Abstract
Two DNA methyltransferase inhibitors, azacitidine and decitabine, are currently approved for the treatment of myelodysplastic syndrome (MDS). Choosing between these drugs is an important practical issue. In this retrospective study, patients receiving AZA-7d (azacitidine 75 mg/m2 subcutaneously × 7 days, n = 75) or DEC-5d (decitabine 20 mg/m2 intravenously × 5 days, n = 74) were compared. The rates of hematologic response (complete response [CR]/partial response [PR]/marrow CR) were 12.0 % (AZA-7d) vs. 29.7 % (DEC-5d) (P = 0.008), and the overall response rates (CR/PR/marrow CR/hematologic improvement) were 52.0 % (AZA-7d) vs. 63.5 % (DEC-5d) (P = 0.155). Grade 3 or higher neutropenia occurred more frequently with DEC-5d (79.6 %) than with AZA-7d (72.2 %) (P = 0.040). Overall survival probabilities at 2 years were 42.1 % (AZA-7d) vs. 42.2 % (DEC-5d) (P = 0.944). Subgroup analysis revealed that AZA-7d associated with higher survival rates than DEC-5d in patients whose MDS duration exceeded 1 year or who had poor performance status. In conclusion, both AZA-7d and DEC-5d regimens were effective in treating patients with MDS. However, the two regimens differed in terms of clinical responses and toxicities. One hypomethylating regimen may be superior to the other regimen in particular subgroups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Two DNA methyltransferase inhibitors, azacitidine and decitabine, are currently approved for the treatment of myelodysplastic syndrome (MDS) although decitabine is not yet approved in Europe. Phase II and III trials have demonstrated the safety and efficacy of both agents [2, 10, 11, 17, 24–26, 29, 30]. Azacitidine can prolong the overall survival of patients with higher risk MDS [2] and decitabine can increase the time to acute myeloid leukaemia (AML) evolution or death [2, 10]. The standard regimen for azacitidine is 75 mg/m2 by subcutaneous injection daily for 7 days repeated every 4 weeks [2, 24, 25]. In the case of decitabine, the regimen that was approved initially is 15 mg/m2 by intravenous infusion over 3 h, every 8 h, over 3 days and repeated every 6 weeks (3-day regimen) [10]. However, the most widely used decitabine regimen is 20 mg/m2 by intravenous infusion over 1 h daily for 5 days repeated every 4 weeks (5-day regimen). This regimen is more common than the 3-day regimen because it can be given in an outpatient setting and is thus more convenient; it is also associated with higher complete response (CR) rates than the 3 day regimen [11, 13, 26].
The use of DNA methyltransferase inhibitors to treat MDS is now widespread. However, an important practical issue that has not yet been resolved remains: once the decision to administer a hypomethylating agent has been made, which drug should be chosen for a particular patient? Two meta-analyses comparing the two hypomethylating agents [5, 12] that included the same four randomised controlled trials (two trials each for azacitidine [2, 25] and decitabine [10, 15]) showed that azacitidine but not decitabine improved survival. However, although the two randomised trials with decitabine failed to show a survival benefit, this may reflect the use of a suboptimal decitabine regimen: both trials used the 3-day regimen, which appears to be inferior to the currently used 5-day regimen in terms of response rates and overall survival [11, 13, 26]. Furthermore, the impact of azacitidine or decitabine on survival in lower risk patients with MDS is not yet known [27]. Prospective or retrospective studies that compare the 7-day regimen of azacitidine (AZA-7d) and the 5-day regimen of decitabine (DEC-5d) have not yet been performed. Such studies would help to guide the choice between the two hypomethylating agents in clinical practice.
In this retrospective study, the MDS treatments, AZA-7d and DEC-5d, were compared with regard to treatment response, toxicity and survival.
Subjects and methods
Patients
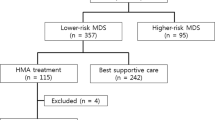
Between September, 2006 and October, 2010, 149 patients with MDS (including chronic myelomonocytic leukaemia [CMML]) were treated with azacitidine (n = 75) or decitabine (n = 74) in three Korean institutes (Asan Medical Center, Seoul; Busan Baek Hospital, Busan; Haeundae Baek Hospital, Busan); all are included in this analysis. All patients had an International Prognostic Scoring System (IPSS) score of 0.5 or more. All patients were treated with azacitidine between September, 2006 and July, 2008, when azacitidine only was approved in Korea. Thereafter, the choice between azacitidine and decitabine was made according to attending physician’s preference.
Treatment and evaluation
Azacitidine 75 mg/m2/day was administered as a subcutaneous injection for seven consecutive days (AZA-7d) and decitabine 20 mg/m2/day as a 1 h intravenous infusion for five consecutive days (DEC-5d). Both regimens were repeated every 4 weeks on an outpatient basis. Prophylactic antimicrobial agents and haematopoietic growth factors were given on the basis of the attending physician’s decision. The treatment response to hypomethylating agents was assessed by a central reviewer who used modified International Working Group (IWG 2006) response criteria [1]. The overall response rate was calculated and included rates for CR, partial response (PR), marrow CR (mCR) and hematologic improvement (HI). Adverse events were graded according to the Common Toxicity Criteria for Adverse Events version 3.0.
Statistical analysis
The primary objective of this study was to compare AZA-7d and DEC-5d in terms of their ability to treat MDS. The secondary objectives were to identify prognostic factors for treatment response and survival, and to perform subgroup analyses that would identify specific subgroups that demonstrated more beneficial effects with one of the two hypomethylating agents.
The Chi-square test was used to compare categorical variables and the Mann–Whitney U test or Student’s t test was used to compare continuous variables. Survival curves were drawn by using the Kaplan–Meier method, and differences in survival were tested for significance by employing the log-rank test and using censored data. Multivariate analysis was performed by using a stepwise multiple logistic regression for overall response rate and the Cox proportional hazards model for overall survival. Subgroup analysis was performed by using a univariate Cox proportional hazards model to evaluate the effect of hypomethylating drug type on overall survival. All hazard ratios were for patients receiving DEC-5d, as compared to those receiving AZA-7d.
Results
Patient characteristics
Table 1 shows the characteristics of the patients. Their median age was 60 years (range, 23–83). The World Health Organization (WHO) subtype at the time hypomethylating treatment was administered was refractory anaemia (RA) in 18 patients, refractory anaemia with ringed sideroblasts in 2, refractory cytopenia with multilineage dysplasia (RCMD) in 28, refractory cytopenia with multilineage dysplasia and ringed sideroblasts (RCMD-RS) in 5, refractory anaemia with excess of blasts (RAEB)-1 in 46, RAEB-2 in 39, unclassified in 2, and CMML in 9. The IPSS risk category was intermediate-1 in 72 patients, intermediate-2/high in 72, and unknown in five.
Treatment response
The patients received a median of five courses (range, 1–48) of AZA-7d and four courses (range, 1–26) of DEC-5d (P = 0.100) (Table 2). Only six patients were still being treated with AZA-7d (n = 1) or DEC-5d (n = 5) at the time of analysis. The two regimens did not differ significantly in terms of the reasons for discontinuing hypomethylating treatment (Table 2).
Nine patients (12.0 %) who received AZA-7d and 22 patients (29.7 %) who received DEC-5d exhibited hematologic responses (CR/PR/mCR) (P = 0.008) (Table 2). The AZA-7d- and DEC-5d-treated patients did not differ significantly in terms of overall response rate (CR/PR/mCR/HI) (52.0 % vs. 63.5 %, P = 0.155). In lower risk MDS (IPSS Intermediate-1), DEC-5d induced higher overall response rates than AZA-7d (21/32 [65.6 %] vs. 16/40 [40.0 %], P = 0.031), but in higher risk MDS (IPSS Intermediate-2/High), the rates of the two regimens were similar (25/40 [62.5 %] vs. 21/32 [65.6 %], P = 0.784).
Initial response was achieved with a median of two AZA-7d courses (range, 1–6) and one DEC-5d course (range, 1–5) (P = 0.269). A hematologic response was achieved with a median of 5.5 AZA-7d courses (range, 1–6) and two DEC-5d courses (range, 1–9) (P = 0.005).
Adverse events
Adverse events that occurred during the first six courses for all patients were assessed. In total, the adverse events during 584 courses were analysed. The most common adverse events were cytopenia and cytopenia-related infection. Grade 3 or higher anaemia (47.6 %), neutropenia (75.6 %) and thrombocytopenia (56.6 %) were observed frequently. DEC-5d was associated with more frequent grade 3 or higher neutropenia (79.6 %) than AZA-7d (72.2 %) (P = 0.040), but the two regimens had similar incidences of febrile episodes that required intravenous antibiotics (12.4 % with DEC-5d vs. 15.4 % with AZA-7d, P = 0.298). In total, nine episodes (1.6 %) of grade 3 bleeding were observed: 0.6 % with AZA-7d and 2.7 % with DEC-5d (P = 0.054). There were no life-threatening bleeding episodes. In both regimens, grade 3 or higher non-hematologic toxicities were infrequent and reversible.
Survival data
The median follow-up duration of the surviving patients was 60.3 months (range, 11.8–66.6) for AZA-7d and 25.1 months (range 6.6–43.3) for DEC-5d (Table 3). For the AZA-7d and DEC-5d groups, the 2 year overall survival rates were 42.1 % and 42.2 %, respectively (P = 0.944), the 2 year progression-free survival rates were 43.5 % and 50.7 %, respectively (P = 0.517), the 2 year relapse rates after a hematologic response were 44.4 % and 46.3 %, respectively (P = 0.976), and the 2 year AML evolution rates were 33.3 % and 33.6 %, respectively (P = 0.417) (Fig. 1).
In lower risk MDS, the median overall survival was 19.9 months with AZA-7d and 39.1 months with DEC-5d (P = 0.262), while in higher risk MDS, it was 16.8 months with AZA-7d and 14.6 months with DEC-5d (P = 0.382).
Prognostic factor analysis
Univariate analyses were performed to identify prognostic factors for overall response rate and overall survival (Table 4). Multivariate analyses demonstrated that MDS duration of 1 year or less (hazard ratio [HR], 2.703; 95 % confidence interval [CI], 1.188–6.149; P = 0.018) and RBC transfusion independency (HR, 2.844; 95 % CI, 1.422–5.685; P = 0.003) were independent prognostic factors for a higher overall response rate, while age ≥ 60 years (HR, 2.260; 95 % CI, 1.458–3.502; P < 0.001), platelet transfusion dependency (HR, 2.341; 95 % CI, 1.439–3.808; P = 0.001), and IPSS Intermediate-2/High risk (HR, 1.687; 95 % CI, 1.120–2.541; P = 0.012) were independent prognostic factors for lower overall survival.
Subgroup analyses revealed that AZA-7d tended to be superior to DEC-5d in terms of survival in patients with an MDS duration exceeding 1 year (HR, 2.362; 95 % CI, 0.882–6.330; P = 0.087). AZA-7d was significantly superior to DEC-5d in patients with an Eastern Cooperative Oncology Group (ECOG) scale of 2–3 (HR, 3.520; 95 % CI, 1.322–9.367; P = 0.012) (Fig. 2). AZA-7d and DEC-5d did not differ significantly in terms of overall survival in other subgroups.
Subgroup analysis for overall survival. A Cox proportional hazards model was used to estimate hazard ratios and the significance of the comparison for overall survival. The horizontal lines indicate 95 % confidence intervals for the ratios. All hazard ratios are for patients receiving decitabine compared to those receiving azacitidine. No. pts number of patients, m month, AZA-7d 7-day regimen of azacitidine, DEC-5d 5-day regimen of decitabine, MDS myelodysplastic syndrome, IPSS International Prognostic Scoring System, INT intermediate
Discussion
Azacitidine and decitabine are structurally related azanucleosides: azacitidine is a ribonucleoside and decitabine is a deoxyribonucleoside [16]. When applied at low doses, both agents reduce genomic DNA methylation by incorporating into newly synthesised DNA and then binding irreversibly to DNA methyltransferases [8]. The demethylation leads to the reactivation of silenced tumour suppressor genes and accounts, at least in part, for the antitumoural effects of the azanucleosides [32]. At high doses, azacitidine and decitabine are cytotoxic, as they cause chain termination and double-strand breaks [21]. DNA methyltransferase 1 may play a role in mediating the DNA damage response to the agents [19]. Although the mechanisms of action of azacitidine and decitabine are related in that they deplete DNA methyltransferases, several lines of evidence suggest that they are not equivalent agents. First, after cellular uptake and sequential phosphorylations, azacitidine is incorporated into both RNA and DNA while decitabine is phosphorylated by different kinases and is incorporated only into DNA [28]. Second, azacitidine may involve additional mechanisms of activity because it is incorporated into newly synthesised RNA, which inhibits protein synthesis [7]. Third, the in vitro sensitivities of human cancer cell lines to azacitidine and decitabine correlate poorly [22]. Fourth, several comparative studies show that azacitidine and decitabine have different effects on the gene expression profiles of various cancer cell lines [3, 6, 7, 23]. These different mechanisms of action may cause azacitidine and decitabine to have different clinical activities.
In the present study, AZA-7d and DEC-5d were compared retrospectively. Although both regimens were similarly effective in treating patients with MDS, there were some differences with regard to response patterns, toxicities, and the subgroups that showed more beneficial effects with one regimen. DEC-5d was associated with a higher frequency of mCR than AZA-7d, but it was also associated with a higher frequency of grade 3 or higher neutropaenia. These findings may be expected because compared to the ribonucleoside analogue azacitidine (80–90 % of which is incorporated directly into RNA), decitabine is generally believed to be a more potent DNA methylation inhibitor due to its deoxyribonucleoside structure [14, 16, 28]. In the present study, the two regimens were associated with similar overall survival rates. By contrast, two meta-analyses have shown that azacitidine is associated with better survival than decitabine [5, 12]. Moreover, in a phase 3 trial, only azacitidine significantly improved the survival in patients with higher risk MDS [2], whereas two randomised trials showed that decitabine failed to improve survival significantly [10, 15]. However, the latter studies used the 3-day regimen of decitabine. DEC-5d has not been compared to supportive care in a phase 3 trial, although this regimen is more widely used and seems to be more effective than the 3-day regimen. Azacitidine and decitabine have similarities in some pharmacokinetic parameters: they have large volumes of distribution, short half-lives and are rapidly cleared from the systemic circulation by hydrolysis and deamination [28]. These pharmacokinetic features may be improved by refining the dosing and administration. For example, subcutaneous administration of azacitidine results in a twofold longer half-life than intravenous administration [18]. Similarly, DEC-5d may have more advantageous pharmacokinetic profiles in terms of demethylation than the 3-day regimen, although the two decitabine regimens have not been compared in pharmacokinetic or clinical studies [11]. In the subgroup analysis of the present study, AZA-7d was associated with higher survival rates than DEC-5d in patients with an MDS duration over 1 year or a poor ECOG performance scale score, while DEC-5d was associated with higher overall response rates in lower risk MDS. These findings may provide some guidance when selecting between the two hypomethylating agents in clinical practice for MDS.
The present study is limited due to its retrospective nature. Baseline characteristics were not well matched between AZA-7d and DEC-5d (Table 1) and two treatment groups might not be comparable for the evaluation of treatment response and survival. More patients with RA were treated with azacitidine, whereas all but one patient with CMML were treated with decitabine probably because of the efficacy of decitabine in CMML from previous reports [20, 31]. Prior treatment for MDS, which is one of predictive factors for the response to hypomethylating therapy [9], was more frequently found in AZA-7d than in DEC-5d. AZA-7d had more patients with poor performance status or RBC transfusion dependency than DEC-5d. Median number of treatment courses, 5 in AZA-7d and 4 in DEC-5d, was relatively short compared to the reports from prospective clinical trials, and significant proportion of the patients discontinued the hypomethylating treatment due to the causes other than disease progression or excessive toxicity (Table 2). Many patients might receive inadequate hypomethylating therapy because treatment duration of a minimum of six courses is generally recommended before evaluating response, unless overt progression or unacceptable toxicity occurs [4].
In conclusion, both the AZA-7d and DEC-5d regimens were effective in the treatment of patients with MDS. However, the two regimens did differ in terms of clinical responses and toxicities. There may be specific subgroups in which one hypomethylating regimen is superior to others.
References
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, Pinto A, Beran M, de Witte TM, Stone RM, Mittelman M, Sanz GF, Gore SD, Schiffer CA, Kantarjian H (2006) Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 108:419–425
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz G, List A, Gore SD, Seymour JF, Bennett JM, Byrd J, Backstrom J, Zimmerman L, McKenzie D, Beach C, Silverman LR (2009) Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 10:223–232
Flotho C, Claus R, Batz C, Schneider M, Sandrock I, Ihde S, Plass C, Niemeyer CM, Lubbert M (2009) The DNA methyltransferase inhibitors azacitidine, decitabine and zebularine exert differential effects on cancer gene expression in acute myeloid leukemia cells. Leukemia 23:1019–1028
Gotze K, Platzbecker U, Giagounidis A, Hasse D, Lubbert M, Aul C, Ganser A, Germing U, Hofman WK (2010) Azacitidine for treatment of patients with myelodysplastic syndromes (MDS): practical recommendations of the German MDS Study Group. Ann Hematol 89:841
Gurion R, Vidal L, Gafter-Gvili A, Belnik Y, Yeshurun M, Raanani P, Shpilberg O (2010) 5-azacitidine prolongs overall survival in patients with myelodysplastic syndrome—a systematic review and meta-analysis. Haematologica 95:303–310
Hagemann S, Heil O, Lyko F, Brueckner B (2011) Azacytidine and decitabine induce gene-specific and non-random DNA demethylation in human cancer cell lines. PLoS One 6:e17388
Hollenbach PW, Nguyen AN, Brady H, Williams M, Ning Y, Richard N, Krushel L, Aukerman SL, Heise C, MacBeth KJ (2010) A comparison of azacitidine and decitabine activities in acute myeloid leukemia cell lines. PLoS One 5:e9001
Hurd PJ, Whitmarsh AJ, Baldwin GS, Kelly SM, Waltho JP, Price NC, Connolly BA, Hornby DP (1999) Mechanism-based inhibition of C5-cytosine DNA methyltransferases by 2-H pyrimidinone. J Mol Biol 286:389–401
Itzykson R, Fenaux P (2012) Predicting the outcome of patients with higher-risk myelodysplastic syndrome treated with hypomethylating agents. Leuk Lymphoma 53:760–762
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, Klimek V, Slack J, de Castro C, Ravandi F, Helmer R 3rd, Shen L, Nimer SD, Leavitt R, Raza A, Saba H (2006) Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer 106:1794–1803
Kantarjian H, Oki Y, Garcia-Manero G, Huang X, O’Brien S, Cortes J, Faderl S, Bueso-Ramos C, Ravandi F, Estrov Z, Ferrajoli A, Wierda W, Shan J, Davis J, Giles F, Saba HI, Issa JP (2007) Results of a randomized study of 3 schedules of low-dose decitabine in higher-risk myelodysplastic syndrome and chronic myelomonocytic leukemia. Blood 109:52–57
Kumar A, List AF, Hozo I, Komrokji R Djulbegovic B (2010) Decitabine versus 5-azacitidine for the treatment of myelodysplastic syndrome: adjusted indirect meta-analysis. Haematologica 95:340–342, author reply 343–344
Lee JH, Jang JH, Park J, Park S, Joo YD, Kim YK, Kim HG, Choi CW, Kim SH, Park SK, Park E, Min YH (2011) A prospective multicenter observational study of decitabine treatment in Korean patients with myelodysplastic syndrome. Haematologica 96:1441–1447
Li LH, Olin EJ, Buskirk HH, Reineke LM (1970) Cytotoxicity and mode of action of 5-azacytidine on L1210 leukemia. Cancer Res 30:2760–2769
Lubbert M, Suciu S, Baila L, Ruter BH, Platzbecker U, Giagounidis A, Selleslag D, Labar B, Germing U, Salih HR, Beeldens F, Muus P, Pfluger KH, Coens C, Hagemeijer A, Eckart Schaefer H, Ganser A, Aul C, de Witte T, Wijermans PW (2011) Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol 29:1987–1996
Lyko F, Brown R (2005) DNA methyltransferase inhibitors and the development of epigenetic cancer therapies. J Natl Cancer Inst 97:1498–1506
Lyons RM, Cosgriff TM, Modi SS, Gersh RH, Hainsworth JD, Cohn AL, McIntyre HJ, Fernando IJ, Backstrom JT, Beach CL (2009) Hematologic response to three alternative dosing schedules of azacitidine in patients with myelodysplastic syndromes. J Clin Oncol 27:1850–1856
Marcucci G, Silverman L, Eller M, Lintz L, Beach CL (2005) Bioavailability of azacitidine subcutaneous versus intravenous in patients with the myelodysplastic syndromes. J Clin Pharmacol 45:597–602
Mortusewicz O, Schermelleh L, Walter J, Cardoso MC, Leonhardt H (2005) Recruitment of DNA methyltransferase I to DNA repair sites. Proc Natl Acad Sci U S A 102:8905–8909
Oki Y, Jelinek J, Shen L, Kantarjian HM, Issa JP (2008) Induction of hypomethylation and molecular response after decitabine therapy in patients with chronic myelomonocytic leukemia. Blood 111:2382–238431
Palii SS, Van Emburgh BO, Sankpal UT, Brown KD, Robertson KD (2008) DNA methylation inhibitor 5-Aza-2'-deoxycytidine induces reversible genome-wide DNA damage that is distinctly influenced by DNA methyltransferases 1 and 3B. Mol Cell Biol 28:752–771
Qin T, Jelinek J, Si J, Shu J, Issa JP (2009) Mechanisms of resistance to 5-aza-2'-deoxycytidine in human cancer cell lines. Blood 113:659–667
Qiu X, Hother C, Ralfkiaer UM, Sogaard A, Lu Q, Workman CT, Liang G, Jones PA, Gronbaek K (2010) Equitoxic doses of 5-azacytidine and 5-aza-2'deoxycytidine induce diverse immediate and overlapping heritable changes in the transcriptome. PLoS One 5:pii:e12994
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, Stone RM, Nelson D, Powell BL, DeCastro CM, Ellerton J, Larson RA, Schiffer CA, Holland JF (2002) Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol 20:2429–2440
Silverman LR, McKenzie DR, Peterson BL, Holland JF, Backstrom JT, Beach CL, Larson RA (2006) Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol 24:3895–3903
Steensma DP, Baer MR, Slack JL, Buckstein R, Godley LA, Garcia-Manero G, Albitar M, Larsen JS, Arora S, Cullen MT, Kantarjian H (2009) Multicenter study of decitabine administered daily for 5days every 4weeks to adults with myelodysplastic syndromes: the alternative dosing for outpatient treatment (ADOPT) trial. J Clin Oncol 27:3842–3848
Steensma DP, Stone RM (2010) Practical recommendations for hypomethylating agent therapy of patients with myelodysplastic syndromes. Hematol Oncol Clin North Am 24:389–406
Stresemann C, Lyko F (2008) Modes of action of the DNA methyltransferase inhibitors azacytidine and decitabine. Int J Cancer 123:8–13
Wijermans PW, Krulder JW, Huijgens PC, Neve P (1997) Continuous infusion of low-dose 5-Aza-2'-deoxycytidine in elderly patients with high-risk myelodysplastic syndrome. Leukemia 11:1–5
Wijermans P, Lubbert M, Verhoef G, Bosly A, Ravoet C, Andre M, Ferrant A (2000) Low-dose 5-aza-2'-deoxycytidine, a DNA hypomethylating agent, for the treatment of high-risk myelodysplastic syndrome: a multicenter phase II study in elderly patients. J Clin Oncol 18:956–962
Wijermans PW, Ruter B, Baer MR, Slack JL, Saba HI, Lubbert M (2008) Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML). Leuk Res 32:587–591
Yoo CB, Jones PA (2006) Epigenetic therapy of cancer: past, present and future. Nat Rev Drug Discov 5:37–50
Acknowledgments
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A062254).
Conflict of Interest
Je-Hwan Lee has received honoria from Janssen, Korea and Celgene, Korea for lecturing. Other authors have nothing to disclose regarding conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lee, JH., Choi, Y., Kim, SD. et al. Comparison of 7-day azacitidine and 5-day decitabine for treating myelodysplastic syndrome. Ann Hematol 92, 889–897 (2013). https://doi.org/10.1007/s00277-013-1702-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1702-8