Abstract
Introduction
The aim of this study was to determine the location and distribution pattern of neurovascular structures superior and inferior to the clavicle by detailed dissection.
Methods
Fifteen adult non-embalmed cadavers with a mean age of 71.5 years were studied. For measurements, the most prominent point of the sternal end of the clavicle (SEC) on anterior view and the most prominent point of the acromial end of the clavicle (AEC) were identified and divided five equal sections before dissection. A line connecting the SEC and AEC was used as a reference line. The surrounding neurovascular structures were investigated.
Results
The supraclavicular nerve was mainly distributed in the second and the third sections (distribution frequency: 41.30% and 30.43%, respectively) from AEC. Branches of the thoracoacromial artery were mainly distributed in the second, third, and fourth sections (distribution frequency: 21.15%, 26.92%, and 28.85%, respectively). Branches of the subclavian vein were mainly distributed in the third and fourth sections (distribution frequency: 23.26 and 30.23%, respectively). Distribution frequency of subclavian vein, subclavian artery, and brachial plexus ranged from 31.3 to 57.5%.
Discussion
When the clavicle was divided into five sections, there was relatively little distribution of neurovascular damage in the first section or the fifth section. This study reveals the average location of subclavian vein with artery and brachial plexus. Results of this study could be used as reference during surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clavicle is one of the most commonly fractured bones in the human body. Fractures of the clavicle account for 5–12% of all fractures and 35–44% of all injuries to the shoulder girdle. Approximately 81% of these fractures occur in the middle third of the clavicle. They are usually accompanied by displacement by deforming forces from muscular attachments [8, 12].
These fractures can often be managed by an arm sling or splint with pain medicine. However, nonoperative management of clavicular fractures is associated with high rates of nonunion and symptomatic malunion with shortening [3, 18]. Displaced bone fragments can injure surrounding vessels and nerves. In some cases, implant failure might be a risk factor for neurovascular structure.
Open reduction and internal fixation (ORIF) of a displaced fracture can lead to some complications of vessels and nerves located close to the clavicle [11, 14]. Although a few studies have determined neurovascular structures of the clavicle [2, 5, 6, 10, 11, 14, 16], delicately dissected study for small nerve and vessels of the clavicle is limited.
Therefore, the objective of this study was to determine the location and distribution pattern of neurovascular structures superior and inferior to the clavicle by detailed dissection.
Materials and methods
Fifteen adult non-embalmed cadavers (eight males and seven females) with a mean age of 71.5 years (range 49–88 years) were studied. These specimens were chosen without a history of clavicle fracture or prior surgery to the clavicle or shoulder.
For measurements, the most prominent point of the sternal end of the clavicle (SEC) on anterior view and the most prominent point of the acromial end of the clavicle (AEC) were identified before dissection. A line connecting the SEC and AEC was used as a reference line. Reference point was expressed in absolute distance along the reference line using SEC as the starting point.
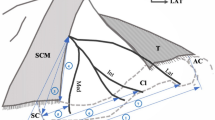
With the specimen in supine position, different colored latexes were injected into the artery (pink) and vein (blue) on the elbow region to the shoulder. Only the skin was removed to expose the fatty layer to find supraclavicular nerve for measurement. The superficial fascia was carefully removed to find subcutaneous vein under the clavicle (Fig. 1). After measuring that, subcutaneous tissue was removed to identify pectoralis major and clavicle. A few muscles attached to the clavicle were then carefully removed to find small artery for measurement (Fig. 2). Brachial plexus, thoracoacromial trunk with its branches, and subclavian artery with vein were measured in this study (Fig. 3).
Photograph showing neurovascular structures under the clavicle after cutting part of the middle of clavicle. SCM sternocleidomastoid, SEC the most prominent point of the sternal end of the clavicle on the anterior view, AEC the most prominent point of the acromial end of the clavicle on the anterior view, BP brachial plexus, SUP superior, LAT lateral
The supraclavicular nerve, branches of thoracoacromial trunk, and subclavian vein were investigated to determine the distribution frequency to understand how many branches were located in that area after dividing them to five equal sections on the reference line.
A single observer obtained all measurements using a measuring tape and digital calipers (resolution 0.01 mm, CD-20PSX, Mitutoyo, Japan). Data were analyzed using SPSS software version 23.0 (IBM SPSS Inc., Chicago, IL, USA).
Results
The mean distance of the reference line from the SEC to AEC was 15.8 ± 1.4 cm. There was no significant difference in reference line distance between males and females or between right and left ankles (p ≥ 0.05).
The first, second, third, fourth, and fifth branches of the supraclavicular nerve were located at 15.6%, 31.2%, 48.6%, 67.5%, and 90.1% of the reference line from the AEC, respectively. Distribution frequencies of those branches were 4.35%, 41.30%, 30.43%, 19.57%, and 4.35% respectively (Table 1; Fig. 4).
Photograph showing distribution frequency of the supraclavicular nerve after dividing the clavicle into five equal sections. SEC the most prominent point of the sternal end of the clavicle on the anterior view, AEC the most prominent point of the acromial end of the clavicle on the anterior view, SUP superior, LAT lateral, ANT anterior
The thoracoacromial trunk was located at 48.7% on the X-coordinate and 12.2% on the Y-coordinate of the reference line from AEC. These five branches from the thoracoacromial trunk were located at 14.5%, 30.6%, 49.1%, 67.4%, and 86.7% of the reference line from AEC. Distribution frequencies of these branches were 11.54%, 21.15%, 26.92%, 28.85%, and 11.54%, respectively (Table 2; Fig. 5).
Photograph showing distribution frequency of the thoracoacromial trunk with its branches after dividing the clavicle into five equal sections. SEC the most prominent point of the sternal end of the clavicle on the anterior view, AEC the most prominent point of the acromial end of the clavicle on the anterior view, TAT thoracoacromial trunk, SUP superior, LAT lateral, ANT anterior
The first, second, third, fourth, and fifth branch of the subclavian vein were located at 15.0%, 36.1%, 53.5%, 72.8%, and 84.0% of the reference line from the AEC, respectively. Distributed frequencies of these branches were 11.63%, 16.28%, 23.26%, 30.23%, and 18.60%, respectively (Table 3; Fig. 6).
Photograph showing distribution frequency of branches of subclavian vein after dividing the clavicle into five equal sections. SEC the most prominent point of the sternal end of the clavicle on the anterior view, AEC the most prominent point of the acromial end of the clavicle on the anterior view, SUP superior, LAT lateral, ANT anterior
The subclavian vein, subclavian artery, and brachial plexus were located from 31.3%, 41.4%, 45.5–41.0%, 47.2%, and 57.5% (Table 4; Fig. 7).
Photograph showing distribution frequency of subclavian vein and artery as well as brachial plexus of the clavicle. SEC the most prominent point of the sternal end of the clavicle on the anterior view, AEC the most prominent point of the acromial end of the clavicle on the anterior view, SCV subclavian vein, SCA subclavian artery, BP brachial plexus, SUP superior, LAT lateral, ANT anterior
Discussion
In implant failure, nerve palsy has been reported 5.7%. The most common complication is brachial plexus symptom (about 13.0%) [11]. In other reports, approximately 2.0–5.0% of all fractures in adults and 10.0–15.0% of all fractures in children involve the clavicle. In case of clavicle fracture, almost cases are midshaft fractures, while lateral-third fractures are less common, accounting for 25.0% of all the cases [7, 13, 18]. In this study, we did not include a children group. Specimens were from those aged from 49 to 88 years. There will be no helpful data about children case; however, this results were used not only fracture site can be predicted which structures were damaged but to minimize neurovascular damage during surgery.
Robinson et al. [14] have examined relationships of neurovascular structures to the clavicle using three-dimensional computed tomographic arteriograms. They targeted subclavian artery with the same vein and brachial plexus to show the distance from these structures to clavicle cortex. Sinha et al. [15] have also used radiological method to study screw safety zone. However, these studies were radiological studies targeting very big structures such as subclavian vessels and brachial plexus. We injected color latex into the vessel differently and investigated very fine dissections. Robinson et al. [14] have indicated that neurovascular risk is the most significant during screw placement of clavicle. In addition, they have insisted that no clear-cut guidelines should be established for the treatment of displaced fractures of the clavicle. Subclavian vessel and brachial plexus injuries have been reported with plunging while drilling and exposing screw tips [7]. A subclavian vein thrombosis requiring long-term therapeutic anticoagulation has also been reported [9]. Our results from dissection can be used as guidelines to clinical field to prevent severe neurovascular injuries (Figs. 4, 5, 6, 7).
Other anatomical studies have been well conducted. Anastasopoulos et al. have reported that the external jugular vein crosses superficial to the lateral third of the clavicle [2]. Havet et al. have clarified the branch pattern network of supraclavicular nerve [6]. Later, Havet et al. have demonstrated arterial supply to the middle third of the clavicle [5]. Stillwell et al. have divided clavicle into three parts and investigated subclavian artery with vein and brachial plexus for safe osteosynthesis in clavicle fracture [16]. We measured neurovascular structures passing through the reference line to provide information for the clinical field. The limitation of this study was that we did not trace the origin of target neurovascular structures (Figs. 1, 2, 3). According to a Greek study, the supraclavicular nerve passes through the foramen or groove of clavicle in rare cases [10]. However, we did not find supraclavicular nerve-perforated clavicle (Fig. 1).
Congenital pseudarthrosis of the clavicle is a relatively rare pathology. Up to date, more than 200 cases have been reported. Female patients and the middle part of the clavicle unilaterally (especially the right side) seem to be more frequently affected. However, about 10% cases have occurred bilaterally [1, 4, 17]. A recent study has investigated abnormal shape of clavicle for the clinical field [19]. However, this study focused on neurovascular structures under the clavicle to provide locational information about their densely distributed areas (Figs. 4, 5, 6, 7).
The subclavius posticus muscle is an aberrant muscle originating from the medial aspect of the first rib, reaching to the superior border of the scapula. Depending on its activation, it may cause dynamic compression of the brachial plexus. Patients with thoracic outlet syndrome might develop carpal tunnel syndrome. The clavicle is also closely linked to upper limb syndrome. However, this study did not reveal its relationship with structures, including the subclavius muscle.
In this study, the supraclavicular nerve was densely distributed at the second and third sections in 71.73% of all the cases (Table 1; Fig. 4). Branches of the thoracoacromial artery were located in the second, third, and fourth sections in 76.92% of all the cases. The thoracoacromial trunk was located at 48.7% on x-coordinate and 12.2% on y-coordinate (Table 2; Fig. 5). Branches of subclavian vein were evenly distributed at all sections. However, their distribution was more common in the third and fourth sections (Table 3; Fig. 6). The subclavian vein and artery and brachial plexus were located from 31.3 to 57.5%. That area needs caution, because major neurovascular structures run underneath the clavicle (Table 4; Fig. 7).
References
Abdellaoui H, Atarraf K, Chater L, Afifi MA (2017) Congenital pseudarthrosis of the clavicle treated by Masquelet technique. BMJ Case Rep
Anastasopoulos N, Paraskevas G, Apostolidis S, Natsis K (2015) Three superficial veins coursing over the clavicles: a case report. Surg Radiol Anat 37:1129–1131
Der Tavitian J, Davison J, Dias J (2002) Clavicular fracture non-union surgical outcome and complications. Injury 33:135–143
Di Gennaro GL, Cravino M, Martinelli A, Berardi E, Rao A, Stilli S, Trisolino G (2017) Congenital pseudarthrosis of the clavicle: a report on 27 cases. J Shoulder Elbow Surg 26:e65–e70
Havet E, Duparc F, Tobenas-Dujardin A, Muller J, Delas B, Fréger P (2008) Vascular anatomical basis of clavicular non-union. Surg Radiol Anat 30:23–28
Havet E, Duparc F, Tobenas-Dujardin A, Muller J, Fréger P (2007) Morphometric study of the shoulder and subclavicular innervation by the intermediate and lateral branches of supraclavicular nerves. Surg Radiol Anat 29:605–610
Hussey MM, Chen Y, Fajardo RA, Dutta AK (2013) Analysis of neurovascular safety between superior and anterior plating techniques of clavicle fractures. J Orthop Trauma 27:627–632. https://doi.org/10.1097/BOT.0b013e31828c1e37
Lazarides S, Zafiropoulos G (2006) Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg 15:191–194
Naimark M, Dufka FL, Han R, Sing DC, Toogood P, Ma CB, Zhang AL, Feeley BT (2016) Plate fixation of midshaft clavicular fractures: patient-reported outcomes and hardware-related complications. J Shoulder Elbow Surg 25:739–746
Natsis K, Totlis T, Chorti A, Karanassos M, Didagelos M, Lazaridis N (2016) Tunnels and grooves for supraclavicular nerves within the clavicle: review of the literature and clinical impact. Surg Radiol Anat 38:687–691
Navarro RA, Gelber JD, Harrast JJ, Seiler JG, Jackson KR, Garcia IA (2016) Frequency and complications after operative fixation of clavicular fractures. J Shoulder Elbow Surg 25:e125–e129
O’Neill BJ, Hirpara KM, O’Briain D, McGarr C, Kaar TK (2011) Clavicle fractures: a comparison of five classification systems and their relationship to treatment outcomes. Int Orthop 35:909–914
Qiu X, Wang X, Zhang Y, Zhu Y, Guo X, Chen Y (2016) Anatomical study of the clavicles in a Chinese population. Biomed Res Int
Robinson L, Persico F, Lorenz E, Seligson D (2014) Clavicular caution: an anatomic study of neurovascular structures. Injury 45:1867–1869
Sinha A, Edwin J, Sreeharsha B, Bhalaik V, Brownson P (2011) A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Jt Surg Br 93:1247–1252. https://doi.org/10.1302/0301-620X.93B9.25739
Stillwell A, Ioannou C, Daniele L, Tan S (2017) Osteosynthesis for clavicle fractures: how close are we to penetration of neurovascular structures? Injury 48:460–463
Studer K, Baker MP, Krieg AH (2017) Operative treatment of congenital pseudarthrosis of the clavicle: a single-centre experience. J Pediatr Orthop B 26:245–249
Van der Meijden OA, Gaskill TR, Millett PJ (2012) Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg 21:423–429
Viciano J, Urbani V, D’Anastasio R (2017) Congenital anatomical variant of the clavicle. Anat Rec (Hoboken) 300:1401–1408
Author information
Authors and Affiliations
Contributions
AJ: data collection, data management, performing dissection, and writing manuscript. CMS: data collection and performing dissection. J-HL: project development, data analysis, performing dissection, and manuscript writing and editing. S-HH: project development and data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jeon, A., Seo, C.M., Lee, JH. et al. The distributed pattern of the neurovascular structures around clavicle to minimize structural injury in clinical field: anatomical study. Surg Radiol Anat 40, 1261–1265 (2018). https://doi.org/10.1007/s00276-018-2091-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-018-2091-4