Abstract
Purpose
There is confusion regarding the names, the number, and the exact location of the colonic arterial arches which provide connections between the superior and inferior (IMA) mesenteric arteries at the level of the left colic angle. The aim of this review was to delineate the “true” colic arches arising in the meso of the left colic angle and to describe their surgical implications.
Methods
A systematic review of the literature was performed using the MEDLINE database. The search included only human studies between 1913 and 2018. All dissection, angiographic, arterial cast and corrosion studies were analyzed.
Results
The terms “Riolan arch”, “marginal artery of Drummond”, “meandering mesenteric artery” and “Villemin’s arch” must no longer be used in the scientific literature. Three arterial arches were found at the level of the left colic angle, permitting the communication between the two arterial mesenteric systems: (1) the Marginal Artery (the most peripheral, found in 100% of cases); (2) the “V” termination of the ascending branch of the left colic artery (LCA), existing in more than 2/3 of cases; and (3) the inter-mesenteric trunk, found more centrally located and existing in less than 1/3 of cases.
Conclusions
Three arterial arches exist at the level of the left colic angle: (1) the Marginal Artery, (2) the “V” termination of the ascending branch of the LCA, and (3) the inter-mesenteric trunk. The knowledge of this anatomy is essential for performing colorectal surgeries involving ligation of the IMA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is a confusion regarding the names, the number and the exact location of the colic arterial arches (peripheral and central), which provide connections between the superior (SMA) and inferior (IMA) mesenteric arteries at the level of the left transverse colon, the splenic flexure and the descending colon [1, 6, 7, 10, 11]. This connection between the two arterial systems is essential in colorectal surgeries involving ligature of the inferior mesenteric artery at its origin (especially in cancer patients), because it allows for vascularization of the descending colon by the superior mesenteric artery [3, 4, 6, 11, 22].
The Riolan arch and the marginal artery of Drummond are two major peripheral arterial arches described in the literature; however, the use of this terminology is decreasing due to the heterogeneity of their definitions:
-
Some authors exclusively use the term “marginal artery” to define the principle peripheral arc. The expression “Riolan arch” is never mentioned (Fig. 1a) [7, 10, 11, 19].
-
Some authors consider the marginal artery and the Riolan arch to be synonyms [11].
-
Other authors define the Riolan arch as a part of the marginal artery, connecting the middle colic artery to the ascending branch of the left colic artery (Fig. 1b) [1, 11].
-
Finally, some authors describe two independent arches: the Riolan arch is more important and central, connecting the middle colic artery to the left colic artery, whereas the marginal artery (of Drummond) is more peripheral, limited to the left colic angle and supplying the straight arteries (Fig. 1c) [6, 8, 11].
Central communications between the SMA and the left colic artery are found during laparoscopic left colectomy, and confusion arises once again because these communications are poorly described in the anatomic literature and the nomenclature is unclear (Villemin’s arch, inter-mesenteric trunk) [6, 11, 20].
Due to the confusion surrounding the colonic arterial arches, this review aimed to study the arterial structures found in the meso of the left colic angle and to clearly delineate the “true” colic arches and then describe their surgical implications.
Methods
A systematic overview of the literature was performed using the MEDLINE database using the following terminology: “Vascularization of the colon”, “colonic vascularization”, “Transverse colon”, “Spleen flexure”, “Riolan’s arch”, “artery of Riolan”, “meandering artery of Riolan”, “Inter-mesenteric artery”, “inter-mesenteric communications”, “Meandering mesenteric artery”, “Marginal artery of the colon”, “marginal artery of Drummond”, “Left colic artery”, “middle colic artery”, and “right colic artery”. The search included only human studies between 1913 and 2018. All dissection, angiographic, and arterial cast and corrosion studies concerning colic arterial anatomy were analyzed.
Results
After a systematic review of the literature, it is clear that the terms “Riolan arch”, “marginal artery of Drummond”, “meandering mesenteric artery” and “Villemin’s arch” must no longer be used in the scientific literature [1, 6, 7, 10, 11, 19, 20].
The distinct and separate arterial structures at the origin of the formation of the inter-mesenteric connections at the left colic angle are the marginal artery, the left branch of the middle colic artery, the ascending branch of the left colic artery and a number of central connections emerging from the origin of the IMA and/or SMA.
Marginal artery of the colon
The International anatomic designation of the marginal artery (or marginal arch) (MA) is “arteria marginalis coli.” A literature analysis found many synonyms, such as “marginal artery of Drummond”, “principal artery”, “primary artery”, “parallel artery” or “paracolic artery” [1]. All of these designations describe a continuous arterial duct bordering the colic wall between the cecum and the rectosigmoid junction, with a caliber varying from 2.5 to 3 mm [1]. The marginal artery is located approximately 2.5 cm from the mesocolic side of the colon. These are the straight arteries, emerging perpendicularly from the MA and vascularizing the colic wall.
The marginal artery is principal and is the more peripheral inter-mesenteric connection [11].
Many authors consider the MA to be constant and always present (prevalence of 100%), connecting the MCA and the LCA at the level of the left colic angle [1, 10, 17, 18, 20]. The connection between the marginal artery and the termination of the ascending branch of the left colic artery at the level of the left colic angle represents the zone between the IMA and SMA (Fig. 1a).
Middle colic artery
The middle colic artery (MCA) is an important collateral branch of the superior mesenteric system, forming the “true” right pillar of the marginal artery [1, 10, 13, 18]. The MCA emerges from the superior mesenteric artery at the level of the first jejunal artery. Its caliber varies from 2.2 to 3.5 mm. The MCA enters at the right part of the transverse mesocolon, and after a variable distance, it divides into 2 branches (Fig. 2):
-
The right branch of the MCA runs toward the right colic angle to anastomose with the ascending branch of the right colic artery and/or the ileocolic artery (if the right colic artery is absent) [1].
-
The left branch of the MCA runs through the meso of the left colic angle to anastomose with the ascending branch of the left colic artery, thus forming the left pillar (or left part) of the marginal artery. The left branch of the MCA is long and regular when compared to the right branch. The connection and continuity of the left branch of the MCA with the ascending branch of the LCA are considered to be quasi constant, however, some cases do exist where there is an interruption of the marginal artery occurring at this level (Griffith’s point). When the ascending branch of LCA is absent, the left branch of the MCA can reach the left colic angle and the left colic artery (incidence 7%) (Fig. 5) [1, 11, 20]. Recently, Miyake et al. [14] described the accessory middle colic artery (AMCA) as a feeding artery for the left-sided colon. The AMCA existed in 36.4% of the cases, originating from the superior mesenteric artery. The frequency of the presence of the AMCA was associated with the branching pattern of the LCA, and was more frequent when the LCA was absent [14].
The MCA is absent, on average, in 5% of cases (prevalence varies from 2 to 22% in the literature) [1, 10, 13]. In these cases, the vascularization of the transverse colon is assured by the right colic artery and a “pronounced” or prominent marginal artery.
Left colic artery
According to many authors, the Left colic artery (LCA) is the only artery that is constantly present for the vascularization of the left colon. However, other authors have described the absence of the LCA in 6% of cases [1, 6, 10, 11, 16, 22]. The LCA originates from the inferior mesenteric artery, 4–6 cm from the left border of the L4 vertebral body. We can describe two kinds of origins: the isolated departure from the colosigmoid trunk (80%) or the departure “in branches” [22]. Its mean length is 15.6 cm with a caliber varying from 1.9 to 3 mm [1]. Initially, the LCA runs transversely to the left; it then crosses the inferior mesenteric vein and divides into two branches. First, the descending branch anastomoses to the superior sigmoidal artery to vascularize the left colon and sigmoid colon. Second, the ascending branch of the LCA rises to the left colic angle to constitute the left pillar of the marginal artery at this level.
Ascending branch of the left colic artery
The ascending branch of the LCA (ABLCA) represents the left pillar of the connections between the superior and inferior mesenteric systems through the intermediary of the marginal artery. The ABLCA is found in between 63% and 100% of cases [1, 10, 13, 17, 18]. When it is present, it runs parallel to the inferior mesenteric vein and ultimately joins the marginal artery after dividing at the left colic angle (splenic flexure). The ascending branch of the LCA divides into two branches forming a “V” at termination that directly connects to the marginal artery (Fig. 3) [1, 11, 13]:
-
1.
The medial branch, which supplies the transverse colon, eventually joins the left branch of the middle colic artery and helps form the right part of the marginal artery.
-
2.
The lateral branch, which supplies the descending colon, ultimately joins the superior sigmoidal artery and helps form the left part of the marginal artery.
The terminal bifurcation in a “V” by the ascending branch of the LCA represents a functional and valid anastomotic arterial arch supplementary to the marginal artery. In 14% of cases, the medial branch of the terminal bifurcation is absent, leaving the vascularization of the left colic angle solely dependent on the marginal artery [13]. Lange et al. [11] demonstrated that the marginal artery and the “V” termination of the ABLCA must be considered two functional peripheral arches at the level of the left colic angle. The marginal artery is more peripheral than the “V” termination of the ABLCA; however, this “V” termination constitutes a true second order arch capable of compensating for a discontinuous marginal artery at the level of the left colic angle or splenic flexure (Griffith’s point) [10, 12].
Central inter-mesenteric communications
Central inter-mesenteric communications exist at the root of the mesocolon at the left colic angle, close to the duodenojejunal angle (angle of Treitz), and run along the cephalad aspect of the inferior mesenteric vein. These central communications, initially described by Vandamme and Villemin [6, 20], present some variable anatomic dispositions, but their prevalence is low (0–18%) [1, 10, 11, 13, 18, 20].
The best-known and most well-described central communication is the “inter-mesenteric trunk” (IMT). This artery represents when added to the MA and ABLCA, a third way of communication (third arch) between the superior and inferior mesenteric systems at the level of the left colic angle.
Initially described on cadavers as the “arcus inter-mesentericus” [20], the IMT is named “arteria ascendens” in the international anatomic nomenclature. Its prevalence is variable, measuring between 12 and 18%, depending on the study [1, 20]. This vessel, often forgotten, is defined using a simple and precise classification based how the IMT connects the two mesenteric axes (Fig. 4) [1].
-
Direct IMT: when a direct connection exists between the origins of the SMA and the IMA.
-
Mixed IMT: when a connection exists between the origin of one of the two mesenteric arteries and one of the main branches of the other mesenteric arteries, with the most frequent example being a connection between the origin of the SMA and the Left colic artery.
-
Indirect IMT: when a connection exists between two main branches of both mesenteric arteries (SMA, IMA). In most cases of this, the connection exists between the Middle colic artery and the Left colic artery, however, this specific connection is clearly proximal and central (in contrast to the marginal artery, which is distal and peripheral).
The path the inter-mesenteric trunk follows varies depending on its type. In the “direct” and “mixed” types, the IMT follows alongside the inferior mesenteric vein, parallel to the spinal column, usually connecting at the origin of the SMA. In the “indirect” type, the connection between the LCA and the MCA is more lateral (Fig. 4).
Discussion
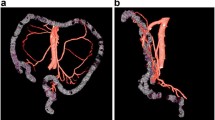
The arch theory by Mac Kay and Tandler contends that longitudinal arterial anastomosis account for the genesis of the arterial trunk anastomoses and the main anatomic variations [6]. This review demonstrates that the mesenteric arteries are joined together by three types of arterial arches at the level of the left colic angle (Fig. 5), with each one having a variable prevalence:
-
Arch of first order, the most peripheral and the most common: the Marginal Artery, which is quasi constant (100%) [1, 10, 17, 18, 20].
-
Arch of second order, the “V” termination of the ascending branch of the left colic artery. It can compensate for a discontinuous marginal artery at the level of the left colic angle. It should be noted that the ascending branch of the LCA is present in 63 to 100% of cases [10, 13, 17, 18]. Its “V” termination can be absent in 14% of cases [13].
-
Arch of third order, more central: the inter-mesenteric trunk, existing in less than 18% of cases [1, 20].
The term “meandering mesenteric artery” (MMA) was used by some authors as a synonym to the Riolan’s arc [9, 15, 21]. Introduced by Moskowitz et al. [15], It represented a large and tortuous vessel connecting the proximal segments of the MCA and the LCA. The MMA was only described in radiologic studies in cases of specific atherosclerosis of the digestive arteries. After a rigorous analysis of the literature, the MMA was determined to represent a hypertrophied and tortuous marginal artery present during chronic atherosclerotic pathologies of the mesenteric vasculature. Use of the term “meandering mesenteric artery” must be abolished.
At the level of the meso at the left colic angle, many anatomic arguments exist for assigning a clinical role to the marginal artery. In fact, during injected contrast studies of the SMA, some authors discovered a permeability rate of 100% associated with the MA at the left colic angle (Fig. 5) [18]; a significant permeability rate was confirmed by performing studies on cadavers [2].
In contrast to these results, other authors described a discontinuous MA at the level of the left colic angle. This discontinuity leads to a functional insufficiency of the MA at this level, and defines the critical point of Griffiths [10, 12]. This specific point represents an area of weakness, related to the MA, which can lead to ischemic colic phenomena downstream (Fig. 6).
These contradictions between authors might be explained by the fact that Steward et al. [18] and Binns et al. [2] did not ligate the two terminal branches of the termination of the ascending branch of the LCA, forgetting the possibility that the specific “V” termination can connect the SMA to the IMA., At the end, this “V” termination can bypass (i.e., bridge) an eventual insufficiency of the MA at the level of the left colic angle (Fig. 6b, c).
These significant observations confirmed the presence and the functional role of a second peripheral arch formed by the “V” termination of the ascending branch of the LCA at the left colic angle. It represents a second arterial axis, supplementary to the marginal artery, that can compensate for a discontinuous MA and can connect the superior and inferior mesenteric systems. Regarding these results, it is important to respect the terminal bifurcation of the ascending branch of the LCA during all left colic surgery encompassing IMA ligature at its origins. This is especially critical in cases involving an insufficient marginal artery at the left colic angle. These vascular anastomoses are normally preserved in cases of high-tie (transection of the inferior mesenteric artery) or low-tie (transection of the superior rectal artery with preservation of the left colic artery) IMA ligature without any additional meso transection at the level of the left colic angle. In high tie IMA ligature, surgeons must recut the LCA trunk, while preserving the V termination of the ascending branch of the LCA during the meso transection.
No significant differences were found in the fistula rate or in the number of lymph nodes removed between high tie or low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery [3,4,5, 16, 22]; however, Bonnet et al. [3, 4] observed that colon length was 10 cm greater for high-tie vascular transections with conservation of the left colic artery when compared to low-tie vascular transections.
Finally, all these observations raise three major points:
-
Surgeons need to preserve the “V” termination of the ascendant branch of the LCA. By the fact that there is no routine exam to evaluate the permeability of the marginal artery, the conservation of this termination (arch of second order) appears essential to avoid any colic ischemia in cases involving a discontinuous marginal artery (Fig. 6a).
-
In cases with a discontinuous MA with a functional “V” termination of the ascendant branch of the LCA, the preservation of the LCA is advised but not mandatory (Fig. 6b).
-
Finally, in cases with both a discontinuous MA and an absent medial branch of the ascending branch termination of the LCA, the preservation of the LCA appears theoretically mandatory to maintain adequate vascularization of the colon (Fig. 6c).
Concerning the inter-mesenteric trunk, its low prevalence (< 20%) and the absence of a rigorous evaluation of its functional capacity to connect the two mesenteric axes, the literature does not support the idea that adequate vascularization of the colon will be accomplished by the inter-mesenteric trunk alone [1, 11, 20]. In fact, opinions differ regarding its function because some authors consider the IMT to be a real central structure involved in supplying vascularization under normal physiologic situations, whereas other authors consider it a permeable vascular axis, which becomes functional only in pathologic conditions (e.g., meandering mesenteric artery).
The IMT can garner clinical interest in cases of ligature of the IMA at its origins when the MA is discontinuous and an absent medial branch of the termination of the ascending branch of the LCA.
All of these specific situations need to be analyzed when they arise (Fig. 7). Surgeons must make their best effort to avoid surgery that is too invasive or involves unnecessary dissection of the meso at the left colic angle solely in pursuit of preserving the “V” termination of the ascending branch of the LCA or a possible IMT. However, the preservation of the IMT appears difficult after ligature of the inferior mesenteric vein when a complete left colic angle mobilization is required for tension-free colorectal or coloanal anastomosis.
Conclusion
The review of the literature demonstrated the presence of 3 types of arterial arcs at the level of the left colic angle, allowing the communication between the two arterial mesenteric systems (Fig. 5):
-
Arch of the first order, the most peripheral and the most frequent: the Marginal Artery (prevalence of 100%).
-
Arch of the second order, the “V” termination of the ascending branch of the left colic artery (existing in more than 2/3 of cases).
-
Arch of the third order, more central: the inter-mesenteric trunk, (existing in fewer than 1/3 of cases).
The knowledge of this anatomy is essential to perform colorectal surgeries involving the ligation of the IMA to preserve adequate vascularization of the colon, especially in cancer patients and some very specific anatomic situations. The transection of the meso of the left colic angle must be performed carefully to preserve the marginal artery and the “V” termination of the LCA. The preservation of the inter-mesenteric trunk is required, but usually impossible during the left colic angle mobilization after ligature of the inferior mesenteric vein.
References
Bertelli L, Lorenzini L, Bertelli E (1996) The arterial vascularisation of the large intestine. Anatomical and radiological study. Surg Radiol Anat 18(Suppl 1):A1–A6 (S1–59)
Binns JC, Isaacson P (1978) Age-related changes in the colic blood supply: their relevance to ischemic colitis. Gut 19:384–390
Bonnet S, Abid B, Wind P, Delmas V, Douard R (2013) Anatomical basis of laparoscopic medial-to-lateral mobilization of the descending colon. Clin Anat 26:377–385
Bonnet S, Berger A, Hentati N et al (2012) High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum 55:515–521
Corder AP, Karanjia ND, Williams JD et al (1992) Flush aortic tie versus selective preservation of the ascending left colic artery in low anterior resection for rectal carcinoma. Br J Surg 79:680–682
Douard R, Chevallier JM, Delmas V, Cugnenc PH (2006) Clinical interest of digestive arterial trunk anastomoses. Surg Radiol Anat 28:219–227
Drummond H (1913) The arterial supply of the rectum and pelvic colon. Br J Surg 1:677–685
Gallot D (2006) Anatomie chirurgicale du côlon. EMC Tech Chir Appar Dig 1:1–8
Gourley EJ, Gering SA (2005) The meandering mesenteric artery: a historic review and surgical implications. Dis Colon Rectum 48:996–1000
Griffiths JD (1956) Surgical anatomy of the blood supply of the distal colon. Ann R Coll Surg Eng 19:241–256
Lange JF, Komen N, Akkerman G et al (2007) Riolan’s arch: confusing, misnomer, and obsolete. A literature survey of the connection(s) between the superior and inferior mesenteric arteries. Am J Surg 193:742–748
Meyers MA (1976) Griffiths’ point: critical anastomosis at the splenic flexure. Significance in ischemia of the colon. Am J Roentgenol 126:77–94
Michels NA, Siddharth P, Kornblith PL et al (1963) The variant blood supply to the small and large intestines: its import in regional resections. J Int Coll Surg 39:127–170
Miyake H, Murono K, Kawai K et al (2018) Evaluation of the vascular anatomy of the left-sided colon focused on the accessory middle colic artery: a single-center study of 734 patients. Colorect Dis. https://doi.org/10.1111/codi14287
Mosckowicz M, Zimmerman H, Felson B (1964) The meandering mesenteric artery of the colon. Am J Roentgenol 92:1088–1099
Patroni A, Bonnet S, Bourillon C et al (2016) Technical difficulties of left colic artery preservation during left colectomy for colon cancer. Surg Radiol Anat 38:477–484
Peters JH, Kronson JW, Katz M et al (1995) Arterial anatomic considerations in colon interposition for oesophageal replacement. Arch Surg 130:858–863
Steward JA, Rankin FW (1933) Blood supply of the large intestine. Its surgical considerations. Arch Surg 26:843–891
Siddharth P, Ravo B (1988) Colorectal neurovasculature and anal sphincter. Surg Clin North Am 68:1185–1200
VanDamme JP (1993) Behavioural anatomy of the abdominal arteries. Surg Clin North Am 73:699–725
VanGulik TM, Schoots I (2005) Anastomosis of Riolan revisited; the meandering mesenteric artery. Arch Surg 140:1225–1229
Voron T, Douard R, Berger A (2016) Conservation of the left colic artery during laparoscopic left-hemicolectomy for cancer. J Chir Visc 153:39–43
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Research involving human participants and/or animals
All applicable institutional and/or national guidelines were followed.
Informed consent
Informed consent does not apply.
Rights and permissions
About this article
Cite this article
Bruzzi, M., M’harzi, L., El Batti, S. et al. Inter-mesenteric connections between the superior and inferior mesenteric arteries for left colonic vascularization: implications for colorectal surgery. Surg Radiol Anat 41, 255–264 (2019). https://doi.org/10.1007/s00276-018-2139-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-018-2139-5