Abstract
The purpose of our study is to compare the 7-year response to imatinib monotherapy as an initial treatment and re-treatment in Chinese patients with chronic myelogenous leukemia-chronic phase (CML-CP) patients in a single center in Beijing. A retrospective study of 171 CML-CP patients receiving imatinib monotherapy was done with 73 in the initial treatment group (disease course ≤6 months) and 98 in the re-treatment group (disease course >6 months). Cumulative rates of complete cytogenetic response (CCyR) at 6, 12, and 36 months after imatinib treatment in the initial and re-treatment groups were 75%, 89%, and 96%, and 48%, 77% and 84% (p = 0.0002), respectively. The median time to CCyR in the initial and re-treatment groups was 6 months (95% CI, 3.3–8.3) and 9 months (95% CI, 6.4–11.6), respectively (p = 0.0002). Cumulative rates of major molecular responses at 9, 12, and 18 months after imatinib treatment in the initial and re-treatment groups were 31%, 48%, and 60%, and 15%, 25% and 37% (p = 0.017), respectively. The median time to the major molecular response in the initial and re-treatment groups was 15 months (95% CI, 12.3–17.7) and 36 months (95% CI, 25.9–46.0), respectively (p = 0.017). Progression-free survival at 84 months in the initial and re-treatment groups was 97% and 85%, respectively (p = 0.09). Event-free survival at 84 months in the initial and re-treatment groups was 92% and 70%, respectively (p = 0.049). Only two of the 171 patients discontinued imatinib therapy for grade 3/4 adverse events. Our study revealed that CML-CP patients would benefit from early treatment with imatinib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Imatinib mesylate, a selective bcr-abl tyrosine kinase inhibitor, has demonstrated remarkable efficacy and tolerability in patients with chronic myelogenous leukemia-chronic phase (CML-CP), either newly diagnosed or after failure of interferon-α treatment. Imatinib has become the standard of treatment for this disease [1, 2]. A phase two trial of imatinib in late CML-CP after interferon-α (re-treatment) showed that 6-year cumulative rates of major cytogenetic response (MCyR) and complete cytogenetic response (CCyR) were 67% and 57%, respectively. Estimated rates of freedom from progression to accelerated phase (AP) and blastic phase, and overall survival (OS) at 6 years were 61% and 76%, respectively [3]. The IRIS (International Randomized trial of Interferon versus STI571) study has reported the response to imatinib as a first-line treatment for CML-CP patients and shown that more than 80% of patients receiving initial treatment with imatinib reached CCyR during the 5-year follow-up period [3]. Estimated 5-year OS rate with imatinib was 89%, event-free survival (EFS) rate was 83%, and those free from progression to AP and blast crisis were 93%. Based on clinical results from randomized trials, imatinib has been approved for first-line treatment of all phases of chronic myelogenous leukemia (CML) [4–9]. The efficacy of imatinib as a first-line treatment seems superior to its use as a second-line re-treatment in CML-CP patients based on various clinical trials [3–9]. To date, there have been rarely homeochronous studies comparing the response to imatinib in CML-CP patients as a first-line treatment versus re-treatment as imatinib has been mostly used for first-line treatment in all phases of CML in many countries.
In China, many CML-CP patients cannot receive imatinib as an initial treatment due to economic limitations. In this study, we explore whether timing of imatinib treatment affects efficacy in CML-CP patients, by comparing the 7-year response to imatinib monotherapy as an initial treatment versus the re-treatment in CML-CP patients in a single center in Beijing, China.
Materials and methods
Patients
Data was collected from a total of 171 CML-CP patients who received imatinib monotherapy over the period of April 2001 to December 2007, including 73 in the initial treatment group (disease course of no more than 6 months) and 98 in the re-treatment group (disease course of more than 6 months). Chronic phase was defined by the presence of <15% blasts, <20% basophils, and <30% blasts plus promyelocytes in the peripheral blood and marrow. No patients in the initial treatment group had received interferon α (IFN-α) prior to the study. However, all patients in the re-treatment group had previously been treated with IFN-α, presenting as hematologic or cytogenetic resistance or intolerance [10].
Treatment method
All patients had been treated by imatinib monotherapy (Novartis, Switzerland) at an initial dose of 400 mg/day, and the dose increased to 600–800 mg/day on the basis of hematology results and molecular genetics analyses; for patients with insufficient response (defined in the NCCN 2008) [11], direct sequencing was applied to detect the abl kinase domain mutation.
Bone marrow morphology, bone marrow chromosome [12], and bcr-abl mRNA levels [13] (via quantitative RT-PCR) were checked every 3 months in the first and second year during treatment and every 6 months after reaching CCyR. Size of the liver and spleen, as well as extramedullary infiltration, were examined at each follow-up visit.
Assessment criteria
The assessment criteria are as follows: (1) Hematologic response, including complete hematologic response (CHR) [10]: CML-CP progression was defined as a disease that had progressed to AP or blast phase under continuous treatment. (2) Cytogenetic response in marrow cells was defined as CCyR (no Ph-positive marrow metaphases) and MCyR (1% to 35% Ph-positive metaphases) on the basis of G-banding in at least 20 cells in metaphase per sample. (3) Molecular responses were indicated by major molecular response (MMoR), defined as a 3-log reduction in bcr-abl mRNA transcripts compared with a standardized baseline. (4) Imatinib resistance, according to NCCN 2008, is defined as primary resistance (failure to achieve CHR after treatment with imatinib at a daily dose of more than 300 mg for 3 months, failure to achieve MCyR after treatment with imatinib at a daily dose of 400 mg for 12 months, or failure to achieve CCyR after treatment with imatinib at a daily dose of 400 mg for 18 months) and secondary resistance (hematologic relapse, recurrence of Ph chromosome, Ph chromosome increased by 30% in re-check at a 3-month interval, emergence of clonal evolution besides Ph chromosome, bcr-abl/abl ratio increased by more than 1 log in sequence examination or with Ph recurrence at the same time) [13–15] and (5) EFS.
Events were defined by the first occurrence of any of the following: death from any cause during treatment, progression to the AP or blast crisis of CML, or loss of a CHR or CCyR.
Efficacy observation
To assess treatment efficacy, we compared the cytogenetic efficacy, molecular efficacy, progression-free survival (PFS), and EFS between the two groups after 84 months of imatinib treatment.
Statistical analysis
Rank-sum test was applied to compare gender, age distribution, and follow-up time between the two groups. The Kaplan–Meier survival analysis and log-rank tests were used to compare the cumulative rates of CCyR achieved by the two groups. The Kaplan–Meier method was also used to calculate PFS and EFS, and the log-rank test used to compare the survival rates of the two groups.
Ethics and study management
The study protocol was reviewed by the ethics committee of the People's Hospital of Peking University. All patients gave written informed consent according to institutional regulations.
Results
Basic conditions of the patients in the two groups are described in Table 1. The gender and age composition of the two groups were similar (p > 0.8); the proportions of high, medium, and low-risk Sokal scores of the two groups were similar (p = 0.945). The median (range) follow-up time was 40 months (20–100) in the initial treatment group and 64 months (23–100) in the re-treatment group. The median follow-up time of all patients was 46 months (20–100).
All 171 patients achieved CHR. Only two patients were withdrawn from the study after treatment for 4 and 5 months, respectively, due to grade four skin rash, and the non-tolerance rate was 1.2%.
Cytogenetic response
On December 2009, cumulative rates of CCyR in initial treatment and re-treatment groups were 96% and 92%, respectively (Fig. 1a); cumulative rates of CCyR at 6, 12, and 36 months after imatinib treatment in initial treatment and re-treatment groups were 75%, 89% and 96%, and 48%, 77% and 84%, respectively (p = 0.0002) (Fig. 1a). Median time to CCyR in initial treatment and re-treatment groups was 6 months (95% CI, 3.3–8.3) and 9 months (95% CI, 6.4–11.6), respectively (p = 0.0002), indicating that the time to CCyR in the initial treatment group was significantly shorter than that in the re-treatment group.
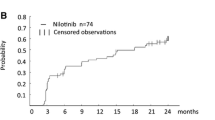
Cumulative rates of CCyR and major molecular response (MMoR) in the initial treatment and re-treatment groups of CML-CP patients receiving imatinib. a Cumulative rates of CCyR in the two groups. Median time to CCyR in the initial treatment and re-treatment groups was 6 months and 9 months, respectively. b Cumulative rates of MMoR in the two groups
Molecular response
The number of patients who received molecular monitoring in the initial treatment and re-treatment groups was 71 and 53, respectively. The cumulative rates of MMoR are described in Fig. 1b. There was a significant difference in the MMoR ratio achieved by the two groups within 5 years. Cumulative rates of MMoR at 9, 12, and 18 months after imatinib treatment in the initial treatment and re-treatment groups were 31%, 48% and 60%, and 15%, 25% and 37%, respectively (p = 0.017) (Fig. 1b). The MMoR rates in the initial treatment and re-treatment groups were expected to be 86% and 85%, respectively. Median time to MMoR in the initial treatment and re-treatment groups was 15 months (95% CI, 12.3–17.7) and 36 months (95% CI, 25.9–46.0), respectively (p = 0.017). The time to MMoR in the initial treatment group was shorter than that in the re-treatment group.
Survival
PFS at 84 months in initial treatment and re-treatment groups was 97% and 85%, respectively (p = 0.09) (Fig. 2). Survival with continued CCyR in the initial treatment and re-treatment groups was 98% and 83%, respectively (p = 0.12) (Fig. 3). The 84-month PFS in 148 patients with CCyR and 23 patients without CCyR was 92% and 32%, respectively (p < 0.0001) (Fig. 4). The 84-month EFS in the initial treatment and re-treatment groups was 92% and 71%, respectively (p = 0.049) (Fig. 5).
The expected 7-year survival, free from progression to AP and blast phase, in patients with CCyR plus MMoR, with CCyR without MMoR, and those without CCyR at 12 months was 100%, 100%, and 88% in the initial treatment group, and 100%, 92%, and 68% in the re-treatment group, respectively. There was a statistically significant difference (p = 0.0045) in the PFS between patients with CCyR and without CCyR in the two groups at 12 months.
Discussion
Imatinib has been recommended by the NCCN Practice Guidelines in Oncology and the European Leukemia Net (ELN) criteria as the standard first-line treatment for chronic phase CML. This means there are few homeochronous studies comparing the first-line and re-treatment responses of CML-CP patients with imatinib in Western countries.
In our retrospective and homeochronous study of 171 CML-CP patients treated with imatinib, only two (1.2%) of 171 patients withdrew from the study due to serious skin rash, indicating that imatinib was well tolerated in Chinese CML-CP patients.
The IRIS study [16] showed that after treatment with imatinib, the peak of disease progression (including loss of CHR, loss of CCyR, acceleration, blast crisis, and death) occurred during the second year (7.5%). However, the rate of disease progression subsequently declined year by year, with an annual rate of disease progression of only 1.6% in the third year, 0.9% in the fourth year, and nil by the sixth year. In our study, the median follow-up time of the initial treatment group was more than 3 years, past the peak of disease progression. Thus, the difference in the observation period between the two groups did not affect the PFS and OS.
Similar to the results of the IRIS study [16], the expected 7-year PFS of patients with CCyR plus MMoR in both groups of our study was 100% at 12 months. The 12-month MMoR can thus be used to estimate the possibility of a 7-year progression-free course of the disease.
Our study found a significant benefit in the use of imatinib as an initial treatment, compared with its use as a second-line re-treatment in single center. The median time to CCyR and MMoR was significantly shorter in the initial treatment group than that in the re-treatment group (Fig. 1). Goldman and colleagues [17] reported that the molecular effects of imatinib in the treatment of CML-CP patients increased over time in their study. The fact there was no difference in the MMoR of the two groups in our study after 5 years was likely related to the shorter follow-up period in the initial treatment group than that in the re-treatment group.
There was no significant difference in PFS between the two groups. Survival with continued CCyR was significantly higher in the initial treatment group than in the re-treatment group (98% versus 83%; p = 0.045). The 7-year EFS was significantly higher in the initial treatment group than in the re-treatment group (92% versus 70%; p = 0.049), which indicated that the possibility for the occurrence of acceleration, blast crisis, loss of CHR, or loss of CCyR was significantly higher in the re-treatment group than in the initial treatment group. Furthermore, both CCyR and MMoR were higher in the initial treatment group than in the re-treatment group at 12 months, suggesting a higher treatment response in the initial treatment group and also indicating that the disease status was more stable in patients with lower residual leukemic cell counts. In the era of interferon or tyrosine kinase inhibitors, other studies have confirmed our finding that CCyR is relevant to a high PFS [18–20].
In conclusion, a high 7-year CCyR was achieved in both the initial treatment and re-treatment groups of CML-CP patients. Survival free from progression to AP and blast phase was significantly higher in patients with CCyR than in patients without CCyR. Median time to CCyR and MMoR was significantly shorter in the initial treatment group than that in the re-treatment group. For CML-CP patients, the earlier the imatinib was administered, the sooner CCyR and MMoR were achieved. Although there was no significant difference in the 7-year PFS between the two groups, the 7-year EFS was significantly higher in the initial treatment group than in the re-treatment group. It is expected that the overall efficacy of imatinib as an initial treatment will be superior to that when it is used as a re-treatment.
The respective results of the IRIS study and the phase two trial of imatinib in late CML-CP after interferon-α [3, 4] suggest that response with imatinib as a first-line treatment for CML-CP patients is superior to that when used as a second-line re-treatment, supporting the conclusions of the present study.
We, therefore, hope that these findings will support guidelines recommending that CML-CP patients in China be treated with imatinib as a first line of treatment or as soon as possible thereafter.
References
Goldman JM, Melo JV (2003) Chronic myeloid leukemia: advances in biology and new approaches to treatment. N Engl J Med 349:1451–1464
Druker BJ, Lydon NB (2000) Lessons learned from the development of an Abl tyrosine kinase inhibitor for chronic myelogenous leukemia. J Clin Invest 105:3–7
Hochhaus A, Druker BJ, Sawyers C, Guilhot F, Schiffer CA, Cortes J et al (2008) Favorable long-term follow-up results over 6 years for response, survival, and safety with imatinib mesylate therapy in chronic-phase chronic myeloid leukemia after failure of interferon-treatment. Blood 111(3):1039–1043
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N et al (2006) Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 355:2408–2417
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM et al (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344:1031–1037
Sawyers CL, Hochhaus A, Feldman E, Goldman JM, Miller CB, Ottmann OG et al (2002) Imatinib induces hematologic and cytogenetic responses in patients with chronic myelogenous leukemia in myeloid blast crisis: results of a phase II study. Blood 99:3530–3539
Talpaz M, Silver RT, Druker BJ, Goldman JM, Gambacorti-Passerini C, Guilhot F et al (2002) Imatinib induces durable hematologic and cytogenetic responses in patients with accelerated phase chronic myeloid leukemia: results of a phase 2 study. Blood 99:1928–1937
Kantarjian H, Sawyers C, Hochhaus A, Guilhot F, Schiffer C, Gambacorti-Passerini C et al (2002) Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med 346:645–652
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F et al (2003) Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 348:994–1004
Jiang H, Chen S, Jiang B, Jiang Q, Lu D et al (2003) Imatinib in the treatment of 54 cases of Ph-positive chronic myeloid leukemia. Chin J Hematol 24:281–285
NCCN Practice Guidelines in Oncology-v.3.2008. http://www.nccn.org/professionals/physician_gls/PDF/cml.pdf
Hong H, Qiu J, Lai Y, Shi Y, He Q, Dang H et al (2003) Cytogenetic analysis of interferon-α in the treatment of Ph+ chronic myeloid leukemia. Chin J Exp Hematol 3:269–273
Qin Y, Li J, Zhu H, Ruan G, Li L, Zhang Y et al (2006) The level of bcr-abl mRNA monitored by real-time quantitative RT-PCR in patients with chronic myeloid leukemia after hematopoietic stem cell transplantation. Chin J Hematol 8:511–514
O’Brien SG (2004) Optimal therapy in CML. Am Soc Hematol Educ Program 146–149
Apperley JF (2003) Managing CML with patient-specific strategies. Am Soc Hematol Educ Program 142–152
Shah NP (2005) Loss of response to imatinib: mechanisms and management. Am Soc Hematol Educ Program 183–187
Hochhaus A, Druker BJ, Larson RA, O’Brien SG, Gathmann I, Guilhot F et al (2007) IRIS 6-year follow-up: sustained survival and declining annual rate of transformation in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) treated with imatinib. Blood (ASH Annual Meeting Abstracts) 110(11) (abstr 25)
Goldman JM, Hughes T, Radichet J, Branford S, Hochhaus A, So C et al (2005) Continuing reduction in level of residual disease after 4 years in patients with CML in chronic phase responding to first-line imatinib (IM) in the IRIS Study. Blood (ASH Annual Meeting Abstracts) 106(11) (abstr 163)
Bonifazi F, de Vivo A, Rosti G, Guilhot F, Guilhot J, Trabacchi E et al (2001) Chronic myeloid leukemia and interferon-alpha: a study of complete cytogenetic responders. Blood 98:3074–3081
Kantarjian HM, O’Brien S, Cortes JE, Shan JQ, Giles FJ, Rios MB et al (2003) Complete cytogenetic and molecular responses to interferon-alpha-based therapy for chronic myelogenous leukemia are associated with excellent long-term prognosis. Cancer 97:1033–1041
Acknowledgments
The authors would like to thank the contributions of all the people who have participated in this research. This includes our laboratory staff, our colleagues, and our nurses. During April 2001 to April 2002, 46 patients in our study had enrolled in the international phase II expanded clinical trial of imatinib mesylate sponsored by Novartis. Imatinib for patients for 9 months every year was supplied by the Glivec International Patient Assistance Program (Novartis)—patients paid for the other 3 months each year themselves.
Funding
Supported by the program for innovative research team in the university (grant No. IRT 0702)
Authorship and Disclosures
JH, CSS, JB, and JQ received research grants from Novartis in the course of the international phase II expanded clinical trial of imatinib mesylate in China from April 2001 to April 2002. All other authors declare no competing financial interests. HXJ takes responsibility for the paper. JH, CSS, JB, and JQ recruited the patients. QYZ and LYY performed the laboratory work for this study. HXJ and JH coordinated the research. JH participated in the statistical analysis. HXJ and JH wrote the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, H., Chen, SS., Jiang, B. et al. Seven-year response to imatinib as initial treatment versus re-treatment in Chinese patients with chronic myelogenous leukemia in the chronic phase. Ann Hematol 90, 41–46 (2011). https://doi.org/10.1007/s00277-010-1031-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-010-1031-0