Abstract
Invasive aspergillosis is an important factor in the morbidity and mortality of patients suffering from hematologic disorders treated with chemotherapy. Treatment with amphotericin B is often limited because of toxicity, particularly nephrotoxicity. We describe a case of invasive pulmonary Aspergillus fumigatus infection in acute myeloid leukemia with renal failure due to amphotericin B therapy, which responded to treatment with a new antifungal agent, micafungin. Micafungin appears to be an effective and safe therapy for Aspergillus infections with renal failure due to amphotericin B.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive aspergillosis is an important factor in the morbidity and mortality of patients suffering from hematologic disorders treated with chemotherapy [1]. For many years, amphotericin B with or without 5-flucytosine has been the drug of choice in the treatment of these cases. Concerns over reports of fungal resistance [2] and toxicity [3, 4] have highlighted the urgent need for alternatives to be found.
Case report
A 64-year-old male patient presented to our institution in January 1999 with clinical signs of hyperleukocytosis and thrombocytopenia. A diagnosis of de novo acute myeloblastic leukemia (AML, normal karyotype, subtype M5a by the French-American-British Classification) was made and induction chemotherapy was begun with cytarabine 60 mg/m2 for 12 days, daunorubicin 20 mg/m2 for 5 days and 6-mercaptopurine 50 mg/m2 with allopurinol 300 mg/body for 12 days. Post-induction therapy bone marrow biopsy was inclusive for complete remission with 0.2% blast. The patient received three courses of consolidation therapy with mitoxantrone 8 mg/m2 and etoposide 80 mg/m2 each for 4 days. After he received four courses of consolidation therapy, he remained in complete remission and was discharged in September 1999.
In July 2002 he presented with fever and bone marrow aspiration, which at that time revealed 19.5% blast. Reinduction therapy with cytarabine 2 g/m2 every 12 h on days 1, 3, and 5 was begun, but he did not receive antibiotic and antimycotic prophylaxis. He received granulocyte colony-stimulating factor (G-CSF, filgrastim) 5µg/kg subcutaneously starting on day 6. G-CSF was stopped upon recovery of leukocytes to more than 10000/µl. On day 11 of reinduction therapy, he developed neutropenic fever and signs of respiratory failure with tachypnea and hypoxia. Chest X-rays showed pulmonary infiltration of the right, middle and lower lobes. Intravenous broad spectrum antibiotics were started and escalated with vancomycin and fluconazole, but the high fever continued and his clinical condition deteriorated. Aspergillus was not cultured from his sputum and serologic testing, antigen test, and blood culture was negative. However, 1,3-beta-D-glucan was increased to 30.63 pg/ml(normal value<4.95 pg/ml). Endotoxin was below 0.95 pg/ml(normal value<0.95 pg/ml) and fluconazole was not effective. As Aspergillosis was suspected, fluconazole was discontinued and intravenous amphotericin B (1 mg/kg/day) was initiated on day 20.
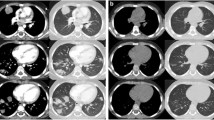
After starting treatment with amphotericin B, his respiratory condition improved, followed a week later by resolution of the fever. On day 42, bone marrow aspiration revealed complete hematological remission. CRP and 1,3-beta-D-glucan was decreased, but Chest X-ray showed minor regression of infiltrates. Computed tomography (CT) showed the presence of pulmonary infiltrates and cavity in the right, middle lobe (Fig. 1). On day 44, bronchoscopy was performed and showed hyperemia, erosion, and red swelling lesion in the bronchial mucosa of the right, middle lobe. A transbronchial biopsy was performed on a red swelling lesion, which was microscopically identified as Aspergillus fumigatus (Fig. 2). Chest X-rays gradually demonstrated improvement of pulmonary infiltrates, but remained as a hazy shadow. 1,3-beta-D-glucan was decreased to 5.40 pg/ml but remained positive. After 57 days of therapy with amphotericin B (total dose 2850 mg), the antifungal regimen was changed to oral itraconazole (200 mg/day). Serum creatine rose during amphotericin B therapy from 0.84 mg/dl to 2.18 mg/dl, but stabilized at 1.5 mg/dl after the antimycotic agent was changed. On day 98 of consolidation therapy, cytarabine 2 g/m2 every 12 h on days 1 and 3, followed by G-CSF, was initiated and itraconazole was continued as a secondary prophylaxis. He did not develop neutropenic fever or signs of respiratory distress on this therapy. On day 122, bone marrow aspiration maintained signs of complete hematological remission.
On day 130, a second consolidation therapy with cytarabine 2 g/m2 every 12 h on days 1 and 3, followed by G-CSF, was initiated and itraconazole was continued as secondary prophylaxis. Neutropenic fever and signs of respiratory failure with tachypnea and hypoxia recurred on day 9 of the second consolidation therapy. Chest X-rays showed pulmonary infiltrates in the right, middle and lower lobes and 1,3-beta-D-glucan was increased to 23.8 pg/ml. Itraconazole was subsequently changed to intravenous amphotericin B (1 mg/kg), broad spectrum antibiotics were started, and the fever and respiratory conditions improved. On day 142, his urinary output decreased and serum creatinine increased from 1.85 mg/dl to 4.1 mg/dl during a treatment with amphotericin B. Since he did not show signs of improvement, amphotericin B was changed to intravenous micafungin (300 mg/day). After the change of treatment, chest X-rays showed regression of the pulmonary infiltrate and micafungin was continued for 50 days. As a result, serum creatinine decreased from 4.1 mg/dl to 1.42 mg/dl, chest X-rays showed no abnormal shadow and 1,3-beta-D-glucan was below 4.95 pg/ml. He was discharged on day 193 and continues to be without evidence of relapse of his leukemia and remains free of mycotic infection (Fig. 3).
Discussion
We reported the diagnosis of invasive pulmonary aspergillosis during a second consolidation with high-dose cytarabine and the repeated treatment and clinical improvement with amphotericin B; however, renal failure due to amphotericin B occurred and treatment with micafungin showed clinical improvement. As the earlier formulation of itraconazole (capsule form) was poorly absorbed in patients with prolonged neutropenia with gastrointestinal damage following chemotherapy and radiotherapy [5], the low dose of itraconazole as secondary prophylaxis might induce invasive pulmonary aspergillosis; thus, serum-levels of itraconazole should generally be measured during the clinical course. If these levels had been sub-therapeutic, other antifungal drugs such as amphotericin B might have been utilized, although placebo-controlled trials of an adequate size have not yet been carried out [6].
Micafungin is a novel, water-soluble echinocandin lipopeptide that has been developed by Fujisawa Pharmaceutical, Osaka, Japan [7, 8, 9]. Micafungin is a new parenterally administered antifungal drug of the echinocandin class of antifungal agents. 1,3-beta-D-glucan, a structural piece of the fungal cell wall, is essential for the cell to grow and divide. Micafungin noncompetitively inhibits the synthesis of 1,3-beta-D-glucan, leading to disruption of the growing fungal cell wall and death of the fungal cell [10]. As 1,3-beta-D-glucan is not found in mammalian cells, micafungin is specific for fungi and appears to have limited mammalian toxicity. Several investigations have shown that detection of beta-D-glucan is a good marker for deep-seated fungal infection [11, 12]. Micafungin has not only excellent in vitro activity against both Candida and Aspergillus, but also promising in vivo activity in animal models of disseminated candidiasis and aspergillosis [13]. Preliminary clinical studies with the drug against esophageal candidiasis in HIV-positive patients [14], febrile neutropenic patients [15], patients with deep mycosis [16], and patients with cancer and with candidemia [17] have also demonstrated good activity. Recently, a large trial has shown the effectiveness of treatment with micafungin in invasive aspergillosis [18]. The most commonly reported adverse reactions are headache, fever, rash, diarrhea, phlebitis, and mild liver and renal function test elevations [17]. Nephrotoxicity is often a dose-limiting side effect of amphotericin B, but is uncommon with micafungin.
In conclusion, micafungin appears to be an effective therapy for invasive pulmonary Aspergillus fumigatus infection in acute myeloid leukemia with renal failure due to amphotericin B. Additional studies are necessary to further evaluate its efficacy and indications.
References
Denning DW (1998) Invasive aspergillosis. Clin Infect Dis 26:781–803
Dannauoui E, Borel E, Persat F, Piens MA, Picot S (2000) Amphotericin B resistance of Aspergillus terreus in a murine medel of disseminated aspergillosis. J Med Microbiol 49:601–606
Meunier F (1994) Alternative modalities of administering amphotericin B: current issues. J Infect 28[Suppl 1]:51–6
Fanos V, Catalfi Ll (2000) Amphotericin B-induced nephrotoxicity: a review. J Chemother 12:463–470
Pretice HG, Caillot D, Dupont B (1999) Oral and intravenous itraconazole for systemic fungal infections in neutropenic haematological patients. Acta Haematol 101:56–62
Cornely OA, Ullmann AJ, Karthaus M (2003) Evidence-based assessment of primary antifungal prophylaxis in patients with hematologic malignancies. Blood 101:3365–3372
Iwamoto T, Sakamoto N, Yamashita M (1993) FR90139, a novel antifungal antibiotic. In: Abstract 371 of the 33rd Intersci Conf Antimicrob Agents Chemother, New Orleans, 27–20 Oct
Ueda S, Tanaka M, Ezaki M (1998) Studies on a novel lipopeptide acylase(FR901379 acylase) from Streptomyces sp. for production of FR179642, a key intermediate of antifungal lipopeptide drug FK 463. In: Abstract F 145 of the 38th Intersci Conf Antimicrob Agents Chemother, San Diego,24–27 Sept
Fromtling RA, Castner J (1998) FK-463. Drugs Future 23:1273–1278
Fromtling RA (2002) Micafungin sodium (FK-463). Drugs Today 38:245–257
Kohno S, Mitsutake K, Maesaki S, Yasuoka A, Miyazaki T, Kaku M, Koga H, Hara K (1993) An evaluation of serodiagnostic tests in patients with candidemia:beta-D-glucan, mannan, Candida antigen by Cand-Tec and D-arabinitol. Microbiol Immunol 37:207–212
Obayashi T, Yoshida M, Mori T, Goto H, Yasuoka A, Iwasaki H, Teshima H, Kohno S, Horiuchi A, Ito A (1995) Plasma(1➠3)-beta-D-glucan determination in the diagnosis of invasive deep mycosis and fungal febrile episodes. Lancet 345:17–20
Warn PA, Morrissey G, Morrissey J, Denning DW (2003) Activity of micafungin (FK463) against an itraconazole-resistant strain of Aspergillus fumigatus and a strain of Aspergillus terrus demonstrating in vivo resistance to Amphotericin B. J Antimicrob Chemother 51:913–919
Pettengell K, Mynhardt J, Kluyts T (2000) A multicentre study of the echinocandin antifungal FK 463 for the treatment of esophageal candidiasis in HIV positive patients. In: Abstract of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, Toronto, Ontario, Canada, Abstract 1104, p 371. American Society for Microbiology, Washington, DC, USA
Seibel NL, Schwartz C, Arrieta A (2000) Phase I study to determine the safety and Pharmacokinetics (PK) of FK463 (Echinocandin) in febrile neutropenic pediatric patients. In: Abstract of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, Toronto, Ontario, Canada, Abstract 18, p 1. American Society for Microbiology, Washington, DC, USA
Kohno S, Masaoka T, Yamaguchi (2001) A multicenter, open label clinical study of FK 463 in patients with deep mycosis in Japan. In: Abstract J-834 of the 41st Intersci Conf Antimicrob Agents Chemother, Chicago, 22–25 Sept
Kontoyiannis DP, Buell D, Frisbee-Hume S (2001) Initial experience with FK463 for the treatment of candidemia in cancer patients. In: Abstract J-1629 of the 41st Intersci Conf Antimicrob Agents Chemother, Chicago 22–25 Sept
Ullmann AJ, Van Burik JA, McSweeney P, Ratanatharathom V, Raymond J, de Morais VL, McGuirk J, Lau W, Facklam D, Koblinger S, Reusch M, Marr K, Patterson TF, Denning DW (2003) An open phase II study of the efficacy of micafungin (FK463) alone and in combination for the treatment of invasive aspergillosis (IA) in adults and children. 13th ECCMID meeting, Glasgow, Scotland, UK
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yokote, T., Akioka, T., Oka, S. et al. Successful treatment with micafungin of invasive pulmonary aspergillosis in acute myeloid leukemia, with renal failure due to amphotericin B therapy. Ann Hematol 83, 64–66 (2004). https://doi.org/10.1007/s00277-003-0736-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-003-0736-8