherapy followed by HDT/ASCT [11–16]. Established salvage regimens achieve overall response (OR) rates between 40 and 70 % in patients with PTCL, and response to salvage therapy is a strong positive predictive factor prior to HDT and ASCT [14, 17, 18]. For relapsed and refractory aggressive B cell NHL, a large prospective randomized trial using common salvage regimens has not shown any superiority for any particular regimen [19]. Moreover, for PTCL, no randomized trials or comparative data are available evaluating the relative efficacy of these salvage therapies before HDT/ASCT. With only 10–15 % of all NHL patients, T cell lymphoma is a rare disease, and case numbers in published data are generally small. Consequently, the optimal salvage therapy still needs to be determined for patients with refractory or relapsed PTCL. Therefore, efforts to identify the best pretransplant salvage chemotherapy regimen, including therapeutic activity, stem cell mobilizing potential, and therapy-associated toxicity, represent challenging issues for these patients. Here, we report on a single-institution retrospective analysis of a relatively small patient cohort comparing the effects of two established salvage therapy regimens, DexaBEAM and ICE, followed by HDT/ASCT, attempting to identify the parameters influencing the feasibility, safety profile, and efficacy.
Patients and methods
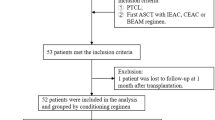
From 1996 to 2009, a total of 35 patients with refractory or relapsed PTCL after anthracycline-based first-line treatment were referred consecutively to the Department of Medicine A of the University Hospital of Muenster, Germany. Patients received either DexaBEAM or ICE as first salvage chemotherapy followed by HDT and ASCT with curative intention. Each patient gave informed consent to the actual treatment approach individually followed. The allocation of the patients to either DexaBEAM or ICE was by coincidence. Patients were treated by one of two different attending physician services within the same department according to vacancy, of which one service favored DexaBEAM and the other ICE, concerning the advantages versus disadvantages of either regimen. All patients had histologically confirmed diagnosis of PTCL according to the WHO criteria [20] and an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2. Staging evaluations at relapse/refractory disease with thoracic and abdominal computed tomography scans and bone marrow biopsy, a glomerular filtration rate of at least 60 ml/min, the absence of hypoxemia as measured by capillary blood gas analysis, and a transfer factor of at least 60 % of normal were prerequisites for eligibility. Based on these criteria, 31 out of the 35 patients (89 %) with refractory or relapsed PTCL were incorporated in the present evaluation; the remaining patients were excluded (e.g., due to severe sepsis at time of relapse and/or ECOG >2). The individual International Prognostic Index (IPI) was determined by the absence or presence of respective risk factors [21, 22]. Details of patient characteristics, prior chemotherapy regimens, disease status at diagnosis and at relapse, response rates after salvage chemotherapy, stem cell harvesting, conditioning regimen previous to ASCT, and follow-up were obtained.
ICE and DexaBEAM salvage regimens
DexaBEAM regimen [23] was given every 22–28 days (depending on peripheral blood cell recovery time and general performance) on an inpatient basis, for two to three cycles. DexaBEAM consisted of 24 mg dexamethasone on days 1 to 10, carmustine 60 mg/m2 on day 2, etoposide 100 mg/m2 on days 4 to 7, cytarabine 100 mg/m2 every 12 h on days 4 to 7, and melphalan 20 mg/m2 on day 3. ICE regimen [24] was given every 15–22 days (depending on peripheral blood cell number recovery time and general performance) on an inpatient basis as well, for two to three cycles. ICE consisted of ifosfamide 5 g/m2 on day 2, carboplatin administered on day 2, and dosed to an area under the curve of 5, and etoposide 100 mg/m2 on days 1 to 3. Granulocyte colony-stimulating factor (G-CSF) was administered from day 12 (DexaBEAM) or 7 (ICE) and until absolute blood neutrophil counts exceeded 1,000/μL or if a sufficient amount of CD34+ cells for stem cell harvest was achieved for peripheral stem cell harvest. Supportive care according to the center’s standard consisted of ciprofloxacin 2 × 500 mg per os (p.o.) and amphotericin B suspension 4 × 2 ml p.o. daily during grade IV neutropenia, prophylactic blood product support, with irradiation of blood products administered during the stem cell mobilizing chemotherapy, antiemetic prophylaxis including 5HT3 antagonists, adequate hydration during chemotherapy, and 2-mercaptoethanesulfonate-Natrium at least 140 % of the ifosfamide dose for hemorrhagic cystitis prevention for patients receiving ICE. Hematological toxicity and side effects related to chemotherapy were evaluated according to WHO criteria.
Assessment of response and definition of endpoints
Response to therapy was assessed by conventional diagnostic methods, including physical examination, computed tomography scans, and bone marrow biopsy if abnormal before treatment. Positron emission tomography scanning was available in some patients but not performed routinely for all patients during the period of this study. Response was assessed using the International Working Group criteria [25, 26]. Complete remission (CR) was defined by the disappearance of all documented disease; unconfirmed CR (CRu) was used when a residual mass was present without evidence of active disease. Partial response (PR) was defined as a >50 % volume reduction of measurable disease lasting >1 month. Any response less than PR was considered stable disease (SD); increase in size of lesion >50 %, occurrence of new lesions, and/or progress of initial symptoms was labeled as progressive disease (PD). OR included patients with CR, CRu, and PR. Response was assessed after the second and, if administered, the third cycle of salvage therapy and after HDT/ASCT. Overall survival (OS) was counted from the first day of salvage therapy until death of any course, with patients censored at the last time point known to be alive. Progression-free survival (PFS) was defined as the time interval from initiation of first salvage therapy until disease progression or death.
Number of cycles
Patients with CR or CRu after two cycles of salvage therapy proceeded to HDT/ASCT, whereas patients with PR after two cycles received a third cycle, and patients with SD or PD received an alternative therapy. At least PR was required as the best response to proceed to HDT/ASCT.
High-dose chemotherapy and autologous stem cell transplantation
Mobilization and collection of peripheral blood stem cells (PBSCs) were carried out using s.c. G-CSF administration after the first course of salvage therapy if possible. In case of bone marrow infiltration, stem cell mobilization was performed after histologically confirmed clearance of the lymphoma in the bone marrow. The minimum threshold of PBSCs to proceed to ASCT was 2 × 106 CD34+ cells/kg body weight. If response to first salvage regimen was less than very good PR, patients were switched either from DexaBEAM to ICE or vice versa, or to a different salvage regimen. Patients who achieved at least PR after the second salvage treatment were also referred to HDT as well. HDT before ASCT consisted of BEAM (carmustine 300 mg/m2 on day 6, etoposide 100 mg/m2 every 12 h on days 6 to 3, cytarabine 200 mg/m2 every 12 h on days 6 to 3, and melphalan 140 mg/m2 on day 2). PBSCs were reinfused on day 0, at least 30 h after completion of BEAM chemotherapy.
Statistical analysis
The primary endpoint taken for this evaluation was response to salvage therapy (OR) after ICE and/or DexaBEAM treatment prior to ASCT. Secondary endpoints were CR/CRu rate, OS, and PFS, as well as toxicity of the two salvage regimens. Data are presented as descriptive values and percentages or median values and ranges, when appropriate. Comparisons of categorical variables were performed by chi-square test and of continuous variables by Mann–Whitney U test. Survival data were estimated by the Kaplan–Meier method and compared using log rank test. All variables showing a two-sided P value <0.05 were considered as indicating statistically significant differences. For data analysis, a computer-based statistical package PASW Statistics 18.0 (IBM Corp.) was used.
Results
Characteristics of patients
Patient characteristics are listed in Table 1. Thirty-one patients with relapsed or refractory PTCL after cyclophosphamide–hydroxydaunorubicin–oncovin–prednisone (CHOP) or CHOP-like first-line chemotherapy were treated with either DexaBEAM (n = 16; 8 females; median age 46 years; range 18–66) or ICE (n = 15; 8 females; median age 40 years; range 17–59) salvage therapy. PTCL (NOS) was the most frequent histological subtype in both groups (44 % of patients in the DexaBEAM group and 40 % of patients in the ICE group). The number of chemotherapy cycles administered was similar in both groups with 16 patients receiving 38 cycles of DexaBEAM and 15 patients receiving 28 cycles of ICE regimen (P = 0.16).
Response to treatment
OR, including CR, CRu, and PR, was achieved after first salvage therapy by 69 % (95 % confidence interval 46.0–91.5 %) of patients in the DexaBEAM group as compared to 20 % of patients in the ICE group (95 % confidence interval −0.2–40.2 %; P = 0.01). Both CR (38 %; 95 % confidence interval 13.8–61.2 %; vs. 7 %; 95 % confidence interval −6.0–19.6 %; P = 0.08) and PR rates (31 vs. 13 %, P = 0.39) were higher in patients treated with DexaBEAM as compared to the ICE regimen. One patient (6 %) achieved very good partial response (VGPR) after DexaBEAM regimen. In contrast, SD and PD after first salvage therapy were observed in 31 % in the DexaBEAM group and 80 % in the ICE group (P = 0.01). Among the patients with ALK+ ALCL or ALCL with unknown ALK status representing a subgroup with potentially more favorable prognosis in the DexaBEAM group, three patients achieved OR (CR, one patient; PR, two patients), whereas PD was observed in three patients. Exclusion of patients with ALK+ ALCL and ALCL with unknown ALK status did not change the results. OR was achieved after first salvage therapy by 80 % (95 % confidence interval 55.2–104.8 %) of these patients in the DexaBEAM group as compared to 20 % in the ICE group (P = 0.005). Again, both CR (50 %, 95 % confidence interval 19.0–81.0, vs. 7 %; P = 0.023) and PR rates (30 vs. 13 %, P = 0.358) were higher in patients treated with DexaBEAM as compared to the ICE regimen.
HDT with ASCT could be administered in 8 of 11 patients with response to DexaBEAM salvage therapy and in all 3 patients with response to ICE salvage therapy. All 12 patients not responding to ICE salvage therapy were switched to DexaBEAM third-line therapy. Interestingly, 59 % of these patients (n = 7) achieved CR (33 %, n = 4) or PR (25 %, n = 3), and six of these patients were then referred to HDT/ASCT. In contrast, three patients with response failure after DexaBEAM first salvage regimen were switched to ICE third-line therapy. One of these patients achieved PR, but HDT/ASCT could not be performed due to reduced performance status, and the patient finally experienced PD. The two other patients did not achieve any measurable response after ICE third-line therapy and could not be treated with HDT/ASCT.
Survival
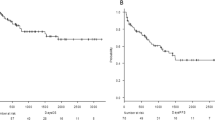
Among all 16 patients treated with DexaBEAM as first salvage regimen, median PFS from the start of salvage therapy was 6.4 months (95 % confidence interval 8.6 to 32.3 months). Median PFS among all 15 patients treated with ICE as first salvage regimen was significantly shorter (2 months; 95 % confidence interval 0.03 to 15.8 months; P = 0.01) (Fig. 1a). Two-year PFS was 40 % in the DexaBEAM group and 7 % in the ICE group (P = 0.04). OS was not significantly different between the two groups. Median OS was 22.8 months in the DexaBEAM group (95 % confidence interval 17.4 to 50.5 months) and 29.8 months in the ICE group (95 % confidence interval 20.3 to 57.3 months; P = 0.72) (Fig. 1b). Four-year OS was 33 % in the DexaBEAM group and 43 % in the ICE group (P = 0.26). For all patients proceeding to ASCT, OS was not different irrespective of first-line salvage therapy (data not shown). Patients receiving HDT and ASCT had a median relapse-free survival of 23.4 months and median OS of 37.3 months. Three-year OS of all patients receiving HDT/ASCT was 50 %.
Progression-free (a) and overall (b) survival after DexaBEAM or ICE first salvage therapy regimen. Survival curves of both patient groups are depicted in one figure although this was not a randomized prospective study but a retrospective analysis of two patient cohorts with allocation by coincidence
Adverse events
Adverse events related to either DexaBEAM or ICE chemotherapy are listed in Table 2. The major adverse event after both regimens was myelosuppression. One patient in the DexaBEAM group died due to sepsis in CR after HDT/ASCT. Toxicity was further increased for patients receiving DexaBEAM third-line chemotherapy after ICE salvage regimen, with longer duration of chemotherapy-induced neutropenia, 100 % leukocytopenia, and thrombocytopenia of WHO grade III/IV, 85 % anemia of WHO grade III and IV, and increased occurrence of mucositis of all WHO grades, most likely due to cumulative toxicity of the different chemotherapy regimens (data not shown). Altogether, adverse events after both salvage chemotherapy regimens were manageable, even after third-line application, and no treatment-related death occurred.
Discussion
PTCLs are often refractory to anthracyclines [3], and standard first-line chemotherapies can usually achieve long-term survival of only 12–45 % [2]. Value of HDT and ASCT in the first initial remission is still controversial in these patients [7, 16, 17, 27, 28]. Thus, in PTCL, two populations are candidates for salvage treatment followed by HDT and ASCT: patients who experience a relapse after achieving CR and those who do not achieve CR after first-line therapy. One large randomized trial comparing two established salvage regimens in patients with relapsed or refractory aggressive B cell lymphoma did not show any benefit for one or the other regimen [19], and for relapsed or refractory PTCL, no randomized trial or comparative analysis of any salvage regimens has ever been reported previously. Thus, no data are available which salvage regimen is preferable for these patients in terms of efficacy and toxicity. Definite efficacy of salvage therapy, however, is ultimately dependent on the possibility to perform following HDT/ASCT. This option in turn depends on the response rate and toxicity of the prior salvage regimen chosen.
The present retrospective study analyzed the efficacy and safety of two established salvage chemotherapy regimens, DexaBEAM and ICE, prior to HDT and ASCT, for aggressive relapsed or refractory PTCL in two patient groups with allocation of the patient to either regimen by coincidence. Notably, OR rate as well as PFS in the DexaBEAM group were markedly superior compared to the ICE group. Our results do not show any advantage for patients initially treated with DexaBEAM in terms of OS, but we assume that this may be due to the good response rate of patients treated with DexaBEAM second salvage chemotherapy after response failure to ICE regimen. Disease status after salvage therapy and prior to HDT/ASCT is one of the strongest prognostic predictors for survival of patients with relapsed or refractory aggressive B and T cell NHL [14, 17, 18]. Our findings demonstrate the potential benefit of patients with relapsed or refractory PTCL treated with DexaBEAM salvage therapy prior to HDT and ASCT versus patients treated with ICE salvage therapy. However, our results should be considered with caution since our data may have been influenced by the substantial biases associated with patient allocation—this is no prospective randomized comparison—and with retrospective analysis of relatively small patient cohorts. We still believe that our single-center data provide a basis for future prospective studies of salvage chemotherapy regimens for relapsed or refractory PTCL. Another potential caveat in our evaluation was the higher incidence of patients with the potentially more favorable entity ALCL, ALK+, and ALCL, ALK status unknown, in the DexaBEAM group. Nevertheless, even an exclusion of these patients did not influence the superiority of DexaBEAM compared to ICE. The response rate in the DexaBEAM group was also superior to response rates to other salvage regimens for patients with relapsed or refractory PTCL in previous reports [29–31]. However, comparison with other studies is difficult in most cases since most other studies included both relapsed/refractory B and T cell lymphoma, and numbers of PTCL patients in these studies are usually very low.
Interestingly, of 12 patients with response failure to ICE salvage regimen, seven patients (58 %) still responded to DexaBEAM second salvage chemotherapy (four CR, three PR), offering the chance of subsequent HDT and ASCT treatment with potential cure of the disease. Thus, DexaBEAM may still be a promising option even for PTCL patients after failure of two chemotherapy regimens. However, the facts that PFS is significantly better in patients treated with DexaBEAM first salvage chemotherapy than among those treated with ICE and that toxicity is further increased in patients receiving DexaBEAM as second salvage therapy suggests that the application of DexaBEAM as first salvage regimen is preferable.
Adverse events were more severe in the DexaBEAM group. However, all adverse events were manageable with supportive therapies, and no treatment-related deaths after salvage therapy occurred in any of the two groups.
In conclusion, taking the limitations of the retrospective nature of the analysis and the small sample size into account, our data suggest that DexaBEAM is superior to ICE as salvage chemotherapy for relapsed or refractory PTCL to induce effective disease remission and to enable HDT and ASCT. DexaBEAM may even be suitable as third-line chemotherapy for these patients after failure of initial salvage regimens but reduced toxicity when used as second-line therapy seems to favor early application. However, before a firm therapy recommendation can be made, further prospective studies using larger patient cohorts and including other salvage regimens, as well as new targeted therapies [1, 6, 32–37] are required to establish optimal clinical strategies for relapsed and refractory PTCL.
References
Foss FM, Zinzani PL, Vose JM, Gascyone RD, Rosen ST, Tobinai K (2011) Peripheral T-cell lymphoma. Blood 117:6756–6767
Shankland KR, Armitage JO, Hancock BW (2012) Non-Hodgkin lymphoma. Lancet 380:848–857
Vose J, Armitage J, Weisenburger D (2008) International T-Cell Lymphoma Project. International peripheral T-Cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol 26:4124–4130
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242
Habermann TM, Weller EA, Morrison VA, Gascoyne RD, Cassileth PA, Cohn JB, Dakhil SR, Woda B, Fisher RI, Peterson BA, Horning SJ (2006) Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol 24:3121–3127
Pfreundschuh M, Ho AD, Cavallin-Stahl E, Wolf M, Pettengell R, Vasova I, Belch A, Walewski J, Zinzani PL, Mingrone W, Kvaloy S, Shpilberg O, Jaeger U, Hansen M, Corrado C, Scheliga A, Loeffler M, Kuhnt E, MabThera International trial (MInT) Group (2008) Prognostic significance of maximum tumour (bulk) diameter in young patients with good-prognosis diffuse large-B-cell lymphoma treated with CHOP-like chemotherapy with or without rituximab: an exploratory analysis of the MabThera International Trial Group (MInT) study. Lancet Oncol 9:435–444
Armitage JO (2012) The aggressive peripheral T-cell lymphomas: 2012 update on diagnosis, risk stratification, and management. Am J Hematol 87:511–519
Federico M, Rudiger T, Bellei M, Nathwani BN, Luminari S, Coiffier B, Harris NL, Jaffe ES, Pileri SA, Savage KJ, Weisenburger DD, Armitage JO, Mounier N, Vose JM (2013) Clinicopathologic characteristics of angioimmunoblastic T-cell lymphoma (AITL): analysis of 243 cases from the International Peripheral T-cell Lymphoma Project. J Clin Oncol 31:240–246
Ferreri AJ, Govi S, Pileri SA, Savage KJ (2012) Anaplastic large cell lymphoma, ALK positive. Crit Rev Oncol Hematol 83:293–302
Savage KJ, Harris NL, Vose JM, Ullrich F, Jaffe ES, Connors JM, Rimsza L, Pileri SA, Chhanabhai M, Gascoyne RD, Armitage JO, Weisenburger DD, International Peripheral T-Cell Lymphoma Project (2008) ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International T-Cell Lymphoma Project. Blood 111:5496–5504
Greer JP (2006) Therapy of peripheral T/NK neoplasm. Hematol Am Soc Hematol Educ Program 2006:331–337
Philip T, Guglielmini C, Hagenbeek A, Somers R, Van der Lelie H, Bron D, Sonneveld P, Gisselbrecht C, Cahn JY, Harousseau et al (1995) Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin’s lymphoma. N Engl J Med 333:1540–1545
Gutiérrez A, Caballero MD, Pérez-Manga G, Rodriguez J (2008) Hematopoietic SCT for peripheral T-cell lymphoma. Bone Marrow Transplant 42:773–781
Kyriakou C, Canals C, Goldstone A, Caballero D, Metzner B, Kobbe G, Kolb HJ, Kienast J, Reimer P, Finke J, Oberg G, Hunter A, Theorin N, Sureda A, Schmitz N, Outcome-Lymphoma Working Party of the European Group for Blood and Marrow Transplantation (2008) High-dose therapy and autologous stem-cell transplantation in angioimmunoblastic lymphoma: complete remission at transplantation is the major determinant of Outcome-Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 26:218–224
Hosing C, Champlin RE (2011) Stem-cell transplantation in T-cell non-Hodgkin lymphomas. Ann Oncol 22:1471–1477
Schetelig J, Fetscher S, Reichle A, Berdel WE, Beguin Y, Brunet S, Caballero D, Majolino I, Hagberg H, Johnsen HE, Kimby E, Montserrat E, Stewart D, Copplestone A, Rösler W, Pavel J, Kingreen D, Siegert W (2003) Long-term disease-free survival in patients with angioimmunoblastic T-cell lymphoma after high-dose chemotherapy and autologous stem cell transplantation. Haematologica 88:1272–1278
Kim MK, Kim S, Lee SS, Sym SJ, Lee DH, Jang S, Park CJ, Chi HS, Huh J, Suh C (2007) High-dose chemotherapy and autologous stem cell transplantation for peripheral T-cell lymphoma: complete response at transplant predicts survival. Ann Haematol 86:435–442
Rodríguez J, Caballero MD, Gutiérrez A, Marin J, Lahuerta JJ, Sureda A, Carreras E, Leon A, Arranz R, Fernandez de Sevilla A, Zuazu J, Garcia-Larana J, Rifon J, Varela R, Gandarillas M, SanMiguel J, Conde (2003) High dose chemotherapy and autologous stem cell transplantation in peripheral T-cell lymphoma: the GEL-TAMO experience. Ann Oncol 14:1768–1775
Gisselbrecht C, Glass B, Mounier N, Singh Gill D, Linch DC, Trneny M, Bosly A, Ketterer N, Shpilberg O, Hagberg H, Ma D, Briere J, Moskowitz CH, Schmitz N (2010) Salvage regimens with autologous transplantation for relapsed large cell lymphoma in the rituximab era. J Clin Oncol 28:4184–4190
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW (2008) WHO classification of tumours of haematopoietic and lymphoid tissues. IARC, Lyon
Blay J, Gomez F, Sebban C, Bachelot T, Biron P, Guglielmi C, Hagenbeek A, Somers R, Chauvin F, Philip T (1998) The International Prognostic Index correlates to survival in patients with aggressive lymphoma in relapse: analysis of the PARMA trial. Parma Group. Blood 92:3562–3568
Hamlin PA, Zelenetz AD, Kewalramani T, Qin J, Satagopan JM, Verbel D, Noy A, Portlock CS, Straus DJ, Yahalom J, Nimer SD, Moskowitz CH (2003) Age-adjusted International Prognostic Index predicts autologous stem cell transplantation outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. Blood 102:1989–1996
Atta J, Chouw KU, Weidmann E, Mitrou PS, Hoelzer D (2007) Martin H (2007) DexaBEAM as salvage therapy in patients with primary refractory aggressive non-Hodgkin lymphoma. Leuk Lymphoma 48:349–356
Zelenetz AD, Hamlin P, Kewalramani T, Yahalom J, Nimer S, Moskowitz CH (2003) Ifosfamide, carboplatin, etoposide (ICE)-based second-line chemotherapy for the management of relapsed and refractory aggressive non-Hodgkin’s lymphoma. Ann Oncol Suppl 1:i5–i10
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippenstein D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17:1244–1253
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Diehl V, International Harmonization Project on Lymphoma (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25:579–586
Chen AI, McMillan A, Negrin RS, Horning SJ, Laport GG (2008) Long-term results of autologous hematopoietic cell transplantation for peripheral T cell lymphoma: the Stanford experience. Biol Blood Marrow Transplant 14:741–747
D’Amore F, Relander T, Lauritzsen GF, Jantunen E, Hagberg H, Anderson H, Holte H, Österborg A, Merup M, Brown P, Kuittinen O, Erlanson M, Ostenstad B, Fagerli UM, Gadeberg OV, Sundström C, Delabie J, Ralfkiaer E, Vornanen M, Toldbod HE (2012) Up-front autologous stem cell transplantation in peripheral T-cell lymphoma: NLG-T-01. J Clin Oncol 30:3093–3099
Josting A, Sienawski M, Glossmann JP, Staak O, Nogova L, Peters N, Mapara M, Dörken B, Ko Y, Metzner B, Kisro J, Diehl V, Engert A (2005) High-dose sequential chemotherapy followed by autologous stem cell transplantation in relapsed and refractory aggressive non-Hodgkin’s lymphoma: results of a multicenter phase II study. Ann Oncol 16:1359–1365
Kim KH, Joo YD, Sohn CH, Shin HJ, Chung JS, Cho GJ, Shin SH, Kim YS, Lee WS (2009) Gemcitabine, etoposide, cisplatin, and dexamethasone in patients with refractory or relapsed non-Hodgkin’s lymphoma. Korean J Intern Med 24:37–42
Park BB, Kim WS, Lee J, Park KW, Kang JH, Lee SH, Park JO, Kim K, Jung CW, Park YS, Im YH, Kang WK, Ko YH, Lee MH, Park K (2005) IMVP-16/Pd followed by high-dose chemotherapy and autologous stem cell transplantation as a salvage therapy for refractory or relapsed peripheral T-cell lymphomas. Leuk Lymphoma 46:1743–1748
Pro B, Advani RH, Brice P, Bartlett NL, Rosenblatt JD, Illidge T, Matous J, Ramchandren R, Fanale M, Connors JM, Yang Y, Sievers EL, Kennedy DA, Shustov A (2012) Brentuximab vedotin (SGN-35) in patients with relapsed of refractory systemic anaplastic large cell lymphoma: results of a phase II study. J Clin Oncol 30:2190–2196
Coiffier B, Pro B, Prince HM, Foss F, Sokol L, Greenwood M, Caballero D, Borchmann P, Morschhauser F, Wilhelm M, Pinter-Brown L, Padmanabhan S, Shustov A, Nichols J, Carroll S, Balser J, Balser B, Horwitz S (2012) Results from a pivotal, open-label, phase II study of romidepsin in relapsed or refractory peripheral T-cell lymphoma after prior systemic therapy. J Clin Oncol 30:631–636
Enblad G, Hagberg H, Erlanson M, Lundin J, MacDonald AP, Repp R, Schetelig J, Seipelt G, Osterborg A (2004) A pilot study of alemtuzumab (anti-CD52 monoclonal antibody) therapy for patients with relapsed or chemotherapy-refractory peripheral T-cell lymphomas. Blood 103:2920–2924
Gallamini A, Zaja F, Patti C, Billio A, Specchia MR, Tucci A, Levis A, Manna A, Secondo V, Rigacci L, Pinto A, Iannitto E, Zoli V, Torchio P, Pileri S, Tarella C (2007) Alemtuzumab (Campath-1H) and CHOP chemotherapy as first-line treatment of peripheral T-cell lymphoma: results of a GITIL (Gruppo Italiano Terapie Innovative nei Linfomi) prospective multicenter trial. Blood 110:2316–2323
Kim SJ, Kim K, Kim BS, Suh C, Huh J, Ko YH, Kim WS (2009) Alemtuzumab and DHAP (A-DHAP) is effective for relapsed peripheral T-cell lymphoma, unspecified: interim results of a phase II prospective study. Ann Oncol 20:390–392
Prichard M, Harris T, Williams ME, Densmore JJ (2009) Treatment strategies for relapsed and refractory aggressive non-Hodgkin’s lymphoma. Expert Opin Pharmacother 10:983–995
Conflict of Interest
The authors have declared no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
J.H.M. and M.K. contributed equally to the manuscript and share the first authorship. N.H.T. and W.E.B. contributed equally to the manuscript and share senior authorship.
Rights and permissions
About this article
Cite this article
Mikesch, JH., Kuhlmann, M., Demant, A. et al. DexaBEAM versus ICE salvage regimen prior to autologous transplantation for relapsed or refractory aggressive peripheral T cell lymphoma: a retrospective evaluation of parallel patient cohorts of one center. Ann Hematol 92, 1041–1048 (2013). https://doi.org/10.1007/s00277-013-1738-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1738-9