Summary
Invasive fungal infections (IFI) are a major cause of morbidity and mortality in patients with haematological malignancies. Antifungal combination therapy is a promising treatment option. However, available data on feasibility, toxicity and efficacy of this therapy are limited. Therefore, this study was conducted to evaluate the feasibility, toxicity and outcome of different antifungal combination therapies. Patients with haematological malignancies receiving antifungal combination therapy for IFI were retrospectively analysed. Toxicity and response were documented at the end of therapy. Survival was evaluated at the end of therapy and after 12 weeks. Fifty-six patients were treated with different antifungal combinations in the period between 2001 and 2007. The majority of patients (63%) received a combination of liposomal amphotericin B and caspofungin as antifungal combination treatment. Toxicity of all applied combinations was tolerable. At the end of combination therapy, favourable response was 65%, whereas unfavourable outcome occurred in 35% of the cases. Mortality at the end of treatment was 11% and 34% 3 months after initiation of combination therapy. Antifungal combination therapy is feasible and efficient in haematological cancer patients and allogeneic stem cell transplant recipients with IFI. Prospective studies to evaluate the optimal combinations are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence, morbidity and mortality of invasive fungal infection (IFI) in patients with haematological malignancies and allogeneic stem cell transplant recipients are high [6, 12, 15, 17, 28, 36]. To improve the clinical course of fungal infection in these high-risk patients, several new antifungal agents have been introduced into clinical practice in recent years. These comprise different formulations of established agents, e.g. liposomal or lipid formulations of amphotericin B deoxycholate and newer triazoles (voriconazole, posaconazole) but also drugs with different modes of action. Here, the echinocandins represent a new class of antifungal drugs with high efficacy and favourable toxicity profile. Whereas polyenes and triazoles target the lipomembrane of the fungus, the echinocandins target the (1→3-)beta-D-glucan synthesis in the fungal cell wall. In vitro studies have proven high efficacy against yeasts and moulds for all of these drugs [8].
However, in the clinical setting, the outcome of fungal infections in highly immunocompromised patients still remained unsatisfying despite the use of these drugs [18, 23, 29].
Another possibility to improve the outcome and thus prognosis in these patients is the combination of these drugs. Antifungal combination therapy has therefore been studied in recent trials [1, 13, 20, 27]. In summary, mortality from fungal infection was lower in these trials when compared with antifungal monotherapy; however, these retrospective analyses were all examining merely one or two different combinations with the echinocandin/polyene combination being the one most extensively studied. Another drawback of these studies are the small patient collectives actually receiving therapy: these were as small as n = 16 in one of the published articles [27].
Up to now, the database for antifungal combination therapy is still limited, despite the increased clinical use of these combinations. To improve certainty of combining antifungal agents with each other, more clinical evidence is needed.
The purpose of this study was therefore to provide additional data for the clinical use of antifungal combination therapies. Thus, we retrospectively examined all antifungal combination therapies (i.e. concomitant start of application of two antifungal drugs), applied in our centre for invasive fungal infection in haematological high-risk patients. These comprise allogeneic stem cell recipients and patients with acute myeloid leukaemia (AML) with prolonged neutropenia. The goal was to determine both efficacy and toxicity of each combination and to evaluate the mortality from fungal infection when antifungal combination therapy was administered.
Patients and methods
All patients enrolled in this retrospective trial were treated in the Department of Haematology/Oncology at the University of Munich for haematological malignancies between 2001 and 2007. The data obtained for this study were collected by retrospective chart review. Data were obtained following a methodological protocol for the evaluation of antifungal therapy.
All patients were given high-dose chemotherapy for remission induction in AML or were receiving allogeneic stem cell transplantation after the appropriate conditioning regimens. All patients were 18 years of age or older and had received prior antifungal prophylaxis or secondary prophylaxis as single agent antifungal chemotherapy without having the established diagnosis of invasive fungal infection. Primary prophylaxis comprised itraconazole, fluconazole or posaconazole. Six patients who were treated with secondary prophylaxis received either voriconazole or itraconazole. Patients entering the study were therefore treated with first-line antifungal combination therapy when suffering from IFI.
The diagnosis of invasive fungal infection was established according to the EORTC/MSG-criteria [3]. Proven and probable IFI was considered “documented” IFI in contrast to possible IFI. Patients had to receive at least 3 days of combination therapy for inclusion into analysis. Patients who received first-line combination therapy without previous prophylaxis or who had received combination therapy for less than 3 days or who had been treated with antifungal combination therapy ever before were not eligible.
Sequential combination treatment (i.e. addition of a second antifungal drug to a pre-existing antimycotic therapy) was also not allowed for the introduction into the trial. All combination partners had to be started within 24 h after the application of the first drug.
Information collected included demographic data, underlying disease, cytoreductive therapy and/or transplant setting, clinical, microbiological, pathological and radiographic findings, antifungal treatment and laboratory data.
Risk factors for IFI—such as prolonged steroid use, recent history of neutropenia, graft-versus-host disease or use of T cell suppressants—were also documented.
Definitions
Haematological and non-haematological toxicity was evaluated in accordance to the WHO/CTC criteria at the end of treatment (EOT) with antifungal combination therapy.
Complete and partial responses were considered to be favourable outcomes, whereas stable disease and progression of IFI were regarded to be treatment failures. Response was defined as resolution (complete remission, CR) or major improvement (partial remission, PR) of clinical, radiological and/or microbiological signs, depending on the previous diagnostic findings. Any deterioration documented at the end of treatment was defined as progression of the fungal infection.
Death attributable to fungal infection was only documented when pathological or microbiological proof of fungal pathogens was found in autopsy.
Statistical analysis
All data were entered in an Excel database (Microsoft Office Excel 2003, Microsoft Corporation, USA, 2003).
For statistical analysis, the program Statistica 6.1 (StatSoft, Inc., Tulsa, OK, USA) was used. The overall survival was analysed with Kaplan–Meier curves and comparison between the different treatment groups was done using the log-rank test.
Results
Patients
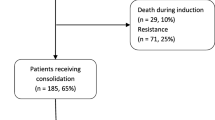
We identified 56 patients (34 male, 22 female) who received antifungal combination therapy for 3 or more days following antifungal prophylaxis at our institution between September 2001 and May 2007. Median age of patients included into the analysis was 46 years [range 20–69 years]. They were treated for haematological malignancies with either high-dose chemotherapy for remission induction or allogeneic stem cell transplantation. Table 1 shows the underlying diseases, antifungal prophylaxis and transplant settings of the patients.
At the onset of antifungal combination therapy, 55 patients were febrile, 37 patients (66%) were suffering of severe (≥III°) graft-versus-host disease (GvHD) and were receiving corticosteroids in combination with other immunosuppressants within the last 14 days. Thirty-two patients (57%) were suffering from neutropenia (absolute neutrophil count ≤500/μl) at that time. Median time to start of antifungal combination therapy after allogeneic stem cell transplantation was 22 days [range 22–772 days].
Possible invasive fungal infection was documented in 11 patients (20%); documented IFI was seen in 45 patients (80%), with 15 patients suffering from probable and 30 patients suffering from proven IFI (Table 2 displays the categories of IFI in the cohort).
The majority of fungal infections were seen in the lungs, although there were a number of cases in the possible group, which could not be further allocated to a specific site of infection.
Underlying pathogens of the documented invasive fungal infections were Aspergillus spp. in 35 of the 45 patients (78%). Candida spp. were identified in ten of the 45 patients (22%): all of these were blood stream infections and thus led to the diagnosis of proven IFI. Table 2 depicts the localisation of fungal infections in the patients as well as the underlying pathogens and the corresponding EORTC criteria.
Proof of the underlying pathogen was not available in patients categorised as “possible” IFI.
Antifungal combination therapy
The median duration of antifungal combination therapy was 16 days [range 3–131 days]. The most common antifungal combination was liposomal amphotericin B (L-AmB) given concomitantly with caspofungin (35 pts, 63%), followed by caspofungin/voriconazole which was administered in 12 patients (21%). Four patients received a combination of L-AmB/voriconazole (7%) and five patients (9%) received different triazole (fluconazole, itraconazole or posaconazole)/polyene (L-amphotericin B) regimens.
All patients receiving a caspofungin-containing therapy were given the 70 mg loading dose on day 1, followed by 50 mg/day starting from day 2. The median polyene dosage (L-amphotericin B and amphotericin B deoxycholate) was 3 mg/kg per day [minimum 1 mg/kg, maximum 5 mg/kg]. Voriconazole was administered in approved dosage (6 mg/kg twice daily as loading dose, followed by 4 mg/kg twice daily from day 2) and all drugs were given intravenously in the documented patients.
Toxicity
We collected laboratory data of all patients at the onset of the combination therapy and at the end of treatment. Serum creatinine levels taken for the measurement of renal toxicity, bilirubin, transaminases, alkaline phosphatase and gamma-GT were used as monitors of liver toxicity.
Six patients had an increased serum creatinine level before the onset of antifungal combination. Five of these patients also showed increased creatinine levels at the end of treatment. Whether this is due to antifungal therapy cannot be evaluated. Four of these patients received polyene-containing therapy, but the administered dosage was reduced to 1 mg/kg per day. One patient with highly elevated baseline creatinine (4.6 mg/dl) was treated with the caspofungin/voriconazole regimen. The median overall serum creatinine level at the start of therapy was 0.9 mg/dl [minimum 0.3 mg/dl; maximum 4.6 mg/dl] and 1.0 mg/dl at the end [minimum 0.4 mg/dl; maximum 3.8 mg/dl]. Mild to moderate renal toxicity occurred in nine patients (16%) while on combination therapy.
Thirty-three patients had a pre-existing liver impairment. These patients had an increased bilirubin level, elevated transaminases, alkaline phosphatase, gamma-GT or a combination of these. All of these patients were suffering from GvHD of the liver.
In particular, 19 patients experienced deteriorations of the serum bilirubin level. In seven patients, this may be due to the application of antifungal combination therapy. Gamma-GT levels at the initiation of antifungal treatment were increased in 32 patients. Ten of these patients experienced a further increase during the examined treatment period. In general, the changes of the abovementioned parameters during the treatment were small (median bilirubin 1.9 vs. 1.4 mg/dl, gamma-GT 109 vs. 184 IU/l, GOT 23 vs. 35 IU/l, GPT 32 vs. 48 IU/l, aP 157 vs. 214 IU/l). In no patient combination therapy had to be stopped for severe toxicity. Figure 1 depicts the toxicity data at baseline and end of treatment in the cohort. There was no statistically significant increase in any of the examined parameters.
Efficacy
At the end of combination treatment (EOT), 36 patients (65%) showed a favourable response (complete and partial response). Unfavourable responses were seen in 20 patients (35%): stable disease was seen in five (9%) patients and progression of disease was documented in 15 patients (27%). Of these patients, six (11%) died during treatment after an average of 20 days on combination therapy, and autopsy proved fungal infection as cause of death in five of these patients. Patients showing progression at EOT (without the patients who died) were distributed among the different treatment groups as follows: 13 patients (37%) in the L-AmB/caspofungin group, one patient (8%) in the caspofungin/voriconazole group and one patient (25%) in the L-AmB/voriconazole group. Noteworthy, all except one patient who showed an unfavourable response at EOT (i.e. stable disease or progression) died in the follow-up period.
Survival
Overall survival was 44% (16/36 patients) in the patients with favourable response. Moreover, 14/15 patients (93%) that did not respond favourably to the combination therapy died in the follow-up period. The median follow-up period was 8 months [range 3–1,111 days]. At the end of treatment, six patients (11%) were dead. Ninety days after the start of treatment, mortality was 34% (19 pts). Figure 2 depicts the survival rates at the beginning of antifungal combination therapy and on days 30, 90 and 120 after initiation of antifungal combination therapy. Median overall survival was 6.3 months (Fig. 3).
Figure 4 depicts the survival according to the different treatment groups. The subgroup treated with caspofungin/voriconazole (n = 12) showed the best results with its median survival not yet reached. The second best survival was seen in the L-AmB/triazole group (n = 9); again, median survival was not reached. The largest group comprised 35 patients treated with L-AmB/caspofungin. In this subgroup, the median survival was about 5 months.
Discussion
The prognosis of antifungal monotherapy for invasive fungal infections remains poor despite the implementation of new antifungal agents [7, 29, 32]. Antifungal combination therapy has therefore recently received increasing attention, but only a few clinical trials examining the role of combination therapy in invasive fungal infections have been published in the last 5 years [20, 24, 27]. All of these studies examined specific combination therapies with echinocandin/polyene combinations or concomitant use of echinocandins and triazoles, mostly in patients with invasive aspergillosis. The only trial examining two different combinations was published by Maertens and colleagues last year. This study evaluated a combination of caspofungin with either polyenes or triazoles and was also one of the only two published prospective trials on this topic [24].
Still, the evaluation of antifungal combination therapy is a demanding task. Some of the combinations are assumed to feature relevant antagonism (or at least no synergy), as concomitant application of polyenes with triazoles have shown antagonistic effects in vitro [21, 31, 33]. Recent studies, however, put that subject into perspective and clear clinical data are missing [10, 19]. Hence, it is not clear whether such antagonism exists in vivo.
The present trial, being the first to investigate more than two combination regimens, evaluates all combination therapies actually applied in our hospital during the last 6 years to determine their feasibility, efficacy and toxicity in haematological patients with invasive fungal infections. The study utilises a large patient cohort with a very high incidence of documented IFI for analysing different antifungal combination therapies in high-risk patients.
We evaluated 56 patients receiving any antifungal combination therapy during the period of 2001 to 2007. All patients were at a high risk for the development of IFI, as they comprise a critically ill population with a high incidence of negative prognostic factors such as mismatch allogeneic stem cell transplantation, high-dose steroids, etc. At the baseline of combination therapy, most patients were neutropenic or suffered from severe graft-versus-host disease, with 86% of the enrolled patients being allogeneic stem cell transplant recipients.
In our study, the majority of patients were diagnosed with proven IFI (53%). In most previous combination therapy studies, the portion of definite cases of invasive fungal infection ranged between 20% and 40% [1, 20, 27]. In the study of Marr et al. [27], the incidence of proven IFI was slightly higher, but the number of patients actually receiving antifungal combination therapy was rather small (n = 16) as compared to our cohort.
Moreover, the underlying fungal pathogen in the previous studies was often not known but assumed to be Aspergillus spp. In everyday practice, the assurance of the pathogen is a major concern, as sometimes diagnostic procedures are failing to identify the underlying pathogen at all [22, 26, 30, 35, 36].
In our cohort, we identified ten patients with proven Candida infection. Although Candida species are no longer the “number one cause of IFI” in haematological patients [12], yeast infections still are a major threat to immunosuppressed patients. Hence, we found it important to evaluate both patients with invasive mould infections and patients suffering from invasive yeast infections although these two species have a different prognosis. All patients in our study with Candida infections responded favourably to combination therapy. Patients showing treatment failure or death at the end of treatment were all documented cases of invasive aspergillosis.
The majority of the patients evaluated in this study were treated with an L-AmB/caspofungin combination. This regimen has been studied most extensively in previous trials and has shown good efficacy and feasibility [1, 20, 24]. The polyene/echinocandin combination is very attractive because of data suggesting additive effects in animal models and in clinical trials [2, 4, 11, 14].
In our study, we found a favourable toxicity profile for this combination as well as for the other treatment regimens applied. No patient had to be withdrawn from combination therapy because of severe liver toxicity or renal failure in the polyene/echinocandin group.
We identified nine patients receiving a polyene/triazole combination in our retrospective cohort. This combination has never been studied in the clinical setting before because of contrarily balanced in vitro studies that suggest antagonistic effects for the concomitant use of polyenes with azoles. In our centre, none of the patients displayed severe toxicity or had to be withdrawn from this regimen. The combination of polyenes with triazoles was feasible and the outcome and overall survival in this subgroup were comparable to the other treatment groups. Only one of these patients (11%) showed unfavourable response although five of the patients (56%) were classified as documented IFI. According to our data, the use of this combination seems clinically applicable despite the former assumption of weak efficacy. Whether this combination is associated with higher efficacy rates or reduced mortality from invasive fungal infection has to be evaluated in further randomised trials.
In the caspofungin/voriconazole group, there was no treatment-related toxicity higher than grade 2 according to WHO/CTC criteria. The most common events were liver toxicity, which could also be caused by pre-existing graft-versus-host disease in some patients.
Due to the fact that this is a retrospective study, further investigations of the causative mechanisms of increased laboratory data were not possible for any treatment group.
With an overall favourable response of 65% at the end of treatment, the efficacy rate is comparable to those published in recent studies on combination therapy. The efficacy levels of these lately published trials range between 48% and 60%. Aliff et al. reached similar results with an overall favourable response of 60%, but the proportion of definite cases of IFI was considerably lower than in our trial [1, 24]. The other published studies examining the efficacy of the polyene/echinocandin treatment also included mainly patients with acute leukaemia, but the proportion of patients with proven IFI was sometimes as small as five patients [20]. These trials showed slightly lower favourable response rates at the end of combination therapy but similar survival.
Moreover, the duration of antifungal combination therapy was different in many previous trials. Some of the patients received antifungal combination for 1 day only [20, 24], whereas in one study the minimum duration on antifungal combination therapy needed to be 7 days [9]. Whether these timeframes really represent a treatment period in which the toxicity and/or efficacy of antifungal combination treatment can be evaluated is not known. In our cohort, the shortest duration of antifungal combination therapy was 3 days.
In this study, we evaluated a large cohort of patients with haematological malignancy suffering from invasive fungal infections treated with three different antifungal combination regimens. The probability of survival in our cohort was better in all three subgroups than most of the published data on antifungal monotherapy in haematological patients and stem cell transplant recipients with invasive fungal infections [5, 28, 34]. Only voriconazole monotherapy has shown higher survival rates at week 12 in the study of Herbrecht and colleagues, when voriconazole was compared with conventional amphotericin B in primary therapy of invasive aspergillosis [16].
Still, the various treatment groups in our cohort were too small to reach statistically significant results for superiority or inferiority for each of the combinations used. In particular, we found, that the concomitant application of polyenes and triazoles is effective, although in vitro data show critical antagonism of this combination. The combination most commonly used consisted of a liposomal polyene and an echinocandin. These drugs have shown good efficacy in studies on antifungal monotherapy in haematological patients as well as in previous trials on combination therapy and have again been shown to be efficacious in our trial [9, 25].
The toxicity of antifungal combination therapy did not lead to the termination of treatment in any of the combinations used. Increased serum levels of bilirubin, alkaline phosphatase, transaminases and creatinine were seen in the cohort, but were induced mainly by severe graft-versus-host disease or transient renal impairment and did not significantly deteriorate during therapy. Although the majority of the patients died in the follow-up period, the efficacy and toxicity at the end of antifungal combination therapy seems favourable.
The heterogeneity of our cohort and the differences in the three evaluated combinations display the need of further investigation of combination therapies and the overcoming of long-known prejudices in antifungal treatment strategies.
Conclusions
Antifungal combination therapy is increasingly applied in clinical practice although specific recommendations for such treatment are still lacking. Our data show that concomitant use of all classes of antifungal drugs is feasible for first-line or salvage therapy in haematological high-risk patients. The risk of treatment-related toxicity is moderate if antifungal drugs are applied in approved dosage. Response rates and mortality in our cohort were better than those of antifungal monotherapy published in previous trials. If antifungal combination therapy should routinely be adopted in the management of these patients, however, has to be further evaluated. Then, risk-adapted strategies with antifungal combination therapy can be implemented into clinical practice.
References
Aliff TB, Maslak PG, Jurcic JG et al (2003) Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer 97:1025–1032 doi:10.1002/cncr.11115
Arikan S, Lozano-Chiu M, Paetznick V et al (2002) In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother 46:245–247 doi:10.1128/AAC.46.1.245-247.2002
Ascioglu S, Rex JH, de Pauw B et al (2002) Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 34:7–14 doi:10.1086/323335
Barchiesi F, Spreghini E, Tomassetti S et al (2007) Caspofungin in combination with amphotericin B against Candida parapsilosis. Antimicrob Agents Chemother 51:941–945 doi:10.1128/AAC.00880-06
Bhatti Z, Shaukat A, Almyroudis NG et al (2006) Review of epidemiology, diagnosis, and treatment of invasive mould infections in allogeneic hematopoietic stem cell transplant recipients. Mycopathologia 162:1–15 doi:10.1007/s11046-006-0025-x
Bodey G, Bueltmann B, Duguid W et al (1992) Fungal infections in cancer patients: an international autopsy survey. Eur J Clin Microbiol Infect Dis 11:99–109 doi:10.1007/BF01967060
Bodey GP, Mardani M, Hanna HA et al (2002) The epidemiology of Candida glabrata and Candida albicans fungemia in immunocompromised patients with cancer. Am J Med 112:380–385 doi:10.1016/S0002-9343(01)01130-5
Bowman JC, Hicks PS, Kurtz MB et al (2002) The antifungal echinocandin caspofungin acetate kills growing cells of Aspergillus fumigatus in vitro. Antimicrob Agents Chemother 46:3001–3012 doi:10.1128/AAC.46.9.3001-3012.2002
Caillot D, Thiebaut A, Herbrecht R et al (2007) Liposomal amphotericin B in combination with caspofungin for invasive aspergillosis in patients with hematologic malignancies: a randomized pilot study (Combistrat trial). Cancer 110:2740–2746 doi:10.1002/cncr.23109
Clemons KV, Espiritu M, Parmar R et al (2005) Comparative efficacies of conventional amphotericin b, liposomal amphotericin B (AmBisome), caspofungin, micafungin, and voriconazole alone and in combination against experimental murine central nervous system aspergillosis. Antimicrob Agents Chemother 49:4867–4875 doi:10.1128/AAC.49.12.4867-4875.2005
Cuenca-Estrella M, Gomez-Lopez A, Garcia-Effron G et al (2005) Combined activity in vitro of caspofungin, amphotericin B, and azole agents against itraconazole-resistant clinical isolates of Aspergillus fumigatus. Antimicrob Agents Chemother 49:1232–1235 doi:10.1128/AAC.49.3.1232-1235.2005
Denning DW, Marinus A, Cohen J et al (1998) An EORTC multicentre prospective survey of invasive aspergillosis in haematological patients: diagnosis and therapeutic outcome. EORTC Invasive Fungal Infections Cooperative Group. J Infect 37:173–180 doi:10.1016/S0163-4453(98)80173-4
Denning DW, Marr KA, Lau WM et al (2006) Micafungin (FK463), alone or in combination with other systemic antifungal agents, for the treatment of acute invasive aspergillosis. J Infect 53:337–349 doi:10.1016/j.jinf.2006.03.003
Graybill JR, Bocanegra R, Gonzalez GM et al (2003) Combination antifungal therapy of murine aspergillosis: liposomal amphotericin B and micafungin. J Antimicrob Chemother 52:656–662 doi:10.1093/jac/dkg425
Groll AH, Shah PM, Mentzel C et al (1996) Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect 33:23–32 doi:10.1016/S0163-4453(96)92700-0
Herbrecht R, Denning DW, Patterson TF et al (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415 doi:10.1056/NEJMoa020191
Jantunen E, Ruutu P, Niskanen L et al (1997) Incidence and risk factors for invasive fungal infections in allogeneic BMT recipients. Bone Marrow Transplant 19:801–808 doi:10.1038/sj.bmt.1700737
Jantunen E, Ruutu P, Piilonen A et al (2000) Treatment and outcome of invasive Aspergillus infections in allogeneic BMT recipients. Bone Marrow Transplant 26:759–762 doi:10.1038/sj.bmt.1702604
Kirkpatrick WR, Coco BJ, Patterson TF (2006) Sequential or combination antifungal therapy with voriconazole and liposomal amphotericin B in a Guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother 50:1567–1569 doi:10.1128/AAC.50.4.1567-1569.2006
Kontoyiannis DP, Hachem R, Lewis RE et al (2003) Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer 98:292–299 doi:10.1002/cncr.11479
Kontoyiannis DP, Lewis RE, Sagar N et al (2000) Itraconazole-amphotericin B antagonism in Aspergillus fumigatus: an E-test-based strategy. Antimicrob Agents Chemother 44:2915–2918 doi:10.1128/AAC.44.10.2915-2918.2000
Lin MT, Lu HC, Chen WL (2001) Improving efficacy of antifungal therapy by polymerase chain reaction-based strategy among febrile patients with neutropenia and cancer. Clin Infect Dis 33:1621–1627 doi:10.1086/322631
Lin SJ, Schranz J, Teutsch SM (2001) Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis 32:358–366 doi:10.1086/318483
Maertens J, Glasmacher A, Herbrecht R et al (2006) Multicenter, noncomparative study of caspofungin in combination with other antifungals as salvage therapy in adults with invasive aspergillosis. Cancer 107:2888–2897 doi:10.1002/cncr.22348
Maertens J, Raad I, Petrikkos G et al (2004) Efficacy and safety of caspofungin for treatment of invasive aspergillosis in patients refractory to or intolerant of conventional antifungal therapy. Clin Infect Dis 39:1563–1571 doi:10.1086/423381
Maertens J, Verhaegen J, Lagrou K et al (2001) Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood 97:1604–1610 doi:10.1182/blood.V97.6.1604
Marr KA, Boeckh M, Carter RA et al (2004) Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis 39:797–802 doi:10.1086/423380
Marr KA, Carter RA, Crippa F et al (2002) Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 34:909–917 doi:10.1086/339202
Metcalf SC, Dockrell DH (2007) Improved outcomes associated with advances in therapy for invasive fungal infections in immunocompromised hosts. J Infect 55:287–299 doi:10.1016/j.jinf.2007.06.012
Obayashi T, Yoshida M, Mori T et al (1995) Plasma (1®3)-beta-D-glucan measurement in diagnosis of invasive deep mycosis and fungal febrile episodes. Lancet 345:17–20 doi:10.1016/S0140-6736(95)91152-9
Pahls S, Schaffner A (1994) Aspergillus fumigatus pneumonia in neutropenic patients receiving fluconazole for infection due to Candida species: is amphotericin B combined with fluconazole the appropriate answer. Clin Infect Dis 18:484–486
Patterson TF (2005) Advances and challenges in management of invasive mycoses. Lancet 366:1013–1025 doi:10.1016/S0140-6736(05)67381-3
Schaffner A, Bohler A (1993) Amphotericin B refractory aspergillosis after itraconazole: evidence for significant antagonism. Mycoses 36:421–424
Shaukat A, Bakri F, Young P et al (2005) Invasive filamentous fungal infections in allogeneic hematopoietic stem cell transplant recipients after recovery from neutropenia: clinical, radiologic, and pathologic characteristics. Mycopathologia 159:181–188 doi:10.1007/s11046-004-5495-0
White PL, Linton CJ, Perry MD et al (2006) The evolution and evaluation of a whole blood polymerase chain reaction assay for the detection of invasive aspergillosis in hematology patients in a routine clinical setting. Clin Infect Dis 42:479–486 doi:10.1086/499949
Yoshida M, Tsubaki K, Kobayashi T et al (1999) Infectious complications during remission induction therapy in 577 patients with acute myeloid leukemia in the Japan Adult Leukemia Study Group studies between 1987 and 1991. Int J Hematol 70:261–267
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rieger, C.T., Ostermann, H., Kolb, HJ. et al. A clinical cohort trial of antifungal combination therapy: efficacy and toxicity in haematological cancer patients. Ann Hematol 87, 915–922 (2008). https://doi.org/10.1007/s00277-008-0534-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-008-0534-4