Abstract
Developed for benign conditions including osteoporotic fractures and haemangiomas, vertebroplasty has since been employed in neoplastic lesions, including myeloma. Advances in myeloma treatments, yielding improved survival times, have led to an increasing need for effective therapies that improve quality of life. The first randomised trials of vertebroplasty to treat painful osteoporotic crush fractures have cast doubt of its benefit over a placebo procedure, with a proposed rationale that fracture healing over time may account for the non-superiority of the results. However, these findings cannot be extrapolated to myeloma where the pathology is one of progressive bony destruction coupled with failure of new bone formation. In this paper, we present the outcome data for myeloma patients treated at our tertiary referral centre over a 5-year period, focusing on both subjective and objective measures of efficacy and safety. Records were reviewed to extract pain score, function and analgesia pre/post-procedure. Where possible, patients were then contacted directly and asked to assess their benefit by grading change in pain score, analgesia use and mobility. Performance status was assessed using the Eastern Cooperative Oncology Group scale. Of the 26 patients treated for painful thoraco-lumbar lesions, 77% reported improved pain score (P < 0.003). Analgesia reduction, better mobility and improved performance status were also seen. Our data support the consideration of vertebroplasty as a first-line treatment for painful myelomatous vertebral disease. Prospective randomised studies are now required to further define its role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Back pain is one of the most common presenting symptoms of multiple myeloma, and approximately 60% of patients have vertebral involvement at diagnosis, primarily between T6 and L4 [1]. Along with the control of tumour burden, the reduction of disease-related symptoms is of utmost importance. Yet with the advancement of novel anti-tumoural agents, skeletal morbidity may persist, decreasing the quality of life of patients who otherwise benefit from improved survival times and longer time to disease progression.
The management of painful myeloma bone disease traditionally combines medical therapies, including analgesics, bisphosphonates, steroids and chemotherapy with radiotherapy and surgical intervention. Surgery is usually employed for lesions that threaten neurological function, and whilst radiotherapy is often efficacious, effect onset may be delayed and the dose of radiation limited by proximity to the spinal cord. Side effects from opiate analgesia can be problematic, particularly since myeloma patients are often older. The use of non-steroidal anti-inflammatory drugs is limited by their nephrotoxicity.
Since its initial use to treat benign vertebral haemangiomas [2], percutaneous vertebroplasty has been applied in the treatment of a range of conditions, including osteoporotic crush fractures [3], bone metastases [4] and increasingly for back pain control in myeloma [5].
We have performed a comprehensive review of vertebroplasty for patients with multiple myeloma treated at our tertiary referral centre over a 5-year period between 2004 and 2009.
Materials and methods
Patients
All vertebroplasties performed at the Imperial College Healthcare NHS Trust between 2004 and 2009 were retrospectively reviewed. Patients treated for myeloma were identified and their records reviewed, extracting baseline characteristics, pain score, analgesic regimens pre/post-procedure and complication rates. Where possible, patients were then contacted directly and graded pain score, analgesia use, mobility post-procedure, duration of benefit and performance status assessed using the Eastern Cooperative Oncology Group (ECOG) scale [6]. No patient was excluded from the analysis. The study was performed in accordance with the ethical standards laid down in the Declaration of Helsinki, and patients that were interviewed gave their informed consent.
Vertebroplasty procedure
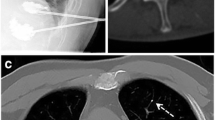
Imaging, including plain radiographs, MRI and isotope bone scan, were reviewed and the vertebra(e) for intervention identified. Vertebroplasty was performed under a short general anaesthetic with the patient in a lateral position under fluoroscopic X-ray guidance. Vertebral access was via a transpeduncular approach (Fig. 1) employing a 7-gauge, 160-mm Gishen bone biopsy needle to inject 1–4 ml of poly(methyl methacrylate) (PMMA) cement. The PMMA cement was made from 9.0 g of Kyphx high-viscosity radio-opaque fluid mixed with 20.0 g of Kyphx cement powder (68% methyl methacrylate–styrene copolymer, 30% barium sulphate and 2% benzoyl peroxide). Post-anaesthetically, all patients were questioned for neurological function and pain level.
a, b Anteroposterior and left lateral views of the insertion of the vertebroplasty needles. One or two needles are placed via a transpeduncular approach and inserted to the area of collapse (frequently the anterior one third of the vertebral body). c, d Placement of the PMMA cement into the vertebra in the same orientations. The cement pathway within the vertebral body follows the low resistance direction. Most procedures are achievable using a single-needle approach
Analysis
Due to the retrospective nature of the study, pre/post-procedure pain scores were on a three-point mild/moderate/severe scale. The patients we contacted were also assessed using a ten-point score. The whole cohort was analysed for reduction in pain score (yes/no); for the 15 patients interviewed, the mean pain score reduction was calculated with P value derivation (Wilcoxon signed-rank test).
Results
Demographics/follow-up
One hundred thirty-two vertebroplasty procedures were performed at the Imperial College Healthcare NHS Trust over the study period. Of these, 26 patients were treated for painful lesions secondary to myeloma. Baseline characteristics are detailed in Table 1. Mean age was 59.3 years, range 42–76 years. Fifty-seven vertebrae were treated between the T6 and L5 levels. Eight patients had a single vertebra treated, five had two and 13 had three levels simultaneously.
Follow-up ranged from 20 days to 42 months, a mean of 19 months. At the time of the study, ten patients had died. As shown in Table 1, 23 of 26 patients received systemic anti-myeloma chemotherapy prior to the vertebroplasty procedure, and 20 of 26 patients were treated with bisphosphonate therapy. Eleven patients received radiotherapy prior to the vertebroplasty and four afterwards. One patient was treated with radiotherapy both prior to and after the vertebroplasty. Two patients had had surgical intervention prior to receiving the vertebroplasty and one after.
Efficacy
Sixty-five per cent of patients rated their pain as severe and 35% as moderate prior to the procedure. Seventy-seven per cent reported a reduction in their pain score after the procedure (Table 1). Seven patients (26%) reported some benefit on waking from the anaesthetic, which then improved further over the following days/weeks. The median time to improvement was 3 days. A reduction in the pain score was reported by 87.5% of the patients if they had one vertebral level treated, 40% if they had two and 77% if three levels were treated. Twelve patients were available for interview. Ten patients had died, one had moved abroad, and three could not be contacted. Of those 12, 11 reported a benefit with a mean reduction in pain score of 4.7/10 (P < 0.003). Where patients reported benefit, it was sustained for a mean of 13.5 months (range, 1.5–35 months). The majority whose pain returned had concurrent progression of myeloma. Fifty-eight per cent of the patients were able to reduce their systemic analgesia: Nine stopped all forms of opiate analgesia and the others reduced their dose by 30–75%. Mean opiate dose reduction was 45.6%. Fifty-eight per cent reported a significant improvement in mobility, and five had an improvement in ECOG score—primarily due to being able to recommence work.
Safety/complications
The procedure was generally very well tolerated. Three patients had a small (<1 ml) cement leak noted at the time of the procedure. Two leaks were associated with increased pain on waking from the anaesthetic, which was uncomplicated and resolved within 24 h. Six others, without cement leak, experienced peri-procedure pain, which again resolved within 24 h. There was no cement or fat emboli, bleeding or infections. The only clinically significant complication was anaesthetic-related respiratory compromise in a patient with preexisting lung problems, which resolved within 72 h.
Discussion
The results of this study serve to confirm and extend those reported in recent literature. We have shown that percutaneous vertebroplasty is a safe and effective modality of treatment, with 77% of recipients reporting a reduction in their pain score that began, in a quarter of patients, as early as waking from the anaesthetic. Our results also show that significant reduction in systemic analgesia is possible, with over one third of patients able to stop all opiate analgesia. The withdrawal of these medications has a positive impact on the patients’ well-being, eliminating troublesome and frequent side effects such as sedation and constipation.
Most studies examining percutaneous vertebroplasty in multiple myeloma have involved limited patient numbers (<15), with the majority of patients being treated at a single vertebral level [7–9]. Fifty per cent of the patients in our study were treated at three vertebral levels simultaneously. It has been postulated that the treatment of multiple levels may improve outcomes due to a lessening of the risk of fracture involving vertebrae neighbouring a cemented level and uncovering pain in adjacent vertebrae [5]. We did not, however, reproduce this finding in our data, perhaps because a larger cohort is required to reveal more subtle differences in treatment effect.
The first, recently reported, randomised controlled studies in osteoporosis were unable to demonstrate the superiority of cementoplasty over a sham procedure [10, 11]. One possible explanation is that natural healing over time accounts for a large proportion of the improvement seen. However, in contrast to osteoporosis, the pathology of myeloma—via the up-regulation of the receptor activator of nuclear factor kappa B (RANK)–RANK ligand interaction, down-regulation of osteoprotegerin and up-regulation of dickkopf-1 [12, 13]—is one of progressive bony destruction and failure of healing mechanisms. It is therefore not possible to extrapolate the results of these trials to the malignant setting.
The myeloma patients treated at our institution were selected for consideration of vertebroplasty on a case-by-case basis, initiated by their treating haematologist who organised imaging consisting of plain X-rays, MRI scan and, in some cases, an isotope bone scan. A referral with the results of these investigations was made to the interventional radiologist who assessed for lesions that may be causing the symptoms that were amenable to treatment. Referral was based on pain refractory to systemic analgesia or requiring unacceptably high/problematic doses of opiates as judged by the patient and haematologist according to symptoms of pain and medication-related side effects. In accordance with our local policy agreed by our haematology and interventional radiology departments, all of our patients were treated with percutaneous vertebroplasty as opposed to balloon kyphoplasty, which involves the injection of cement under lower pressure into a cavity created by balloon inflation within the vertebra being treated. The advantages of each type of procedure is a topic of much debate [9, 14, 15], a full review of which is outside the scope of this article. However, minimal vertebral height gain is the main difference achievable with kyphoplasty. This is, however, usually only a few millimetres and is balanced against longer procedure and, hence, anaesthetic time and higher procedure-related costs.
Patients with acute neurological presentation are not empirically excluded from undergoing therapeutic vertebroplasty at our centre, and three patients in our cohort with acute neurological symptoms, two with cord compression (patients 5 and 10) and one with L3 root compression (patient 11) were treated with vertebroplasty as first-line therapy. All received subsequent radiotherapy and one (patient 10) had surgical fixation 4 months later. Our standard practice includes multidisciplinary team evaluation of patients with neurological deficit involving haematological, neurosurgical and interventional radiology specialists. Percutaneous vertebroplasty may be considered in patients not requiring immediate surgery or with lesions not amenable to surgical fixation as well as for patients not appropriate for surgery based on their performance status. As the experience in our cohort suggests, vertebroplasty can be successfully combined with radiotherapy both prior and afterwards. There is, however, some evidence suggesting that optimal results are achieved by performing vertebroplasty first [16]. As we saw, it has also been successfully employed with surgical instrumentation [17].
As well as a favourable biomechanical profile with an increase in vertebral body strength [18], the possibility of a local anti-tumoural component to PMMA cement treatment [19] has also been reported with cementoplasty, although clearly, any local tumouricidal effects are likely to be insignificant in the anti-myeloma treatment of myeloma which requires a systemic approach. Twenty-three out of 26 of our cohort had received systemic chemotherapy prior to their vertebroplasty. In the three remaining patients, the diagnostic bone biopsy was taken at the same time as the symptomatic vertebral lesion was being treated. Two went on to receive systemic anti-myeloma treatment after the procedure; one patient died before chemotherapy was initiated. Clearly, systemic therapy is a key in the control of myelomatous disease, although from the point of view of bony lesions, it may be inadequate even in combination with bisphosphonate therapy in the control of pain from already damaged vertebrae—as was seen in our cohort.
Of particular relevance when treating myeloma patients, care must be taken to correct for post-vertebroplasty artefact when using imaging, particularly PET/CT, to monitor disease progression [20, 21].
The most serious potential complications of vertebroplasty are cement leakage posteriorly into the spinal canal which may cause nerve root irritation or cord compression and embolisation of either the cement or extravasated fat. Minimising the risk of the latter is why our institution treats a maximum of three levels at one sitting. Small leaks of cement in other directions, i.e. superior/inferior/lateral, are usually irrelevant. Bleeding and infective complications have been consistently low among other studies [8, 18], and we experienced neither in our cohort.
Our study involved the treatment of the thoraco-lumbar spine, although reports of cervical spine treatment, pelvic bones and non-weight-bearing regions, such as the sternum, are emerging [22–24]. We employed a posterolateral approach, although novel approaches including anterior and even trans-oral access of the cervical spine have been reported.
This study was limited by the relatively small number of patients and its retrospective nature. The lack of a prospectively completed questionnaire meant that we relied on a three-point pain score as recorded by the treating physicians in the medical notes at the time. For those patients interviewed, reports of function and pain score could have been affected by recall bias. These limitations could be overcome by future randomised, multicentre, prospectively designed trials.
Conclusion
Despite the results of the first randomised, controlled vertebroplasty trials in osteoporosis, we believe that this procedure is a safe and effective treatment option for painful myelomatous bone disease that is still underutilised within the UK. It can frequently allow for the withdrawal of opiate-based regimens, thus averting their side effects, and, if used as an upfront therapy, may avert prolonged periods of suboptimally controlled pain. Larger scale, prospective, randomised studies are now required to further define the role of this treatment for a patient population that is potentially expanding in line with advances in existing treatment strategies and emerging innovative therapies.
References
Lecouvet FE, Vande Berg BC, Maldague BE, Michaux L, Laterre E, Michaux JL, Ferrant A, Malghem J (1997) Vertebral compression fractures in multiple myeloma. Part I. Distribution and appearance at MR imaging. Radiology 204:195–199
Nicola N, Lins E (1987) Vertebral haemangioma: retrograde embolization–stabilization with methyl methacrylate. Surg Neurol 27:481–486
Deramond H, Saliou G, Aveillan M, Lehmann P, Vallée JN (2006) Respective contributions of vertebroplasty and kyphoplasty to the management of osteoporotic vertebral fractures. Joint Bone Spine 73(6):610–613
Lee B, Franklin I, Lewis JS, Coombes RC, Leonard R, Gishen P, Stebbing J (2009) The efficacy of percutaneous vertebroplasty for vertebral metastases associated with solid malignancies. Eur J Cancer 45(9):1597–1602
Tran Thang N, Abdo G, Martin J-B, Seium-Neberay Y, Yilmaz H, Verbist M-C, Rufenacht D, Sappino A-P, Dietrich P-Y (2008) Percutaneous cementoplasty in multiple myeloma: a valuable adjunct for pain control and ambulation maintenance. Support Care Cancer 16:891–896
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Ramos L, Las Heras JA, Sanchez S, Gonzalez-Porras JR, Gonzalez R, Mateos MV, San Miguel JF (2006) Medium-term results of percuteneous vertebroplasty in multiple myeloma. Eur J Haematol 77:7–13
Cotton A, Dewatre F, Cortet B, Assaker R, Leblond D, Desquesnoy B, Chastanet P, Clarisse J (1996) Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methylmethacrylate at clinical follow-up. Radiology 200:525–530
Bartolozzi B, Nozzoli C, Pandolfo C, Antonioli E, Guizzardi G, Morichi R, Bosi A (2006) Percuteneous vertebroplasty and kyphoplasty in patients with multiple myeloma. Eur J Haematol 76:180–181
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361(6):557–568
Kallmes D, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361(6):569–579
Tian E, Zhan F, Walker R et al (2003) The role of the Wnt/b-catenin signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 349:2483–2494
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350:1655–1664
Movrin I, Vengust R, Komadina (2010) Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a comparison of balloon kyphoplasty and vertebroplasty. Arch Orthop Trauma Surg (in press)
Kose KC, Cebesoy O, Akan B, Altinel L, Dincer D, Yazar T (2006) Functional results of vertebral augmentation techniques in pathological vertebral fractures of myelomatous patients. J Natl Med Assoc 98(10):1654–1658
Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E (1996) Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology 199:241–247
Chakrabarti I, Burton AW, Rao G, Feiz-Erfan I, Hlatky R, Rhines LD, Mendel E (2006) Percutaneous vertebroplasty of a myelomatous compression fracture in the presence of previous posterior instrumentation: report of two cases. J Neurosurg Spine 5:168–171
Oakland RJ, Furtado NR, Timothy J, Hall RM (2008) The biomechanics of vertebroplasty in multiple myeloma and metastatic bladder cancer: a preliminary cadaveric investigation. J Neurosurg Spine 9:439–501
San Milan RD, Burkhardt K, Jean B, Muster M, Martin JB, Bouvier J, Fasel JH, Rufenacht DA, Kurt AM (1999) Pathology findings with acrylic implants. Bone 25:85S–90S
Kuo PH, Cheng DW (2005) Artifactual spinal metastases imaged by PET/CT: a case report. J Nucl Med Technol 33:230–231
Fossaceca R, Di Terlizzi M, Stecco A, Canalis L, Travaglini F, Ambrosini R, Carriero A (2007) MRI post-vertebroplasty. Radiol Med 112:185–194
Rodriguez-Catarino M, Blimark C, Willen J, Mellqvist U, Rodjer S (2007) Percutaneous vertebroplasty at C2: case report of a patient with multiple myeloma and a literature review. Eur Spine J 16(Suppl 3):S242–S249
Zhou B, Wu C, Li M, Gu Y, Cheng Y (2009) Percutaneous osteoplasty for painful sterna lesion from multiple myeloma. Skeletal Radiol 38:281–285
Mont’Alverne F, Vallee J, Guillevin R, Cormier E, Jean B, Rose M, Caldas JG, Chiras J (2009) Percutaneous vertebroplasty for multiple myeloma of the cervical spine. Neuroradiology 51:237–242
Acknowledgements
We would like to thank Dr. Belinda Lee for her advice on patient evaluation and questionnaire and Dr. Richard Szydlo for his help with P value derivation. We would also like to thank Dr. John Garland who read and commented on the manuscript.
Conflict of interest statement
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garland, P., Gishen, P. & Rahemtulla, A. Percutaneous vertebroplasty to treat painful myelomatous vertebral deposits—long-term efficacy outcomes. Ann Hematol 90, 95–100 (2011). https://doi.org/10.1007/s00277-010-1021-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-010-1021-2