Abstract
Posttransplant lymphoproliferative disease (PTLD) is closely linked to primary Epstein–Barr virus (EBV) infection. A defect of EBV specific cellular immunity is postulated to play a pivotal role in the etiology of PTLD, but there is some debate as to whether EBV load in the peripheral blood of transplant patients predicts onset of PTLD or relapse after treatment. The current prospective, single-center study was undertaken to investigate the impact of therapy on EBV load in adult patients with PTLD. Fifteen patients with PTLD after solid organ transplantation were included and of these, seven had EBV-associated PTLD. All 15 patients received Rituximab as primary therapy. In cases of treatment failure or relapse after Rituximab treatment, patients received polychemotherapy according to the cyclophosphamide, vincristine, doxorubicin, and prednisone regimen. At onset of PTLD, the median EBV load in the peripheral blood of patients was higher in EBV-associated PTLD than PTLD with no associated EBV infection. After Rituximab therapy, four of seven patients with EBV-associated PTLD achieved long-lasting complete remissions. However, in two of these patients, EBV load increased to reach levels as high as those recorded at onset of PTLD. Another patient showed a dramatic decline of EBV load after the first dose of Rituximab while suffering from progressive disease. The other patient relapsed after Rituximab monotherapy, but his viral load stayed low. In total, discordance in EBV load and clinical course was observed in five of the seven patients with EBV-associated PTLD. We conclude that in adult patients with PTLD, EBV load does not correlate with treatment response and is not suitable as a predictive marker for PTLD relapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttransplant lymphoproliferative disease (PTLD) is the most common neoplastic disease after solid organ transplantation [14]. The Epstein–Barr virus (EBV), a ubiquitous lympho- and epitheliotropic γ1-herpesvirus, is detectable in lesions of PTLD in up to 60–90% of cases and is believed to be one of the major factors involved in the pathogenesis of PTLD [28]. About 10 years ago, EBV viral load in peripheral blood was established as a diagnostic tool in PTLD. However, EBV viral load monitoring after therapy is still controversial and differences may exist in pediatric and adult patients. Several groups reported increased EBV load in peripheral blood mononuclear cells (PBMC), whole blood or serum in patients at the time of PTLD onset [4, 5, 8, 9, 13, 16–18, 20, 22, 25–27], and some groups also described a correlation in decreased viral load and effective PTLD treatment [5, 8, 16, 18]. However, Yang et al. [27] described a marked divergence in clearance of EBV load and clinical response after Rituximab treatment and suggested that reduced EBV DNA after Rituximab therapy is a consequence of B-cell clearance. This lack of relationship between change in viral load and clinical response highlights the difference between EBV-infected PBMCs and neoplastic cells in PTLD. Along with other parameters, however, viral load monitoring is still widely used in patients with PTLD for follow-up and to assess the effectiveness of therapeutic protocols. Most prior studies have been performed in pediatric patients, with only the study of Yang et al. [27] included adult patients, and therefore neither the frequency or duration of monitoring nor the predictive value of EBV viral load monitoring after solid organ transplantation (SOT) has been clearly established in adults. To establish the parameters of EBV monitoring for adult PTLD patients, we investigated the impact of therapy on EBV viral load in 15 adult patients with PTLD. Monitoring, using a quantitative real-time polymerase chain reaction (PCR) technique, commenced at disease onset, with a median follow-up of 23 months.
Materials and methods
Patients
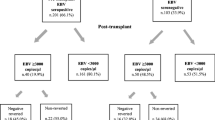
This prospective single-center study aimed to investigate the impact of therapy on EBV load in the peripheral blood of adult patients presenting with PTLD was commenced in January 2000. All patients gave their written informed consent and were seen at the university hospital Charite-Campus Virchow Clinic, Berlin, Germany. Two patients (patients 6 and 7) were EBV-seronegative before transplantation and received a renal transplant from an EBV-positive donor, and all remaining patients were EBV-seropositive before transplantation.
Histopathology
PTLD diagnosis was based on an examination of histological material obtained by open biopsy or by core needle biopsy, and lesions were classified according to the World Health Organization (WHO) Classification of Tumors [6]. An association with EBV was confirmed by immunohistochemical staining of the latent membrane protein-1 or by Epstein–Barr nuclear antigen 2, or by in situ hybridization of EBV encoded RNA (EBER) transcripts. Immunohistochemical staining of LMP1 was performed on all lesions, while staining of EBNA2 and in situ staining for EBER was performed at the reference laboratory of Professor Harald Stein (Department for Pathology, Free University Berlin, Germany) in biopsies from 11 patients.
Staging
Patient evaluation included a complete patient history, physical examination, bone marrow biopsy, and computed tomography scans of the chest, abdomen, and pelvis. Peripheral blood analyses included a complete blood count, while biochemical analyses included lactate dehydrogenase concentration (upper limit 240 U/l) and routine tests of hepatic and renal function. Further studies were performed as clinically indicated.
Treatment
Immunosuppressive therapy was withdrawn in all patients before their entry into the study protocol, but failed to confer a significant benefit in all cases. Rituximab, a monoclonal antibody against CD20 antigen, has proven its effectiveness in treatment of PTLD [2, 12] and, accordingly, all seven patients with EBV-associated PTLD were treated with Rituximab. All patients were commenced on Rituximab 375 mg/m2 by intravenous infusion on days 1, 8, 15, and 22. Those patients with relapsed or refractory PTLD after Rituximab received polychemotherapy comprising the CHOP (cyclophosphamide, vincristine, doxorubicin, and prednisone) regimen. Carboplatin (CBCDA) plus VP-16 (etoposide) or bortezomib were third- and fourth-line regimens, respectively. In a patient with lymphocyte-predominant, advanced Hodgkin PTLD, ABVD (doxorubicin, bleomycin, vinblastin, and dacarbazin) was used instead of CHOP.
EBV load measurement
Peripheral blood samples were taken at diagnosis and at weekly intervals for the first 4 weeks. In patients receiving polychemotherapy, blood tests were performed on a biweekly basis. Blood samples were collected at 4–12 week intervals thereafter, depending on the clinical course.
DNA was extracted from 200 μl whole blood by QIAmp DNA Minikit (Qiagen, Hilden, Germany) and eluted in a final volume of 100 μl. As EBV is mainly latent and not lytic during cell proliferation, it is therefore integrated in cells. For this reason, samples including the cellular fraction are more appropriate than cell-free material for measurement of EBV load in PTLD; as opposed to PCR from PBMCs, PCR from whole blood determines EBV copies both from infectious virions during primary infection (which is very unlikely in the setting of the study) or from EBV-positive memory cells. There are only a few studies in which whole blood, PBMCs, and cell-free material have been compared. In a study by Wadowsky et al. [23], however, comparison of EBV evaluation in whole blood and isolated lymphocytes demonstrated a superior correlation compared with that observed between lymphocytes and plasma.
EBV PCR was performed as hot-start real-time PCR (LightCycler, Roche Diagnostics, Mannheim, Germany) on the viral capsid (VCA) gene for p23. Briefly, extracted DNA (8 μl) was amplified in a final volume of 20 μl reaction mix containing 2 μl master mix (LightCycler DNA Mater Hybridization Probes, Roche Diagnostics, Mannheim, Germany) supplemented with 0.32 μl of a Taq antibody (Taq Start Antibody, Clontech, Palo Alto, CA, USA), 6 mM MgCl2, and 0.5 μM of the EBV primers 5′-TGG CGT TGG GGT CGT TTG AT-3′ (89332-351 in B95-8) and 5′-CGV CTG GCT CGC CTG GAG T-3′ (88997-89015) and 0.15 μM of the probes 5′-GCG GAG GCA CTG GAG CAG AAG GAA CAFl-3′ (89077-102) and 5′-Red640AGG TAG ACG AGG CAC AGG CAC CCC CT-3′ (89050-075). Cycling conditions included an initial step at 95°C for 75 s, followed by 45 cycles at 95°C for 1 s, at 60°C for 10 s, and at 72°C for 18 s. Melting point analysis (between 40 and 75°C) was applied after amplification to enhance specificity. Each run contained multiple negative controls and standards for quantitation using the plasmid pGem3Z30 including the gene sequence of p23 in EBV-negative DNA. Inhibition control was performed by a second PCR in which positive control was added to each sample [7]. Specificity was proven because DNAs from all other seven human herpesviruses were negative. Sensitivity was determined using both plasmid and cellular dilution series. Plasmid containing EBV genome was quantified by optical density, and tenfold dilutions corresponding to two, 20, or 200 copies/PCR run (in 8 μl template) were tested. In addition, a dilution series of Namalwa cells (approximately two copies/cell) of one, ten, and 100 Namalwa cells/PCR run (in 8 μl template) was also tested. The plasmid and Namalwa cell dilution series were also tested after 20-fold dilution. In the plasmid dilution series, positive results were observed in 7/20, 19/20, and 20/20 PCR runs in the two, 20, and 200 copy dilutions, respectively. In the Namalwa cell dilution series, positive results were observed in 5/20, 20/20, and 20/20 PCR runs in the one, ten, and 100 cell dilutions (equal to two, 20, and 200 copies), respectively. Thus, the 95% detection limit is slightly lower than 20 copies/PCR run, which translates to a detection limit of 1,250 copies/ml whole blood. However, due to Poisson distribution, some samples tested positive although the viral load was <1,250 copies/ml. A total of 120 healthy individuals tested negative using this PCR method. The linear range for detection is therefore between 1,250 and 108 copies/ml.
Results
Patient and disease characteristics
A total of 15 patients with PTLD were enrolled in this study. Patient ages ranged from 18 to 67 years, with a median age of 51 years. Three patients were recipients of a heart transplant, nine had received a kidney transplant, and the remaining three patients were liver transplant recipients. Histological evaluation demonstrated polymorphic PTLD in one patient and monomorphic PTLDs in 14 patients [DLBCL, nine; mantle cell lymphoma (MCL), two; follicular lymphoma, one; atypical Burkitt lymphoma, one; and lymphocyte-predominant Hodgkin-type lymphoma, one]. Approximately, two-thirds of the patients had stage III or stage IV disease. More details on clinical characteristics, EBV-association, and response to therapy are given in Table 1.
EBV load at diagnosis
The EBV load at PTLD diagnosis is shown in Fig. 1 and Table 1. In the seven patients with EBV-positive PTLD, EBV was not detectable in the peripheral blood of three and in the remaining four patients; viral load ranged from 1,250 to 2,650,000 copies/ml. In contrast, in three of eight patients with non-EBV-associated PTLD, EBV DNA was present in whole blood at levels of 2,000–6,100 EBV copies/ml. All other non-EBV-associated PTLD patients did not show detectable levels of EBV genome.
EBV viral load at diagnosis of PTLD. PTLD diagnosis was based on an examination of histological material. An association with EBV was confirmed by immunohistological staining as described in “Materials and methods”. EBV PCR was performed as hot-start real-time PCR on the viral capsid (VCA) gene for p23, and melting point analysis was applied after amplification to enhance specificity. For details concerning negative controls, standards for quantitation, inhibition control, and specificity, see “Materials and methods”. A 95% detection rate of at least 20 copies/PCR run was determined corresponding to a detection limit of 1,250 copies/ml whole blood (dotted line). The linear range is between the detection limit and 108 copies/ml. Of seven patients with EBV-positive PTLD, EBV was not detectable in the peripheral blood of three patients and in the remaining four patients; viral load ranged from 1,250 copies/ml to 2,650,000 copies/ml. Median viral load was 1,250 copies/ml (horizontal black line). In contrast, in three of eight patients with non-EBV-associated PTLD, EBV DNA was present in whole blood at a level of 2,000–6,100 EBV copies/ml. All other non-EBV-associated PTLD patients did not show detectable levels of EBV genome. Median viral load for non-EBV-associated PTLD was 0 copies/ml (horizontal black line)
EBV load after Rituximab therapy in patients with EBV-associated PTLD
After Rituximab monotherapy, four of the seven patients achieved complete remissions of long duration (1,098, 1,279, 1,403, and 1,630 days, respectively). In patient 2, the first dose of Rituximab was associated with a dramatic decline in EBV load (from 2,650,000 copies/ml before Rituximab to 100 copies/ml DNA 1 week later; Fig. 2b), which was paralleled by a dramatic reduction of the patient’s tumor mass. Moreover, using FACS analysis, we could show that this rapid disappearance of virus-infected cells was paralleled by the disappearance of circulating B-cells [10]. Reconstitution of CD20-positive cells in peripheral blood was associated with an increase in EBV-load starting 12 months after Rituximab treatment and reaching levels as high as those observed before treatment. With a follow-up time of more than 2 years, this increment in EBV load was not associated with a relapse of PTLD. Similar findings were observed in patient 4 (data not shown); 12 months after Rituximab treatment, the EBV load increased to 850,000 copies/ml with no evidence of PTLD relapse.
EBV load after Rituximab therapy in patients with EBV-associated PTLD. Blood samples were collected at diagnosis and at weekly intervals for the first 4 weeks and at 4–12 week intervals thereafter, depending on the clinical course. EBV PCR was performed as hot-start real-time PCR on the VCA gene for p23, and melting point analysis was applied after amplification to enhance specificity. For details concerning negative controls, standards for quantitation, inhibition control, and specificity, see “Materials and methods”. A 95% detection rate of at least 20 copies/PCR run was found. This translates to a detection limit of 1,250 copies/ml whole blood (dotted line). The linear range is between the detection limit and 108 copies/ml. a Patient 1 demonstrates the situation of monitoring EBV load in EBV-associated PTLD without ever measuring elevated EBV load in a period of more than 3 years. The patient had a polymorphic PTLD and achieved a stable complete remission (CR) after Rituximab. b This patient also achieved a long-lasting CR after Rituximab monotherapy. After the first dose of Rituximab, a dramatic decline in EBV load was observed, which was paralleled by a dramatic reduction of the patient’s tumor mass. Twelve months after Rituximab treatment, the EBV load increased to reach pre-Rituximab levels. This increment in EBV load was not associated with a relapse of PTLD. c Patient 3 demonstrated a PTLD relapse not associated with an increase in EBV load, although EBV load was positive earlier and later on. d This patient neither responded to initial antiviral treatment with foscarnet nor to Rituximab. While EBV load increased from 200,000 to 350,000 copies/ml during antiviral therapy, a dramatic decline followed the first application of Rituximab. The patient died due to PTLD progression, although his EBV load remained negative
In patient 6, the reverse situation was observed (Fig. 2d). The patient failed to respond clinically to initial antiviral treatment with foscarnet nor to Rituximab. However, while EBV load increased from 200,000 to 350,000 copies/ml during antiviral therapy, a dramatic decline was achieved after the first application of Rituximab. However, the PTLD did not respond to chemotherapy and the patient died due to PTLD progression, although his EBV load remained negative during the remainder of his clinical course.
Patient 1 responded to Rituximab treatment and is in ongoing complete remission. EBV load was monitored for a period extending beyond 3 years in this patient and remained negative during this time (Fig. 2a). Finally, patient 3 demonstrated a PTLD relapse not associated with an increase in EBV load (Fig. 2c), although EBV load was positive earlier and later on.
Discussion
These data demonstrate that after Rituximab therapy in adult PTLD, EBV load parallels the disappearance and reconstitution of CD20 B-cells in peripheral blood; these are therefore in accordance with the data of Yang et al. [27]. We have demonstrated that an increase of EBV load to PTLD pretreatment values is not necessarily accompanied by relapse of PTLD (patients 1 and 4), and the recovery of EBV viral load is coincident with B-cell recovery after treatment of PTLD with Rituximab (patients 2 and 4) [19]. Earlier studies have already suggested that circulating EBV-positive cells represent memory B-cells and not proliferating lymphoblasts, and are similar to latently infected resting B-memory cells from EBV-positive normal individuals in terms of EBV-gene expression and number of EBV-genomes per cells [1, 27]. Due to an impaired EBV-specific cytotoxic T-lymphocyte (CTL) response, an increased peripheral EBV load may therefore represent a surrogate marker for EBV infection under immunosuppression, with latently infected and expanding blasts remaining in the lymph nodes, similar to their normal counterparts. This may explain why an increase in peripheral EBV load may have some predictive significance for early diagnosis [4, 5, 8, 9, 13, 16–18, 20, 22, 25–27] but limited predictive significance for relapse after Rituximab treatment.
Monitoring of EBV DNA levels after transplantation was considered to guide preemptive treatment of patients before overt EBV PTLD appeared and for the prediction of early PTLD after hematopoetic stem-cell transplantation. In these settings, the detection of two or more levels of EBV DNA above 4,000 copies/μg was reported to have a sensitivity of 100% (specificity 50%) [24]. As the predictive power of detecting EBV DNA levels higher than 4,000 copies/μg on more than two occasions was only 50% in this series, preemptive therapy would have exposed half the recipients to unnecessary therapy. Such therapy could be associated with significant deleterious effects, particularly in patients with PTLD after SOT. In the series presented in this study, an elevated pretherapeutic EBV load was detected in only three of the seven patients with EBV-associated PTLD. This finding indicates that further relevant factors play a role in the pathogenesis of PTLD after SOT, i.e., molecular alterations, such as rearranged oncogenes [3] or accumulated tumor suppressor mutations allowing EBV-independent growth characteristics [15]. These data do not, therefore, support the use of EBV DNA level monitoring to guide preemptive immunotherapy or chemotherapy. However, serial quantitative analysis of the EBV genome load may be useful for preventing PTLD through adjustment of immunosuppression in response to viral genome load after symptomatic EBV infection [11], and in discriminating PTLD from rejection [21].
In summary, by applying EBV real-time quantitative PCR techniques in a significant number of adult PTLD patients, we have confirmed that the individual EBV load in adult PTLD patients during long-term follow-up does not correlate with treatment response and therefore is not suitable as a predictive marker for effective therapy or PTLD relapse in adult patients. In five out of seven patients with EBV-associated PTLD, we were able to demonstrate a significant incongruity of EBV load and clinical course. Moreover, all clinically relevant situations were covered by these patients, i.e., (1) the reappearance of EBV replication without PTLD relapse, (2) a relapse without prior increase in EBV load, (3) progressive disease associated with clearance of EBV DNA in peripheral blood samples, and (4) absence of elevated EBV load. This study significantly contributes to the question on the impact of EBV load in peripheral blood for monitoring adult PTLD patients by presenting data of several novel patients with an extensive long-term follow-up with a remarkable divergence of EBV load and clinical course.
References
Babcock GJ, Decker LL, Freeman RB, Thorley-Lawson DA (1999) Epstein–Barr virus-infected resting memory B cells, not proliferating lymphoblasts, accumulate in the peripheral blood of immunosuppressed patients. J Exp Med 190:567–576
Choquet S, Leblond V, Herbrecht R, Socie G, Stoppa AM, Vandenberghe P, Fischer A, Morschhauser F, Salles G, Feremans W, Vilmer E, Peraldi MN, Lang P, Lebranchu Y, Oksenhendler E, Garnier JL, Lamy T, Jaccard A, Ferrant A, Offner F, Hermine O, Moreau A, Fafi-Kremer S, Morand P, Chatenoud L, Berriot-Varoqueaux N, Bergougnoux L, Milpied N (2005) Efficacy and safety of Rituximab in B-cell posttransplant lymphoproliferative disorders: results of a prospective multicentre phase II study. Blood: (Epub ahead of print)
Dotti G, Fiocchi R, Motta T, Gamba A, Gotti E, Gridelli B, Borleri G, Manzoni C, Viero P, Remuzzi G, Barbui T, Rambaldi A (2000) Epstein–Barr virus-negative lymphoproliferate disorders in long-term survivors after heart, kidney, and liver transplant. Transplantation 69:827–833
Fellner MD, Durand K, Correa M, Bes D, Alonio LV, Teyssie AR, Picconi MA (2003) A semiquantitative PCR method (SQ-PCR) to measure Epstein–Barr virus (EBV) load: its application in transplant patients. J Clin Virol 28:323–330
Green M, Cacciarelli TV, Mazariegos GV, Sigurdsson L, Qu L, Rowe DT, Reyes J (1998) Serial measurement of Epstein–Barr viral load in peripheral blood in pediatric liver transplant recipients during treatment for posttransplant lymphoproliferative disease. Transplantation 66:1641–1644
Harris NL, Ferry JA, Swerdlow SH (1997) Posttransplant lymphoproliferative disorders: summary of Society for Hematopathology Workshop. Semin Diagn Pathol 14:8–14
Ibrahim AI, Obeid MT, Jouma MJ, Moasis GA, Al-Richane WL, Kindermann I, Boehm M, Roemer K, Mueller-Lantzsch N, Gartner BC (2005) Detection of herpes simplex virus, cytomegalovirus and Epstein–Barr virus DNA in atherosclerotic plaques and in unaffected bypass grafts. J Clin Virol 32:29–32
Kenagy DN, Schlesinger Y, Weck K, Ritter JH, Gaudreault-Keener MM, Storch GA (1995) Epstein–Barr virus DNA in peripheral blood leukocytes of patients with posttransplant lymphoproliferative disease. Transplantation 60:547–554
Kogan DL, Burroughs M, Emre S, Fishbein T, Moscona A, Ramson C, Shneider BL (1999) Prospective longitudinal analysis of quantitative Epstein–Barr virus polymerase chain reaction in pediatric liver transplant recipients. Transplantation 67:1068–1070
Maloney DG, Liles TM, Czerwinski DK, Waldichuk C, Rosenberg J, Grillo-Lopez A, Levy R (1994) Phase I clinical trial using escalating single-dose infusion of chimeric anti-CD20 monoclonal antibody (IDEC-C2B8) in patients with recurrent B-cell lymphoma. Blood 84:2457–2466
Matsukura T, Yokoi A, Egawa H, Kudo T, Kawashima M, Hirata Y, Tanaka H, Kagajo K, Wada H, Tanaka K (2002) Significance of serial real-time PCR monitoring of EBV genome load in living donor liver transplantation. Clin Transplant 16:107–112
Oertel SH, Verschuuren E, Reinke P, Zeidler K, Papp-Vary M, Babel N, Trappe RU, Jonas S, Hummel M, Anagnostopoulos I, Dorken B, Riess HB (2005) Effect of anti-CD 20 antibody rituximab in patients with post-transplant lymphoproliferative disorder (PTLD). Am J Transplant 5:2901–2906
Orentas RJ, Schauer DW Jr, Ellis FW, Walczak J, Casper JT, Margolis DA (2003) Monitoring and modulation of Epstein–Barr virus loads in pediatric transplant patients. Pediatr Transplant 7:305–314
Penn I, Hammond W, Brettschneider L, Starzl TE (1969) Malignant lymphomas in transplantation patients. Transplant Proc 1:106–112
Poirel HA, Bernheim A, Schneider A, Meddeb M, Choquet S, Leblond V, Charlotte F, Davi F, Canioni D, Macintyre E, Mamzer-Bruneel MF, Hirsch I, Hermine O, Martin A, Cornillet-Lefebvre P, Patey M, Toupance O, Kemeny JL, Deteix P, Raphael M (2005) Characteristic pattern of chromosomal imbalances in posttransplantation lymphoproliferative disorders: correlation with histopathological subcategories and EBV status. Transplantation 80:176–184
Riddler SA, Breinig MC, McKnight JL (1994) Increased levels of circulating Epstein–Barr virus (EBV)-infected lymphocytes and decreased EBV nuclear antigen antibody responses are associated with the development of posttransplant lymphoproliferative disease in solid-organ transplant recipients. Blood 84:972–984
Rowe DT, Qu L, Reyes J, Jabbour N, Yunis E, Putnam P, Todo S, Green M (1997) Use of quantitative competitive PCR to measure Epstein–Barr virus genome load in the peripheral blood of pediatric transplant patients with lymphoproliferative disorders. J Clin Microbiol 35:1612–1615
Rowe DT, Webber S, Schauer EM, Reyes J, Green M (2001) Epstein–Barr virus load monitoring: its role in the prevention and management of post-transplant lymphoproliferative disease. Transpl Infect Dis 3:79–87
Savoldo B, Rooney CM, Quiros-Tejeira RE, Caldwell Y, Wagner HJ, Lee T, Finegold MJ, Dotti G, Heslop HE, Goss JA (2005) Cellular immunity to Epstein–Barr virus in liver transplant recipients treated with Rituximab for post-transplant lymphoproliferative disease. Am J Transplant 5:566–572
Scheenstra R, Verschuuren EA, de Haan A, Slooff MJ, The TH, Bijleveld CM, Verkade HJ (2004) The value of prospective monitoring of Epstein–Barr virus DNA in blood samples of pediatric liver transplant recipients. Transpl Infect Dis 6:15–22
Stevens SJ, Verschuuren EA, Pronk I, van Der Bij W, Harmsen MC, The TH, Meijer CJ, van Den Brule AJ, Middeldorp JM (2001) Frequent monitoring of Epstein–Barr virus DNA load in unfractionated whole blood is essential for early detection of posttransplant lymphoproliferative disease in high-risk patients. Blood 97:1165–1171
Vajro P, Lucariello S, Migliaro F, Sokal E, Gridelli B, Vegnente A, Iorio R, Smets F, Quinto I, Scala G (2000) Predictive value of Epstein–Barr virus genome copy number and BZLF1 expression in blood lymphocytes of transplant recipients at risk for lymphoproliferative disease. J Infect Dis 181:2050–2054
Wadowsky RM, Laus S, Green M, Webber SA, Rowe D (2003) Measurement of Epstein–Barr virus DNA loads in whole blood and plasma by TaqMan PCR and in peripheral blood lymphocytes by competitive PCR. J Clin Microbiol 41:5245–5249
Wagner HJ, Cheng YC, Huls MH, Gee AP, Kuehnle I, Krance RA, Brenner MK, Rooney CM, Heslop HE (2004) Prompt versus preemptive intervention for EBV lymphoproliferative disease. Blood 103:3979–3981
Wagner HJ, Fischer L, Jabs WJ, Holbe M, Pethig K, Bucsky P (2002) Longitudinal analysis of Epstein–Barr viral load in plasma and peripheral blood mononuclear cells of transplanted patients by real-time polymerase chain reaction. Transplantation 74:656–664
Yancoski J, Danielian S, Ibanez J, Turconi A, Cuarterolo M, Zelazko M, Niesters Hubert GM (2004) Quantification of Epstein–Barr virus load in Argentinean transplant recipients using real-time PCR. J Clin Virol 31:58–65
Yang J, Tao Q, Flinn IW, Murray PG, Post LE, Ma H, Piantadosi S, Caligiuri MA, Ambinder RF (2000) Characterization of Epstein–Barr virus-infected B cells in patients with posttransplantation lymphoproliferative disease: disappearance after Rituximab therapy does not predict clinical response. Blood 96:4055–4063
Young L, Alfieri C, Hennessy K, Evans H, O’Hara C, Anderson KC, Ritz J, Shapiro RS, Rickinson A, Kieff E et al (1989) Expression of Epstein–Barr virus transformation-associated genes in tissues of patients with EBV lymphoproliferative disease. N Engl J Med 321:1080–1085
Acknowledgements
Stephan Oertel and Ralf Trappe contributed equally in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oertel, S., Trappe, R.U., Zeidler, K. et al. Epstein–Barr viral load in whole blood of adults with posttransplant lymphoproliferative disorder after solid organ transplantation does not correlate with clinical course. Ann Hematol 85, 478–484 (2006). https://doi.org/10.1007/s00277-006-0109-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-006-0109-1