Abstract
Lupus anticoagulants (LA) are a surrogate marker for the risk of thromboembolic disease (TE). However, not all individuals with LA acquire TE, and it is desirable to distinguish those at risk for TE from those without. Platelets polymorphisms may contribute to the risk of TE, mainly those of glycoprotein (GP)Ibα: these are the variable number of tandem repeats (VNTR) and a dimorphism in the Kozak region, which affect platelet plug formation in healthy individuals under high shear stress rates. We determined polymorphisms within the GPIbα in individuals with persistent LA and a history of TE (LA/TE+) and in those without TE (LA/TE-). Further, we measured platelet function, as estimated by the collagen-epinephrine closure time (CEPI-CT) of the platelet function analyzer PFA-100 and compared all data with healthy controls. There was no difference of the VNTR alleles compared to healthy controls. The (−5)C allele of the Kozak dimorphism was significantly more frequent in LA patients compared to controls (p = 0.04), as a result of its increased frequency in LA/TE+ (vs controls p = 0.04), but there was no difference between LA/TE+ and LA/TE−. The increased frequency of the (−5)C allele resulted in an overrepresentation of (−5)TC genotype in the LA/TE+ group (p = 0.02) but not in a subgroup of 18 patients with arterial disease. The CEPI-CT of the PFA-100 was shorter in LA/TE+ than in LA/TE− (p = 0.044), but this difference did not persist after exclusion of patients with low platelet counts or low ristocetin cofactor activity. Unlike in healthy individuals, the CEPI-CT was not related to any Kozak dimorphism, neither in LA/TE−, nor in LA/TE+. Thus, the Kozak dimorphism may just contribute to stronger factors disposing individuals with LA towards TE without any discernible effect on their in vitro platelet function estimated by the PFA-100.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lupus anticoagulants (LA) belong to a group of antiphospholipid autoantibodies and are commonly detected through their ability to prolong phospholipid dependent coagulation tests. Antiphospholipid antibodies bind to complexes of negatively charged phospholipids and plasma proteins. LA are common in patients with an antiphospholipid syndrome (APS), and are associated with thromboembolic disease (TE), recurrent spontaneous abortion, and thrombocytopenia [1]. The precise mechanisms for the development of clinical disease are not clear yet. Interestingly, LA are also detected in 1 to 5% of healthy individuals [2]. It is therefore important to differentiate between individuals with LA who are at risk for TE and those who are not. Increased levels of anti-β2-GPI IgG were associated with thrombosis in patients postive for LA [3].
Whether platelets play a role for the development of TE in patients with LA is not clear. There is evidence that LA bind to the phospholipid/plasma protein complex on activated platelet membranes , and thus, influence platelet activation and aggregation [4–11]. Further, monoclonal anti-β2-glycoprotein (GP) I antibodies with LA activity have been shown to bind to platelet membranes in the presence of β2-GP I and lead to platelet activation in the presence of other agonists [12]. Increased levels of anti-β2-GPI IgG were associated with thrombosis in patients positive for LA [3]. Further, findings of increased platelet PAC-1 binding and of CD63 expression [7], strongly suggest that platelets are poised for coagulation in LA patients.
The extent to which platelets respond to various agonists to become activated varies from one individual to the next. It has been shown that some of this variability is associated with inherited polymorphisms of the involved GP complexes Ib/IX/V, Ia/IIa, and IIb/IIIa [13]. Accordingly, some of these inherited polymorphisms have been associated with an increased risk for TE [13, 14].
The platelet GPIbα is the major platelet receptor mediating shear stress induced adhesion and activation. Thus, genetic polymorphisms within this receptor are regarded key candidates to influence its function. These are the variable number of tandem repeats (VNTR), which result from the presence of one to four tandem repeats of a 13-amino acid sequence in the macroglycopeptide region (VNTR A, B, C, or D from largest to smallest) [15], and the Kozak dimorphism, caused by a single nucleotide substitution [(−5)TC] in the Kozak sequence in the GPIbα chain [16]. Whether or not these genetic polymorphisms are associated with an increased risk for TE is controversial [13]. We have shown that the latter polymorphism affects platelet plug formation in healthy individuals under high shear stress rates [17]. We, therefore, were interested to compare allelic frequencies from healthy controls with individuals with LA with a history of TE and those without TE. Assuming that in LA patients, like in healthy individuals, these polymorphisms will influence platelet function, and thus, contribute to thrombotic disease, we evaluated their association with platelet plug formation under high shear stress rates.
Patients
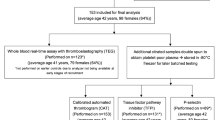
One hundred patients with persistent LA antibodies were included in our study from February 2001 to November 2003. Their clinical characteristics as well as hereditary and acquired risk factors for TE are shown in Table 1. Sixty-seven patients (54 women) had a history of thromboembolic events (group LA/TE+). Their median age at diagnosis of LA was 35.5 years (range, 11.4–77.4 years) and the median age at study entry was 39.7 years (17.1–78.3 years). Thirty-three patients (24 women) without a previous thrombosis (group LA/TE−) were median 53.2 years old (range, 13.4–81.2 years) at diagnosis of LA and median 57.8 years (range, 19.8–86.1 years) at inclusion. In these latter patients, LA was discovered at a routine preoperative coagulation test or with the evaluation of systemic lupus erythematosus (SLE). Fourteen patients (10 LA/TE+ and four LA/TE−) fulfilled the criteria for SLE [18]. The period since the detection of LA until inclusion for this study was similar in both groups (LA/TE− median, 2.4 years; range, 0.8–35.6 years; LA/TE+ median, 3.0 years; range, 0.8–26.3 years; p > 0.05). At the time of the study, 51 LA/TE+ patients and one of the LA/TE− patients received oral anticoagulation by vitamin K antagonists. Four LA/TE+ patients and three LA/TE− patients were under steroid therapy. Two LA/TE+ patients received immunosuppressive therapy.
None of the patients had taken any drugs known to affect platelet function for the last 2 weeks before blood sampling. Two hundred thirty-three healthy individuals (99 women; median age 33 years; range, 27–42 years), who were investigated during the same time period as the LA patients served as controls [17]. Informed consent was obtained from all individuals before entry into the study, which had been approved by the Ethics Committee of the Medical University of Vienna.
Materials and methods
LA testing was performed within 3 h of blood sampling. LA was diagnosed according to the criteria proposed by the Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis [19], by using two different screening assays, activated partial thromboplastin time (PTT LA-reagent, Diagnostica Stago, Asniere sur Seine, France) and diluted Russel’s viper venom time (DVVT, Gradipore, North Ryde, Australia), mixing tests and confirmatory tests, as described previously [20]. At least two detections of LA antibodies in a period of at least 3 months were required for the definition of persistent LA.
The polymorphisms within the platelet GPIbα were determined by our previously published methodology and results were compared to the published data in 233 healthy controls [17].
High-shear-induced platelet plug formation was tested using the platelet function analyzer PFA-100 (Dade Behring, Marburg, Germany). The PFA-100 measures the time needed for a platelet plug to form after activation of platelets by pathophysiologically relevant stimuli, namely collagen and adenosine diphosphate (CADP) or collagen and epinephrine (CEPI) [21]. We determined both shear-stress induced closure times (CADP-CT, CEPI-CT), but CEPI-CT was used as the primary outcome variable, because it is the more sensitive indicator for platelet function, and the results allowed us comparisons with data that we had obtained in healthy controls [17, 22] at the same time as in LA individuals. Single determinations were performed in one batch of cartridges. Individual day-to-day variability in healthy subjects is 9–12%. Low von Willebrand factor antigen (vWFAg) levels and ristocetin cofactor activity (RiCo) may affect PFA-100 values. Therefore, blood was drawn without venostasis at the same time and under the same conditions as blood for the PFA-100 measurements for the assessment of vWFAg and RiCo. All samples were collected into evacuated tubes containing 129 mmol/l buffered sodium citrate (3.8%, Vacuette tubes, Greiner Bio-One, Kremsmünster, Austria). vWFAg was measured with a fully automated simultaneous thermal analyzer using the STA Liatest vWF (Diagnostica Stago, Paris, France). Plasma activity of RiCo was assayed by turbidometry using a commercial kit (BC von Willebrand reagent; Behring Marburg, Germany), which consists of lyophilized platelets and ristocetin, using the Behring Coagulation System (Behring) [23].
Platelet antibodies against GPIb/IX were determined by MAIPA, as described previously [24].
Statistical analyses
Chi-square test was used for comparison of categorical variables between groups. Mann–Whitney-U test was applied to compare metric variables between two groups, Kruskal–Wallis test to compare more than two groups, respectively. Correlations were calculated in nonparametric Spearman test. Odds ratios (OR) and corresponding 95% confidence intervals (CI) were calculated by binary logistic regression analysis comparing homozygous carriers of the (−5)T-allele of the Kozak polymorphism with carriers of the C-allele (CT and CC). Age was added in bivariate binary logistic regression models. A two-sided p value of less than 0.05 was considered to indicate statistical significance. All analyses were performed with the statistical software package SPSS for Windows.
Results
Allelic frequencies of the GPIbα polymorphisms VNTR and within the Kozak region in the two patients’ groups and healthy controls are shown in Table 2. The latter are similar to data in other Caucasoid populations [13] and were in all groups in Hardy–Weinberg equilibrium (Table 2). While allelic frequencies of the VNTR in patients did not differ from healthy controls (p = 0.45), we observed a significant deviation of the allelic frequencies within the Kozak region (p = 0.047). We, therefore, further compared these frequencies in healthy controls with those from LA/TE+ and LA/TE− individuals separately. There was no difference discernible between healthy controls and the LA/TE− group (p = 0.577). However, there was a significant predominance of the (−5)C allele in the LA/TE+ group compared to controls (p = 0.044).There was no difference between LA/TE+ and LA/TE−. The statistical power to detect a significant difference between LA/TE+ (n = 67) and LA/TE− (n = 33) was 8%. The (−5)C allele was associated with a twofold increased risk for thrombosis compared to controls (OR 2.0; 95% CI, 1.1–3.5; p = 0.02), as it resulted in significantly more (−5)TC in the LA/TE+ than in healthy controls (36% vs 22%, Table 3). No statistically significant odds ratio for thrombosis (LA/TE+ vs LA/TE−) was calculated for (−5)CC+CT genotypes compared to (−5)TT in a bivariate logistic regression analysis adjusted for age at the time of thrombosis (OR 1.3; 95% CI, 0.5–3.4; p = 0.53). As platelets play a major role in arteriosclerosis, we were interested to see if the observed allelic deviation in the LA/TE+ group is a result of an increased frequency of the (−5)C allele in the subgroup of 18 patients with a history of arterial TE disease. However, such a predominance of the (−5)C allele was not discernible (p = 0.77).
Applying the platelet function analyzer PFA-100 in healthy individuals, we have observed shorter CEPI-CT in homozygotes with the (−5)TT vs (−5)TC Kozak genotype [17]. Similar to these healthy individuals, we expected shorter CEPI-CT in individuals from the LA/TE− group of the (−5)TT genotype than the (−5)TC genotype. In the LA/TE+ group such an influence of the genotype may be diminished, but we expected overall shortened CEPI-CT in the whole group. There was a significant correlation between CADP-CT and CEPI-CT in both patients’ groups (p = 0.002). CEPI-CT was shorter in LA/TE+ than LA/TE− (LA/TE+ median, 152 s; range, 101–300 s; LA/TE− median, 172 s; range, 69–300 s; p = 0.044). Of note, in both LA groups, we observed prolonged CEPI-CT compared to the respective genotype in healthy controls (Table 3). These were in LA/TE− (−5)TT, and (−5)TC 10 and two individuals, respectively; in LA/TE+ 12 and four patients, respectively, after excluding individuals with platelet counts less than 100 × 109/l, which may already affect the results from the PFA-100 (LA/TE− n = 3, LA/TE+ n = 1). [25] The median CEPI-CT in the two patients’ goups were hardly affected by exclusion of these six patients with platelet counts less than 100 × 109/l. (LA/TE− median, 168 s; range, 60–300 s; LA/TE+ median, 153 s; range, 101–300 s). The prolonged CEPI-CT were not explained by low vWFAg, which was within the normal range (60–180%) in all individuals (LA/TE− median, 130%; range, 64–339%; LA/TE+ median, 156%; range, 70–478%; p = 0.042). However, low RiCo was noted in three LA/TE− individuals with prolonged CEPI-CT, who were therefore excluded from further comparisons. Low RiCo was seen in one LA/TE+ subject with a normal CEPI-CT (not excluded). RiCo activities were in LA/TE− median, 131%, range, 41–354%, and in LA/TE+ median, 143%, range, 53–319%; p = 0.174. There was no difference of the CEPI-CT anymore discernible between the two LA groups after exclusions for low platelet counts and low RiCo (p = 0.21). In contrast to our expectations, CEPI-CT in LA/TE− (−5)TT individuals did not differ from (−5)TC in this group (Table 2, p = 0.42), which is in contrast to healthy controls. The CEPI-CT from patients with arterial disease was also not different from other LA/TE− individuals (Table 3, p = 0.8). Findings were not changed after exclusion of individuals with a CADP-CT > 170 s, which is the upper limit in healthy controls (data not shown).
Platelet antibodies directed against GPIb/IX were detectable in six patients in each patients’ group, and the CEPI-CT was prolonged in four patients from each group (p > 0.05).
Discussion
LA is regarded as a surrogate marker for the risk of TE, which may ensue once its path is paved by a variety of adverse factors coming together. Some of these could be inherited polymorphisms that shift the coagulation cascade towards thrombosis. Thus, platelet GP polymorphisms have been associated with TE [13, 14]. In this report, we show that the (−5)C allel of the Kozak sequence of GPIbα may contribute to the risk for TE in individuals with LA.
Platelets may have distinct roles in the pathomechanism of TE in individuals with LA. First, they may contribute to the generation of LA as a result of the exposure of negatively charged phospholipids, which together with plasma proteins induce LA formation. Alternatively, already activated platelets [7] may have an increased affinity to bind LA. Thus, platelets’ conformation, either in the resting state or activated, may play a significant role in the progress of coagulation, eventually leading to thrombosis. The conformational change of GPIb allows exposure of the binding site for the vWF, binding of thrombin, FXI and FXII, P-selectin and MAC-1 or αMβ2. It was therefore tempted to speculate that GPIbα genes are associated with an increased risk for thrombosis [13, 14].
We observed no deviation of the VNTR gene frequencies of GPIbα in this cohort of LA individuals compared to healthy controls. Our data, however, disclose a predominance of the (−5)C allele of the Kozak sequence in the LA/TE+ population. It has been proposed that this allele is associated with a higher density of the GPIbα than the (−5)T allele [16]. These findings lead to the hypothesis that individuals with the (−5)C allele have platelets of increased function disposing towards an increased risk for coronary disease or stroke [13, 14].
Assuming that platelets in LA/TE− individuals do not differ from healthy individuals, we expected in LA/TE− individuals, like in healthy controls, shorter CEPICT in (−5)TT than in (−5)TC. In LA/TE+ patients, we expected shortened closure times, irrespective the Kozak genotype, indicating increased platelet function. Applying high shear stress rates by the PFA-100, we could not disclose in any of the two LA patients’ groups an increased platelet function, however. Rather, we observed prolonged closure times in individuals from both groups, which were not explained by low vWFAg or RiCo levels. It may be that other factors influence the in vitro response of platelets to high shear stress rates in LA. Platelet autoantibodies, which are common in individuals with LA [26–31], are key candidates to affect platelet function in LA; too few patients had antibodies to GPIb/IX to detect an association between these antibodies and the CEPI-CT, however. Other, so far unknown influences may also play a role in LA individuals’ platelet function, as estimated by the PFA-100. Likewise, Harrison et al. [25] noted prolonged rather than shortened closure times by the PFA-100 in some individuals with the APS.
In a recent report in patients with APS, Levy et al. [32] have noticed an increased platelet deposition on extracellular matrix as determined by the Cone and Plate(let) analyzer in a subgroup of patients with a history of TE. These strong platelet responses were attributed to increased levels of vWFAg in their patients. Likewise, vWFAg levels were high in many individuals from both LA groups in our report, and this elevation was more pronounced in the LA/TE+ group. In accordance with our data on FVIIIAg levels in this patient population [33], a clear differentiation between LA/TE+ from LA/TE− was not possible. As CEPI-CT and CADP-CT were prolonged in some LA individuals from both groups, the PFA-100 may be sensitive to a different malfunction of platelets in LA individuals than the Cone and Plate(let) analyzer or even aggregometry [32].
Our results need cautious interpretation. First, the number of LA individuals in our patient cohorts may be too small to disclose a small or moderate association of the VNTR and the development of LA and/or thrombosis. In particular, larger patient numbers are needed to confirm the association of the (−5)C allele of the Kozak sequence with the risk for TE disease and more rapid plug formation in LA patients, as determined by the PFA-100. Of note, we had to exclude some individuals from both patients’ populations from further evaluations because of variables that prolong the CEPI-CT, like low platelet counts or low RiCo, and therefore may have missed the correlation between a shortened CT and the polymorphism within the Kozak region. Second, the group of individuals with LA who never developed TE is rather small. However, it is difficult to find individuals with a documented persistence of LA without thrombosis. Third, differences between sex and age of the patients and controls may affect our data. The majority of patients was female and of younger age in the LA/TE+ group than in the LA/TE− group. Thus, an estrogen effect may dispose these individuals for TE disease. We hypothesize, however, that LA most often develops already in young individuals, but only pathogenetic significant LA is associated with thrombosis. “Benign” LA that has also been formed in young age is then discovered by chance in elderly subjects who are undergoing medical examination. This hypothesis needs to be evaluated in prospective studies. Fourth, although the observation time was similar in both patients’ groups, we cannot exclude a future thrombotic event in an individual from the LA/TE− group. Longer observation times may be required to address this question. However, only one patient from the LA/TE− patients received oral anticoagulation, which may have prevented future thrombosis. Last, thromboembolism in LA is a possibly fatal disorder, and studying survivors may bias the results, because those who succumb to the disease are lost for evaluation.
In summary, our data suggest an association of the (−5)C allele of the Kozak sequence in LA patients with the risk for TE. However, this genetic disposition may require additional signals for disposing at risk for thromboembolism. The affected platelet function in individuals with LA, as estimated by the PFA-100, is not associated with a particular Kozak genotype or a history of TE, however. These data need confirmation in larger, preferentially multicenter, prospective studies.
References
Love PE, Santoro SA (1990) Antiphospholipid antibodies: anticardiolipin and the lupus anticoagulant in systemic lupus erythematosus (SLE) and in non-SLE disorders. Prevalence and clinical significance. Ann Intern Med 112:682–698
Levine JS, Branch DW, Rauch J (2002) The antiphospholipid syndrome. N Engl J Med 346:752–763
Zoghlami-Rintelen C, Vormittag R, Sailer T, Lehr S, Quehenberger P, Rumpold H, Male C, Pabinger I (2005) The presence of IgG antibodies against beta2-glycoprotein I predicts the risk of thrombosis in patients with the lupus anticoagulant. J Thromb Haemost 3:1160–1165
Campbell AL, Pierangeli SS, Wellhausen S, Harris EN (1995) Comparison of the effects of anticardiolipin antibodies from patients with the antiphospholipid syndrome and with syphilis on platelet activation and aggregation. Thromb Haemost 73:529–534
Escolar G, Font J, Reverter JC, Lopez-Soto A, Garrido M, Cervera R, Ingelmo M, Castillo R, Ordinas A (1992) Plasma from systemic lupus erythematosus patients with antiphospholipid antibodies promotes platelet aggregation. Studies in a perfusion system. Arterioscler Thromb 12:196–200
Galli M, Bevers EM, Comfurius P, Barbui T, Zwaal RF (1993) Effect of antiphospholipid antibodies on procoagulant activity of activated platelets and platelet-derived microvesicles. Br J Haematol 83:466–472
Joseph JE, Harrison P, Mackie IJ, Isenberg DA, Machin SJ (2001) Increased circulating platelet-leucocyte complexes and platelet activation in patients with antiphospholipid syndrome, systemic lupus erythematosus and rheumatoid arthritis. Br J Haematol 115:451–459
Machin SJ (1996) Platelets and antiphospholipid antibodies. Lupus 5:386–387
Martinuzzo ME, Maclouf J, Carreras LO, Levy-Toledano S (1993) Antiphospholipid antibodies enhance thrombin-induced platelet activation and thromboxane formation. Thromb Haemost 70:667–671
Slupsky JR, Cawley JC, Griffith LS, Shaw AR, Zuzel M (1992) Role of Fc gamma RII in platelet activation by monoclonal antibodies. J Immunol 148:3189–3194
Wang L, Su CY, Chou KY, Wang CT (2002) Enhancement of human platelet activation by the combination of low concentrations of collagen and rabbit anticardiolipin antibodies. Br J Haematol 118:1152–1162
Arvieux J, Roussel B, Pouzol P, Colomb MG (1993) Platelet activating properties of murine monoclonal antibodies to beta 2-glycoprotein I. Thromb Haemost 70:336–341
Deckmyn H, Ulrichts H, Van De Walle G, Vanhoorelbeke K (2004) Platelet antigens and their function. Vox Sang 87(Suppl 2):105–111
Yee DL, Bray PF (2004) Clinical and functional consequences of platelet membrane glycoprotein polymorphisms. Semin Thromb Hemost 30:591–600
Lopez JA, Ludwig EH, McCarthy BJ (1992) Polymorphism of human glycoprotein Ib alpha results from a variable number of tandem repeats of a 13-amino acid sequence in the mucin-like macroglycopeptide region. Structure/function implications. J Biol Chem 267:10055–10061
Afshar-Kharghan V, Li CQ, Khoshnevis-Asl M, Lopez JA (1999) Kozak sequence polymorphism of the glycoprotein (GP) Ibalpha gene is a major determinant of the plasma membrane levels of the platelet GP Ib-IX-V complex. Blood 94:186–191
Jilma-Stohlawetz P, Homoncik M, Jilma B, Knechtelsdorfer M, Unger P, Mannhalter C, Santoso S, Panzer S (2003) Glycoprotein Ib polymorphisms influence platelet plug formation under high shear rates. Br J Haematol 120:652–655
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Brandt JT, Triplett DA, Alving B, Scharrer I (1995) Criteria for the diagnosis of lupus anticoagulants: an update. On behalf of the Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the ISTH. Thromb Haemost 74:1185–1190
Schallmoser K, Rosin C, Knittelfelder R, Sailer T, Ulrich S, Zoghlami C, Lehr S, Pabinger I, Panzer S (2005) The Fc gammaRIIa polymorphism R/H131, autoantibodies against the platelet receptors GPIb alpha and Fc gammaRIIa and a risk for thromboembolism in lupus anticoagulant patients. Thromb Haemost 93:544–548
Jilma B (2001) Platelet function analyzer (PFA-100): a tool to quantify congenital or acquired platelet dysfunction. J Lab Clin Med 138:152–163
Homoncik M, Jilma B, Hergovich N, Stohlawetz P, Panzer S, Speiser W (2000) Monitoring of aspirin (ASA) pharmacodynamics with the platelet function analyzer PFA-100. Thromb Haemost 83:316–321
Reiter RA, Mayr F, Blazicek H, Galehr E, Jilma-Stohlawetz P, Domanovits H, Jilma B (2003) Desmopressin antagonizes the in vitro platelet dysfunction induced by GPIIb/IIIa inhibitors and aspirin. Blood 102:4594–4599
Schallmoser K, Rosin C, Vormittag R, Brunner M, Dunkler D, Pabinger I, Panzer S (2006) Specificities of platelet autoantibodies and platelet activation in lupus anticoagulant patients: a relation to their history of thromboembolic disease. Lupus 15:507–514
Harrison P, Robinson MS, Mackie IJ, Joseph J, McDonald SJ, Liesner R, Savidge GF, Pasi J, Machin SJ (1999) Performance of the platelet function analyser PFA-100 in testing abnormalities of primary haemostasis. Blood Coagul Fibrinolysis 10:25–31
Out HJ, de Groot PG, van Vliet M, de Gast GC, Nieuwenhuis HK, Derksen RH (1991) Antibodies to platelets in patients with anti-phospholipid antibodies. Blood 77:2655–2659
Panzer S, Gschwandtner ME, Hutter D, Spitzauer S, Pabinger I (1997) Specificities of platelet autoantibodies in patients with lupus anticoagulants in primary antiphospholipid syndrome. Ann Hematol 74:239–242
Rock G, Chauhan K, Jamieson GA, Tandon NN (1994) Anti-CD36 antibodies in patients with lupus anticoagulant and thrombotic complications. Br J Haematol 88:878–880
Macchi L, Rispal P, Clofent-Sanchez G, Pellegrin JL, Nurden P, Leng B, Nurden AT (1997) Anti-platelet antibodies in patients with systemic lupus erythematosus and the primary antiphospholipid antibody syndrome: their relationship with the observed thrombocytopenia. Br J Haematol 98:336–341
Godeau B, Piette JC, Fromont P, Intrator L, Schaeffer A, Bierling P (1997) Specific antiplatelet glycoprotein autoantibodies are associated with the thrombocytopenia of primary antiphospholipid syndrome. Br J Haematol 98:873–879
Galli M, Daldossi M, Barbui T (1994) Anti-glycoprotein Ib/IX and IIb/IIIa antibodies in patients with antiphospholipid antibodies. Thromb Haemost 71:571–575
Levy Y, Shenkman B, Tamarin I, Pauzner R, Shoenfeld Y, Langevitz P, Savion N, Varon D (2005) Increased platelet deposition on extracellular matrix under flow conditions in patients with antiphospholipid syndrome who experience thrombotic events. Arthritis Rheum 52:4011–4017
Sailer T, Vormittag R, Pabinger I, Vukovich T, Lehr S, Quehenberger P, Panzer S, Lechner K, Zoghlami-Rintelen C (2005) Inflammation in patients with lupus anticoagulant and implications for thrombosis. J Rheumatol 32:462–468
Acknowledgment
The authors thank Silvia Koder for patients’ care and administration, Eva Guschlbauer and Peter Quehenberger for the determinations of von Willebrand Factor Antigen and Ristocetin Cofactor activity, and Beate Eichelberger and Daniela Koren for expert technical assistance.
This work was supported in part by a Grant from the Hochschuljubiläumsstiftung der Stadt Wien and by Grant 8647 from the Österreichischen Nationalbank to Simon Panzer, and by Grant 2027 of the Medizinisch-Wissenschaftlichen Fonds des Bürgermeisters der Bundeshauptstadt Wien to Ingrid Pabinger.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jilma-Stohlawetz, P., Jilma, B., Mannhalter, C. et al. Platelet glycoprotein Ibα polymorphisms and function evaluated by the platelet function analyzer PFA-100 in patients with lupus anticoagulant: the association with thromboembolic disease. Ann Hematol 86, 719–725 (2007). https://doi.org/10.1007/s00277-007-0341-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-007-0341-3