Abstract
Adenovirus (AdV) infection is an emerging complication in patients undergoing allogeneic stem cell transplantation (SCT) and is closely associated with delayed immune reconstitution. In particular, disseminated AdV disease accompanies a high mortality. We retrospectively examined the incidence of AdV infection in patients undergoing unmanipulated haploidentical SCT. Following 121 transplantations in 110 patients, three had asymptomatic AdV viremia, three had localized AdV disease (hemorrhagic cystitis, HC), and seven had disseminated AdV disease (HC + viremia). The median time from transplantation to the onset of AdV-associated HC was 15 days (range 4–39), and the median time to the onset of disseminated AdV disease was 23 days (range 7–38). The cumulative incidence of AdV-associated HC was 8.3 %, and that of disseminated AdV disease was 5.8 %. AdV group B (type 11, type 34, or type 35) was detected in plasma samples from all the patients with disseminated AdV disease. Among them, three patients who received either cidofovir or donor lymphocyte infusion (DLI) alone progressed to pneumonia and died. The remaining four patients were treated with the combination of cidofovir and low-dose unmanipulated DLI, and all survived. We showed that disseminated AdV disease is a significant complication after haplo-SCT and that the combination of cidofovir and DLI is a promising treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Viral infections remain one of the most important complications following allogeneic stem cell transplantation (SCT) [1]. Although surveillance and therapeutic strategies have been established for several viral infections (including CMV infection), such strategies are not yet established for adenovirus (AdV) infection. AdV infection, usually resulting from reactivation of the virus [2], can be divided into three categories: asymptomatic AdV infection, localized AdV disease [e.g., hemorrhagic cystitis (HC), colitis, and pneumonia], and disseminated AdV disease. The reported mortality of patients with disseminated AdV disease is remarkably high, varying from 20 % to 80 % in different studies [3–5].
Previous studies have shown that the development of AdV infection is closely associated with the delayed recovery of T cells [6]. Reported risk factors include in vivo or ex vivo T cell depletion [e.g., the use of antithymocyte globulin (ATG), alemtuzumab, and CD34+ selection] [7–9], HLA-mismatched donors [6], cord blood as the stem cell source [5], and occurrence of GVHD [5]. Thus, the recently issued international guideline states that weekly monitoring for active AdV infection by PCR either for the first 6 months after SCT or for the duration of severe immunosuppression/lymphocytopenia should be considered (CII) for these patients [1]. Nevertheless, no consensus exists on whether systematic surveillance for AdV viremia should be performed for adult patients with those risk factors because of the low incidence of AdV viremia in the absence of clinical symptoms [10].
The current therapeutic options for AdV infection are antiviral drugs and immunomodulation [i.e., reducing the dose of immunosuppressant and donor lymphocyte infusion (DLI)]. To date, cidofovir is the only antiviral drug that is generally accepted to be useful in the treatment of adenovirus infection. Nevertheless, previous studies demonstrated that clearance of the virus with cidofovir occurs only in patients who attain T-cell reconstitution during the treatment [11]. Furthermore, previous studies have shown that the effect of cidofovir is limited in patients with disseminated AdV disease, resulting in a significant mortality [12]. By contrast, although previous studies have shown the efficacy of unmanipulated DLI [3, 7, 13–15], it is often the last treatment of choice because of the risk of GVHD, particularly for patients undergoing HLA-mismatched SCT. Adoptive transfer of AdV-specific T cells is a promising approach [16, 17], but it remains investigational at present and is available at only a few institutions.
Here, we retrospectively examined the incidence of AdV infection in patients who underwent haplo-SCT at our institution. Moreover, we evaluated the efficacy of the treatment strategies in patients who developed disseminated AdV disease.
Patients and methods
Patients and transplantation protocols
In the 2-year period between December 2008 and November 2010, 110 patients received a total of 121 haplo-SCT procedures at Hyogo College of Medicine. Institutional protocols for haplo-SCT with myeloablative preparative conditioning or reduced-intensity conditioning have been previously described [18, 19]. Briefly, for HLA 2−3 antigen-mismatched myeloablative SCT, a combination of tacrolimus, methotrexate, mycophenolate mofetil, and methylprednisolone (2 mg/kg) was used as GVHD prophylaxis. For HLA 1 antigen-mismatched myeloablative SCT, a combination of tacrolimus and methylprednisolone (2 mg/kg) was used as GVHD prophylaxis. For HLA 1−3 antigen-mismatched reduced-intensity SCT, anti-T-lymphocyte globulin (ATG-Fresenius, 2 mg/kg for 4 days) or anti-thymocyte globulin (Thymoglobulin, 0.5−1 mg/kg for 4 days) was included in the preparative regimen, and a combination of tacrolimus and methylprednisolone (1 mg/kg) was used as GVHD prophylaxis. The age-based criteria for the reduced-intensity conditioning regimen were 40 years old or older for HLA 2−3 antigen-mismatched SCT and 50 years old or older for HLA 1 antigen-mismatched SCT. Patients with comorbidities or those who had undergone prior SCT also received the reduced-intensity conditioning regimen. In general, bone marrow was the stem cell source in myeloablative haplo-SCT, and peripheral blood stem cells (PBSC) were the stem cell source in reduced-intensity haplo-SCT.
Acyclovir was administered from day −7 to day 35 at 1,000 mg/day and continued at 200 mg/day until the discontinuation of immunosuppressant. Patients received intravenous immunoglobulin 100 mg/kg weekly for 2 months after transplantation. CMV was monitored weekly by a pp65 antigenemia test, and human herpesvirus-6 was monitored weekly by PCR for virus DNA. Documented CMV or human herpesvirus-6 reactivation was treated with either ganciclovir or foscarnet. This study was approved by the Institutional Review Board of the Hyogo College of Medicine and was conducted according to the declaration of Helsinki. All patients provided informed consent prior to participating in the study.
Laboratory methods
AdV DNA in plasma was prospectively monitored every 2 weeks for 6 weeks and monthly for 3 months after SCT. AdV DNA in urine was tested in patients who had symptoms of HC. Real-time PCR of AdV DNA was performed according to the methods of the previous report, with some modifications [20]. In patients who became positive for AdV DNA either in plasma or in urine, AdV DNA was examined weekly in both plasma and urine until the clearance of AdV DNA. Genotyping of AdV was performed by PCR in plasma taken from the patients with disseminated AdV disease, according to the previous report [21]. Donors for the patients who developed disseminated AdV disease were examined for AdV serostatus for AdV type 2 (group C), type 5 (group C), and type 11 (group B2) by neutralization tests.
Definitions
Asymptomatic AdV infection was defined as any detection of AdV adenovirus without signs and symptoms. Localized AdV disease was defined as the presence of symptoms and signs in addition to AdV detection from the corresponding organ. Disseminated AdV disease was defined as AdV disease involving two or more organs, or AdV disease in one organ together with a high AdV DNA level in plasma (>104 copies/mL). Diagnosis of acute and chronic GVHD was based on standard clinical criteria [22, 23], with histopathologic confirmation where possible.
Treatment of disseminated adenovirus disease
Patients with disseminated AdV disease received either cidofovir, unmanipulated DLI, or both. Cidofovir was administered 1 mg/kg for 3 days per week [24, 25]. Probenecid was not used [26]. DLI was generally started at a low dose (1–10 × 104 CD3+ cells/kg) and thereafter dose-escalated in the absence of GVHD. Low-dose DLI (<5 × 106 CD3+ cells/kg) was performed simply as a transfusion of donor peripheral blood. Higher-dose DLI was performed with leukapheresis. High-dose intravenous immunoglobulin (400 mg/kg for 5 days) was used in combination with the above treatments in some patients.
Statistical analysis
Cumulative incidence was used to estimate the probabilities of AdV disease by treating death as a competing risk. The Gray test was used for group comparisons of cumulative incidence. Potential risk factors for the occurrence of AdV disease were tested using the Cox proportional hazard regression model. The following covariates were tested: patient age (<50 years vs. ≥50 years), sex, disease status (remission vs. no remission), number of HLA mismatches in the GVH vector (1 vs. 2–3), the use of ATG in the preparative regimen, stem cell source (bone marrow vs. PBSC), and number of allo-SCT procedures (first vs. second or later).
Results
Occurrence of AdV infections
Among the 121 patients who received haplo-SCT during the study period, three had asymptomatic AdV viremia, three had localized AdV disease without viremia, and seven had disseminated AdV disease (Table 1). All three patients with localized AdV disease manifested as HC. Moreover, all seven patients with disseminated AdV disease manifested as HC and viremia (high AdV DNA level in plasma). Two of these seven patients had a history of AdV-associated HC prior to the SCT. In all three patients with asymptomatic AdV viremia, detection of AdV DNA was transient, and none developed AdV disease.
The median time from transplantation to the onset of AdV-associated HC (n = 10) was 15 days (range 4–39). The median time from transplantation to the onset of disseminated AdV disease (n = 7) was 23 days (range 7–38). None of the patients had developed acute GVHD at the onset of AdV-associated HC. The cumulative incidence of AdV-associated HC was 8.3 %, and the cumulative incidence of disseminated AdV disease was 5.8 %. Male patients had higher cumulative incidences of AdV-associated HC (12.1 %) and disseminated AdV disease (9.1 %) than did female patients (3.6 % and 1.8 %, respectively), but this difference was not statistically significant (P = 0.097 and P = 0.086, respectively). Multivariate analysis failed to identify any statistically significant risk factors for the occurrence of AdV-associated HC or disseminated AdV disease in this cohort.
Serotypes of the AdV detected in plasma of the patients who developed disseminated AdV disease are shown in Table 2. AdV type 11 (group B) was detected in five out of seven patients, and AdV type 34 (group B) and type 35 (group B) were detected in one patient each.
AdV serostatus of donors
The AdV serostatus of the donors for the seven patients who developed disseminated AdV disease are shown in Table 3. Six out of seven donors were positive for antibodies either to AdV type 2 or type 5 (group C), but negative for antibody to AdV type 11 (group B). The remaining donor was positive for antibody to AdV type 11, but negative for antibodies to AdV type 2 and type 5.
Clinical course of the disseminated AdV disease
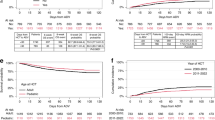
The clinical courses of disseminated AdV disease in seven patients are shown in Fig. 1. The first patient was initially treated with cidofovir alone, but the AdV DNA level continued to increase. One month after the onset of AdV HC, the patient developed AdV pneumonia, which was refractory to DLI, and died (Fig. 1a). The second and third patients received multiple treatments of DLI with dose escalation, but both died of AdV pneumonia, which occurred 1 month after the onset of AdV-associated HC (Fig. 1b, c). The third patient showed stabilization of AdV DNA levels after DLI, but the effect was transient.
On the basis of these experiences, the remaining four patients (no. 4–7) were treated with a combination of cidofovir and unmanipulated low-dose DLI from as early after the diagnosis of AdV disease as possible (Fig. 1d–g). Total number of cidofovir doses were seven in one patient (no. 6), six in two patients (no. 4 and 7), and three in one patient (no. 5). Cause of discontinuation in one patient (no. 5) was a remarkable elevation in serum creatinine level (≥2.0 mg/dl), but it is attributable to AdV-associated postrenal obstruction presenting bilateral hydronephrosis. Another patient (no. 4) also presented an AdV-associated postrenal obstruction during the clinical course, and the other two patients (no. 6 and 7) retained normal renal function. The combined use of cidofovir and DLI resulted in an apparent increase in lymphocyte count in two patients, which coincided with a decrease of AdV DNA load (patient no. 5 and 6). The remaining two patients (no. 4 and 7) showed only mild lymphocyte recovery, but AdV DNA levels steadily decreased in both cases. None of them developed AdV pneumonia, and none died from AdV-related causes. One patient (no. 6) had CMV antigenemia at the onset of AdV disease, which was treated by ganciclovir 5 mg/kg. None of the patients had CMV reactivation during cidofovir treatment. None of the patients had acute GVHD at the onset of AdV disease, and none developed GVHD after low-dose DLI. One patient is alive in complete remission, while causes of death in the other three patients are relapse, thrombotic microangiopathy, and sepsis after second transplantation.
Discussion
The present study has several major findings. We observed a high incidence of disseminated AdV disease in adult patients undergoing unmanipulated haplo-SCT (5.8 %). This may be attributable to delayed immune reconstitution as a result of HLA-mismatched SCT and the use of ATG and steroid as GVHD prophylaxis. Alternatively, the fact that a high proportion of the patients already had prolonged lymphocytopenia at the time of haplo-SCT due to heavy pretreatment (including multiple courses of chemotherapy and prior allo-SCT) may also have affected the result. In fact, two of the seven patients who developed disseminated AdV disease had a history of AdV-associated HC prior to haplo-SCT. Possibly as a consequence of these treatment backgrounds, the median time from SCT to the onset of disseminated AdV disease in the present study was remarkably short (day 23, range 7–38). This is much more rapid than in previous studies, one of which showed that AdV infection occurs later (>90 days after SCT) in adult patients [27].
We also found that disseminated AdV disease exclusively occurred in patients suffering from AdV-associated HC, and group B virus was identified from plasma in all seven patients (type 11 in five patients, type 34 in one patient, and type 35 in one patient). In contrast, previous studies from the West have shown that the most common AdV subgroup detected in patients with disseminated AdV disease was C, followed by A, B, and D [3–5, 7].
Interestingly, the previously reported incidence of post-transplant HC caused by AdV type 11 (group B) is higher in the Japanese studies than in the Western studies [28, 29]. Moreover, a study in the 1970s in non-transplant pediatric settings showed that AdV type 11 was more frequently detected in Japanese cases with HC than in American cases [30]. Overall, ethnicity appears to have an influence on the result of the present study: Japanese patients may have a higher incidence of latent infection of group B AdV, which can translate into a higher incidence of AdV-associated HC and disseminated AdV disease with group B virus. In addition, our result shows a trend of male predominance in AdV-associated HC and disseminated AdV disease, which is consistent with the previously reported male predominance in post-transplant HC in Japanese patients [29]. Tropism of group B AdV to a male-specific organ around the urinary tract is hypothesized to be the reason for male predominance.
We confirmed that a sustained high ADV DNA level in plasma is associated with a fatal outcome, as shown in previous studies [31, 32]. All three of our patients with sustained high ADV DNA levels died from AdV pneumonia. In contrast, the usefulness of the routine monitoring of AdV DNA level by PCR could not be clearly seen in the present study. In fact, all patients who had high AdV DNA levels in plasma also had HC. Moreover, no patients with transient low AdV DNA levels (<1 × 104 copies/mL) developed AdV disease. Our observations are consistent with the recent reports showing that transient low AdV DNA level is not associated with the development of AdV disease [32, 33]. Thus, serial AdV DNA monitoring only in patients who have clinical manifestations of AdV infection (particularly HC in Japanese patients) may be a useful and practical approach.
Finally, we found that the combined use of cidofovir and unmanipulated low-dose DLI at an early time point is a promising treatment option for disseminated AdV disease. All of the four patients treated with this approach had favorable clinical courses. In contrast, low-dose DLI alone did not result in the decrease of AdV DNA load. Moreover, recent studies have shown the effect of cidofovir to be limited in cases of lymphocytopenia. When these results are taken together, synergistic effect of combined treatment with cidofovir and low-dose DLI is suggested. The usefulness of unmanipulated low-dose DLI for viral infection after haplo-SCT was previously shown [34, 35]. Although the frequencies of AdV-specific T cells were not examined in the present study, the kinetics of the viral load indicate that AdV-specific T cells were transferred with the low-dose DLI and consequently functioned to clear virus. Out of seven DLI donors, six were positive for AdV type 2 (group C), type 5 (group C), or type 11 (group B), which suggests that specific T cells for at least some AdV subgroups exist in most healthy donors. Moreover, previous studies aiming to generate AdV-specific T cells have shown that T cells generated with group C adenovirus exert cross reactivity in recognizing AdV from all three subgroups (A, B, and C) [36]. Furthermore, the aforementioned previous study of adoptive transfer of AdV-specific T cells demonstrated that the efficacy was independent of the infused AdV-specific T-cell dose [16]. On the basis of these observations, we speculate that a small number of AdV-specific T cells contained in unmanipulated donor lymphocytes were activated and proliferated in vivo, inducing an effective immune response against AdV.
The present study had several limitations. It was a retrospective study including a relatively small number of patients, and the patient characteristics were highly heterogeneous. Moreover, AdV DNA was not aggressively examined in specimens such as stools and gut biopsies. Thus, the incidence of AdV enteritis may have been underestimated. Nevertheless, our findings provide valuable information regarding the incidence and treatment strategy for disseminated AdV disease after haplo-SCT.
In conclusion, the present study showed that disseminated AdV disease is a significant complication after haplo-SCT. It may occur as a consequence of AdV-associated HC, which is frequently observed in Japanese patients. Although serial AdV DNA monitoring has clinical significance in the patients with AdV disease, the usefulness of routine monitoring of AdV DNA in asymptomatic patients remains uncertain. Finally, we found that the combined use of cidofovir and unmanipulated low-dose DLI is a promising treatment option for disseminated AdV disease. Prospective studies are warranted to evaluate the efficacy and safety of this treatment strategy for use until the adoptive transfer of AdV-specific T cells becomes widely available.
References
Tomblyn M, Chiller T, Einsele H et al (2009) Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Bone Marrow Transplant 44:453–558
Veltrop-Duits LA, van Vreeswijk T, Heemskerk B et al (2011) High titers of pre-existing adenovirus serotype-specific neutralizing antibodies in the host predict viral reactivation after allogeneic stem cell transplantation in children. Clin Infect Dis 52:1405–1413
Howard DS, Phillips IG, Reece DE et al (1999) Adenovirus infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 29:1494–1501
Lion T, Baumgartinger R, Watzinger F et al (2003) Molecular monitoring of adenovirus in peripheral blood after allogeneic bone marrow transplantation permits early diagnosis of disseminated disease. Blood 102:1114–1120
Robin M, Marque-Juillet S, Scieux C et al (2007) Disseminated adenovirus infections after allogeneic hematopoietic stem cell transplantation: incidence, risk factors and outcome. Haematologica 92:1254–1257
Heemskerk B, Lankester AC, van Vreeswijk T et al (2005) Immune reconstitution and clearance of human adenovirus viremia in pediatric stem-cell recipients. J Infect Dis 191:520–530
Chakrabarti S, Mautner V, Osman H et al (2002) Adenovirus infections following allogeneic stem cell transplantation: incidence and outcome in relation to graft manipulation, immunosuppression, and immune recovery. Blood 100:1619–1627
Myers GD, Krance RA, Weiss H et al (2005) Adenovirus infection rates in pediatric recipients of alternate donor allogeneic bone marrow transplants receiving either antithymocyte globulin (ATG) or alemtuzumab (Campath). Bone Marrow Transplant 36:1001–1008
Kampmann B, Cubitt D, Walls T et al (2005) Improved outcome for children with disseminated adenoviral infection following allogeneic stem cell transplantation. Br J Haematol 130:595–603
Munoz-Cobo B, Solano C, Nieto J, et al. (2011) Surveillance for adenovirus DNAemia early after transplantation in adult recipients of unrelated-donor allogeneic stem cell transplants in the absence of clinically suspected infection. Bone Marrow Transplant 46:1484–1486
de Pagter AP, Haveman LM, Schuurman R, Schutten M, Bierings M, Boelens JJ (2009) Adenovirus DNA positivity in nasopharyngeal aspirate preceding hematopoietic stem cell transplantation: a very strong risk factor for adenovirus DNAemia in pediatric patients. Clin Infect Dis 49:1536–1539
Lindemans CA, Leen AM, Boelens JJ (2010) How I treat adenovirus in hematopoietic stem cell transplant recipients. Blood 116:5476–5485
Hromas R, Cornetta K, Srour E, Blanke C, Broun ER (1994) Donor leukocyte infusion as therapy of life-threatening adenoviral infections after T-cell-depleted bone marrow transplantation. Blood 84:1689–1690
Chakrabarti S, Collingham KE, Fegan CD, Pillay D, Milligan DW (2000) Adenovirus infections following haematopoietic cell transplantation: is there a role for adoptive immunotherapy? Bone Marrow Transplant 26:305–307
Bordigoni P, Carret AS, Venard V, Witz F, Le Faou A (2001) Treatment of adenovirus infections in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis 32:1290–1297
Feuchtinger T, Matthes-Martin S, Richard C et al (2006) Safe adoptive transfer of virus-specific T-cell immunity for the treatment of systemic adenovirus infection after allogeneic stem cell transplantation. Br J Haematol 134:64–76
Leen AM, Christin A, Myers GD et al (2009) Cytotoxic T lymphocyte therapy with donor T cells prevents and treats adenovirus and Epstein–Barr virus infections after haploidentical and matched unrelated stem cell transplantation. Blood 114:4283–4292
Ogawa H, Ikegame K, Yoshihara S et al (2006) Unmanipulated HLA 2-3 antigen-mismatched (haploidentical) stem cell transplantation using nonmyeloablative conditioning. Biol Blood Marrow Transplant 12:1073–1084
Ogawa H, Ikegame K, Kaida K et al (2008) Unmanipulated HLA 2-3 antigen-mismatched (haploidentical) bone marrow transplantation using only pharmacological GVHD prophylaxis. Exp Hematol 36:1–8
Teramura T, Naya M, Yoshihara T, Kanoh G, Morimoto A, Imashuku S (2004) Adenoviral infection in hematopoietic stem cell transplantation: early diagnosis with quantitative detection of the viral genome in serum and urine. Bone Marrow Transplant 33:87–92
Takeuchi S, Itoh N, Uchio E, Aoki K, Ohno S (1999) Serotyping of adenoviruses on conjunctival scrapings by PCR and sequence analysis. J Clin Microbiol 37:1839–1845
Przepiorka D, Weisdorf D, Martin P et al (1995) 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 15:825–828
Shulman HM, Sullivan KM, Weiden PL et al (1980) Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 69:204–217
Hoffman JA, Shah AJ, Ross LA, Kapoor N (2001) Adenoviral infections and a prospective trial of cidofovir in pediatric hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 7:388–394
Nagafuji K, Aoki K, Henzan H et al (2004) Cidofovir for treating adenoviral hemorrhagic cystitis in hematopoietic stem cell transplant recipients. Bone Marrow Transplant 34:909–914
Savona MR, Newton D, Frame D, Levine JE, Mineishi S, Kaul DR (2007) Low-dose cidofovir treatment of BK virus-associated hemorrhagic cystitis in recipients of hematopoietic stem cell transplant. Bone Marrow Transplant 39:783–787
Flomenberg P, Babbitt J, Drobyski WR et al (1994) Increasing incidence of adenovirus disease in bone marrow transplant recipients. J Infect Dis 169:775–781
Akiyama H, Kurosu T, Sakashita C et al (2001) Adenovirus is a key pathogen in hemorrhagic cystitis associated with bone marrow transplantation. Clin Infect Dis 32:1325–1330
Asano Y, Kanda Y, Ogawa N et al (2003) Male predominance among Japanese adult patients with late-onset hemorrhagic cystitis after hematopoietic stem cell transplantation. Bone Marrow Transplant 32:1175–1179
Mufson MA, Belshe RB (1976) A review of adenoviruses in the etiology of acute hemorrhagic cystitis. J Urol 115:191–194
Schilham MW, Claas EC, van Zaane W et al (2002) High levels of adenovirus DNA in serum correlate with fatal outcome of adenovirus infection in children after allogeneic stem-cell transplantation. Clin Infect Dis 35:526–532
Gustafson I, Lindblom A, Yun Z et al (2008) Quantification of adenovirus DNA in unrelated donor hematopoietic stem cell transplant recipients. J Clin Virol 43:79–85
Ohrmalm L, Lindblom A, Omar H et al (2011) Evaluation of a surveillance strategy for early detection of adenovirus by PCR of peripheral blood in hematopoietic SCT recipients: incidence and outcome. Bone Marrow Transplant 46:267–272
Yoshihara S, Kato R, Inoue T et al (2004) Successful treatment of life-threatening human herpesvirus-6 encephalitis with donor lymphocyte infusion in a patient who had undergone human leukocyte antigen-haploidentical nonmyeloablative stem cell transplantation. Transplantation 77:835–838
Kawakami M, Nakata J, Ohguro N et al (2005) A case of immune recovery vitritis induced by donor leukocyte infusion for the treatment of cytomegalovirus retinitis. Eur J Haematol 75:352–354
Heemskerk B, Veltrop-Duits LA, van Vreeswijk T et al (2003) Extensive cross-reactivity of CD4+ adenovirus-specific T cells: implications for immunotherapy and gene therapy. J Virol 77:6562–6566
Acknowledgments
We thank the medical, nursing, and laboratory staff of the participating departments for their contributions to this study. We are also grateful to Ms. Aya Yano and Ms. Kimiko Yamamoto for their technical assistance and to Mr. Shigeo Kimura, Ms. Kazuko Saida, and Ms. Kumiko Sugawara for their assistance with data collection.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sources of support
None
Rights and permissions
About this article
Cite this article
Taniguchi, K., Yoshihara, S., Tamaki, H. et al. Incidence and treatment strategy for disseminated adenovirus disease after haploidentical stem cell transplantation. Ann Hematol 91, 1305–1312 (2012). https://doi.org/10.1007/s00277-012-1440-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-012-1440-3