Abstract
Purpose
Although the course of the ureter is described as a straight descent in the retroperitoneum, kinking of the upper ureter is often seen at imaging. The aim of this study was to investigate kinking of the ureter and its underlying anatomico-clinical significance.
Methods
We evaluated 176 computed tomography (CT) images and classified kinking into three grades: no/mild kinking as Grade 1, moderate as Grade 2, and severe as Grade 3. We defined the “crossing point” (CP) as where the ureter crosses over the gonadal vein and assessed its relation to the kinking. Fourteen halves from seven cadavers were used for examination. Approaching anteriorly, we macroscopically observed the ureter and surrounding structures.
Results
On CT, the rate of the radiologically “significant” kinking classified into either Grade 2 or 3 was 18.4 % on the right and 21.8 % on the left. All kinking was either at or above the level of the CP. In cadavers, the ureter was relatively mobile in the perirenal fat and then beginning at approximately the level of the CP became firmly fixed to the anteromedial aspect of the psoas major muscle.
Conclusions
Kinking of the upper ureter is not a clinically significant finding and arises from the ureter having a relatively mobile portion in the perirenal space compared to its caudal portion. The fixation boundary can be identified by observing the CP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is generally accepted that the ureter descends straight in the retroperitoneal space [1, 2]. However, on retrograde pyelography or computed tomography (CT) urography performed routinely in clinical practice, kinking of the upper ureter often occurs near its crossing over the ipsilateral gonadal vein (Fig. 1). Since kinking is sometimes very prominent, one might imagine that it could cause clinical problems, for example predisposing patients to ureteric stone obstruction at this location. Additionally, it could make endo-ureteric procedures difficult. However, to the best of our knowledge, there have been no descriptions in the literature that kinking here poses a problem, possibly for lack of clinical significance, or perhaps because this finding has heretofore been overlooked. Another question is why kinking is almost always seen at approximately the same level within the upper ureter. It has long been known that there are three physiologically narrow points in the upper urinary tract: the ureteropelvic junction (UPJ), the pelvic brim where ureter crosses over the common iliac vessels, and the ureterovesical junction [2, 5]. However, recent studies focusing on the location of ureteral stones using CT images revealed one of the most frequent levels where stones obstruct was actually in the upper ureter, the cause of which was not specifically mentioned [4, 7]. One might be able to speculate that there is some anatomical relationship between obstruction of stones and kinking, both of which occur in the upper ureter.
The aim of this study was to determine the prevalence, location, and degree of kinking seen in the upper ureter on CT urography and investigate its underlying anatomico-clinical significance by dissecting cadavers.
Materials and methods
CT urography
We retrospectively evaluated 176 consecutive patients (117 males and 59 female patients, mean age 64.2 years, range 21–92 years) who underwent enhanced abdominal CT including an excretory phase (CT urography) from April 2014 to March 2015 at our hospital. CT urography was performed for any of the following clinical purposes: investigation of hematuria (n = 95), investigation of suspected abnormality found on other diagnostic modalities such as ultrasound (n = 31), pre-treatment evaluation of bladder carcinoma (n = 24), follow-up examination after transurethral resection of bladder tumor (n = 23) or evaluation of the urinary tract as a recipient before kidney transplantation (n = 3). Exclusion criteria were as follows: congenital abnormality of the upper urinary tract such as duplicated renal pelvis and ureter or horse-shoe kidney, acquired abnormality of the upper urinary tract including neoplasm, a stone of the UPJ or the upper ureter, prior history of an open/laparoscopic surgery of the abdomen or pelvis, and other abnormalities around the upper ureter which could potentially affect the course of the ureter. This study was approved by the Institutional Review Board. Informed consent was waived because of the retrospective nature of the study.
For all patients, 2 mL/kg of intravenous non-ionic contrast material (iohexol, Ominipaque 300, Daiichi Pharmaceutical, Tokyo, Japan; iopamidol, Iopamiron 300, Bayer Healthcare, Osaka, Japan) was injected as a bolus. CT examinations were performed with either of two 64-detector CT scanners (Aquilion, TOHSHIBA, Japan and Optima CT660, GE, USA). The excretory phase scanning was acquired 6 min after completion of an injection of contrast. The CT parameters were as follows: tube voltage 120 kv, tube current 100–500 mA/s, collimation 32 mm, pitch 0.844, field of view 320 mm, matrix 512 × 512 for the Aquilion unit, tube voltage 120 kv, tube current 50–560 mA/s, collimation 40 mm, pitch 0.984, field of view 320 mm, matrix 512 × 512 for the Optima CT660 unit. The axial and coronal images were reconstructed at 1–1.25 and 2–3 mm slice thickness, respectively. Three-dimensional reconstructed images of the excretory phase (CT urography) were obtained using a three-dimensional workstation.
We classified kinking of the upper ureter into three grades (Fig. 2): no/mild kinking of the upper ureter (Grade 1), moderate kinking containing a horizontal portion (Grade 2), and severe kinking containing a retrograde portion (Grade 3). That is, either being classified into Grade 2 or 3 was regarded as radiologically “significant” kinking. As shown in Fig. 2, we measured the width of the kinking in Grade 2 and the width and the height in Grade 3 using the coronal view. Next, we named the point where the ureter crosses over the ipsilateral gonadal vein as the “crossing point” (CP) and measured the vertebral level of each CP. As shown in Fig. 3, we divided each vertebra into thirds and numbered lower third of L2 vertebra to lower third of L5 as 1–10 and analyzed each location. The location of the kinking in relation to the CP was also analyzed.
All CT exams were reviewed by two board-certified radiologists (MK and TN) with 8 and 13 years of experience, respectively.
Cadaveric study
Fourteen halves from seven cadavers (two males and five females, all of Japanese ancestry, mean age at the time of death 85.4 years; range 56–97 years) were used for the dissecting examination. All cadavers were donated to the Department of Anatomy of Tokyo Medical and Dental University. Cadavers were fixed in 8 % formalin and preserved in 30 % ethanol.
To examine the ureter, we removed the skin, the subcutaneous tissues and the alimentary tract from the body. Then we approached the retroperitoneal space from the anterior side and macroscopically observed the position of the ureter and its vascular and nervous distribution. We also visualized the gonadal vein and evaluated its relation to the ureter.
Statistical analysis
According to a power analysis based on a Chi-square goodness of fit test model from a prior study [3], this sample size (n = 176) yielded 100 % power at the significance level of 0.05 for medium size effect. The Chi-square test was performed to assess laterality in the grade of kinking seen in the upper ureter. The paired t test was used to compare the vertebral level of the CP by side and one-way ANOVA was used to compare the vertebral levels of the CP among kinking grades bilaterally. All statistical analyses were performed using R for Windows software (R Development Core Team, version 3.0.2; Vienna, Austria). The level of significance for all calculations was defined at p < 0.05.
Results
CT urography
Of 176 cases, 2 right ureters and 2 left ureters were not evaluated because of difficulty in identifying the ureter or the gonadal vein. Kinking of the upper ureter on the right was seen in 142 cases as Grade 1 (81.6 %), 17 cases as Grade 2 (9.8 %) and 15 cases as Grade 3 (8.6 %). On the left, it was seen in 137 cases as Grade 1 (78. 2 %), 26 cases as Grade 2 (15.5 %) and 11 cases as Grade 3 (6.3 %) (Fig. 4a–c). The findings are summarized in Table 1. The rate of the radiologically “significant” kinking classified into either Grade 2 or 3 was 18.4 % on the right and 21.8 % on the left. There was no laterality in the grade of kinking (p = 0.22). All kinking was seen either at the same vertebral level or above the level of the CP. In Grade 2 kinking, mean width of the kinking was 13 mm (range 3–25 mm) on the right side and 14 mm (range 7–32 mm) on the left side. In Grade 3 kinking, mean width was 11 mm (range 6–20 mm) and mean height was 8.7 mm (range 3–15 mm) on the right side, mean width was 18 mm (6–28) and mean height was 9.5 mm (range 4–20 mm) on the left side. The average level of the CP was 6.4 (middle third of L4 vertebra) on the right side and 5.1 (upper third of L4 vertebra) on the left side. The CP was significantly lower in the right side (p < 0.01) (Fig. 5). On the other hand, there was no significant difference of the vertebral level of the CP by kinking grade on either side (p = 0.78 on the right, p = 0.42 on the left).
Three-dimensional reconstructed images of CT urography. a No kinking of the left upper ureter in a 65-year-old man classified into Grade 1. b Moderate kinking of the left upper ureter in a 48-year-old female classified into Grade 2. c Severe kinking of the left upper ureter in a 58-year-old man classified into Grade 3. Kn kidney, Ur ureter, GV gonadal vein, L3 third lumbar vertebra, L4 fourth lumbar vertebra
Cadaveric study
By removing the peritoneum and the anterior renal fascia, the ureter and the gonadal vessels were visualized. After passing through in the perirenal fat where the ureter was relatively mobile, the ureter was fixed firmly to the medial anterior aspect of the fascia of the psoas major muscle. The upper border of the firm fixation was approximately where the gonadal vein crosses over the ureter (Fig. 6). The ureter had a scarce supply of the vessels and nerves at this relatively fixed area (Fig. 6d, area of asterisk). No direct vessel or nervous distribution was found at the medial side in this area. Above the firmly fixed area, the ureter had arterial and nervous supply from the renal hilum and venous drainage to the renal vein to IVC near the renal hilum. Below the firmly fixed area, it was supplied from or drained by the ipsilateral iliac vessels. No cadaveric specimen demonstrated significant kinking.
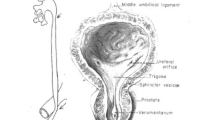
The ureter and its surrounding structures in the cadaver. a The anterior renal fascia was exposed after removal of the peritoneum. b The gonadal artery and vein were revealed beneath the peritoneum. c The ureter was observed beneath the layer of the gonadal vessels. d After passing through in the perirenal fat, the ureter was fixed firmly to the medial aspect of the fascia of the psoas major muscle (area of asterisk). The area of the ureter had a scarce supply of the vessels and nerves. RF renal fascia, Pr peritoneum, GA gonadal artery, GV gonadal vein, PM psoas major muscle, IVC inferior vena cava, Ao aorta, Ur ureter, CIA common iliac artery, Kn kidney, RV renal vein, RA renal artery, IIA internal iliac artery, EIA external iliac artery
Discussion
The ureters are a pair of long cylindrical structures in the retroperitoneal space which connect the kidney and the bladder. The ureteral length is 25–30 cm in adult [6]. While the bladder is to some extent fixed to the pelvis, the kidney is located just under the diaphragm and changes its position dramatically according to physiological movement such as respiration [5, 13]. Its position can be also changed under degenerative change of the lumbar vertebra or weakening of supporting tissues around it. These reversible or irreversible changes of the kidney position always force the ureter to adjust its length.
Intravenous pyelography (IVP) has been long used to assess the ureter. CT urography, however, has recently largely replaced this exam and plays a major role in evaluating urinary tract owing to its availability to provide more detail using multi-planar reconstructed images [9, 12]. One of the differences between these examinations lies in the timing of imaging. In IVP, images are taken in the expiratory phase, while in CT urography, images are usually taken in the inspiratory phase just like other abdominal CT examinations. That is, the images of CT urography are taken in a condition when the kidney descends. Routine observation of the urinary tract in the inspiratory phase is therefore a relatively recent phenomenon.
In this CT urography study, we found kinking in the upper ureter to be common; additionally, it always occurs at or just above the level where the ureter crosses over the ipsilateral gonadal vein. In cadavers, the ureter was relatively mobile as it passed through the perirenal fat and then became fixed firmly to the anterior medial side of the psoas major muscle. The level of the ureter’s fixation was approximately where it crossed over the gonadal vein.
Considering these results together, we speculate that the kinking probably arises as a consequence of the ureter adjusting length when the kidney descends. This hypothesis is also supported by observing dynamic images of the upper ureter during angiography or retrograde pyelography, in which dynamic change of the upper ureter synced to the movement of the kidney is well visualized (Fig. 7). It is thought that kinking is seen at the area where the ureter is relatively mobile, that is, where it runs in the perirenal space. The boundary of the perirenal portion of the ureter can be determined approximately by finding the level of the CP (Fig. 8). From an embryo-anatomical point of view, it is not clear why the CP is associated with fixation of the ureter; after passing through the perirenal space, both the ureter and the gonadal vein are sandwiched between the anterior renal fascia and the posterior renal fascia on the medial side in the retroperitoneal space. Both structures run cranio-caudally in the space and have to cross eventually from the renal hilum to the pelvis. The CP turns out to be at a very practical landmark: the boundary where the ureter exits the perirenal space and is fixed more firmly in the anterior medial aspect of the psoas muscle.
Dynamic images of the ureter during angiography. A 38-year-old female with atonic uterine bleeding. During angiography (uterine artery embolization), dynamic changes of the upper ureter in synchrony with the movement of the kidney is well visualized. The kinking is most prominent in the inspiratory phase and mild in the expiratory phase. Ur ureter, L3 third lumbar vertebra, L4 fourth lumbar vertebra, Catheter catheters in the right internal iliac artery
Mechanism of causing kinking. Kinking arises as a consequence of the ureter adjusting length when the kidney descends. Kinking is seen at the area where the ureter is relatively mobile, that is, where it runs in the perirenal space. The boundary of the perirenal portion of the ureter can be determined approximately by finding the level of the CP. Kn kidney, IVC inferior vena cava, Ao aorta, GA gonadal artery, GV gonadal vein, PM psoas major muscle, Ur ureter
Ureteral kinking did not show laterality in this study. On the other hand, the level of the CP was slightly lower on the right side. This can be explained by the fact that kidney is located lower on the right side because of the liver being just above the right kidney [5, 10, 13]. Fixation of the upper ureter is also probably slightly lower on the right side. The vertebral level of the CP was not significantly different with respect to the grade of the kinking. Thus, it does not appear that kinking is caused by a higher/lower positioning of the point of fixation.
Although most radiologists or urologists who read CT urography regularly in their daily practice are very familiar with kinking of the upper ureter, there have been very few reports focusing on this finding. Indeed, one anatomical text states, “in its abdominal portion the ureter pursues an almost vertical course downward and medially on the anterior surface of the psoas muscle” [1]. Additionally, Silverman et al. published a “normal” three-dimensional urography CT image in which grade 3 kinking was seen on the right side, an example of how this finding had been ignored thus far [11]. On the other hand, Motola et al. mentioned “the proximal ureter is easily visible endoscopically as the variations of kidney position with breathing cause movement of this area secondary to its fixed, non-mobile nature compared with the mobile renal pelvis…,” and “…a bend of mucosa” is noticed around UPJ junction endoscopically [8]. This “bend” may be coincident with the kinking in our study. In our cadaveric study, on the other hand, none of the specimens demonstrated significant kinking. Since cadavers fixed in formalin assume an expiratory configuration because of muscular laxity, the kidney tends to be positioned cranially and the ureteral kinking is therefore absent. Thus, we hypothesize that this is one of the main reasons ureteral kinking has not been previously noted.
So, what, if any, relationship does the area where kinking arises have to clinical problems of the ureter? While the previously mentioned, well-known tendency for obstruction at the UPJ is helpful in theory, in daily practice we often encounter cases in which a stone obstructs at the upper ureter, slightly distal to the UPJ where the caliber change occurs (Fig. 9). Recent studies investigating the distribution of ureteral stone location using multi-planar CT images also mentioned that one of the most common levels of ureteral stone obstruction is in the upper ureter [4, 7]. Although the cause of this obstruction was not described in detail in these articles, it would be difficult to imagine that the diameter of the ureter is the sole cause. We speculate that this area of the upper ureter would likely be near the CP where the ureter is fixed more firmly in the retroperitoneal space and just below where kinking is observed. Some stone obstructions do occur at the UPJ, the physiological area of narrowing near the renal hilum, but these stones tend to be quite large. Smaller stones tend to obstruct in the proximal upper ureter near the CP at the border of the mobile and fixed portions of the ureter. We also speculate that these two separate sites have been quite often lumped together in the clinical setting. We believe the definition of the UPJ needs to be rethought and the newly recognized area of potential obstruction in the upper ureter around the CP might be acknowledged.
A coronal reconstructed image of non-enhanced abdominal CT. A 42-year-old male presented at our emergency department for a sudden onset of right back pain. Non-enhanced CT revealed a small calcified stone (arrow) stuck in the upper ureter around the level of CP. Kn kidney, GV gonadal vein, Ur ureter, IVC inferior vena cava, Ao aorta, PM psoas major muscle, IM iliac muscle
This study has several limitations. First, examinations of CT urography we assessed were not obtained from normal subjects but rather from patients who have or who likely have some disorders of the urinary tract. Second, the ureter can change its shape dynamically with respiration or other normal physiological movements and it also has peristaltic activity to convey urine to the bladder. The images of CT urography are static, only a snapshot of the ureter at one point in time, and the entire dynamic movement cannot be evaluated. Finally, we did not actually evaluate the locations of stone obstructions in the current study, just the gross anatomic and imaging appearances. Further investigation is needed.
Conclusion
Kinking of the upper ureter is not a clinically significant finding, which is often seen in CT urography. This finding can arise due to the fact that the upper ureter passing through the perirenal space has more mobility compared to its caudal portion which is more firmly fixed in the retroperitoneal space. This boundary can be identified by observing CP where the ureter crosses over the ipsilateral gonadal vein.
References
Arson BJ, McVay CB (1984) Surgical anatomy, 6th edn. W.B. Saunders Company, Philadelphia
Borley N (2008) Gray’s anatomy, 40th edn. Elsevier, London
Cohen J (1992) A power primer. Psychol Bull 112(1):155–159. doi:10.1037/0033-2909.112.1.155
Eisner BH, Reese A, Sheth S, Stoller ML (2009) Ureteral stone location at emergency room presentation with colic. J Urol 182:165–168. doi:10.1016/j.juro.2009.02.131
El-Galley RE, Keane TE (2000) Embryology, anatomy and surgical applications of the kidney and ureter. Surg Clin N Am 80(1):381–401
Fröber R (2007) Surgical anatomy of the ureter. BJU Int 100:949–965. doi:10.111/j.1464-410X.2007.07207.x
Moon YJ, Kim HW, Kim JB, Kim HJ, Chang YS (2015) Distribution of ureteral stones and factors affecting their location and expulsion in patients with renal colic. Korean J Urol 56:717–721. doi:10.4111/kju.2015.56.10.717
Motola JA, Shahon RS, Smith AD (1988) Anatomy of the ureter. Urol Clin N Am 15(3):295–299
Potenta SE, D’Agostino R, Sternberg KM, Tatsumi K, Perusse K (2015) CT urography for evaluation of the ureter. Radiographics 35(3):709–726. doi:10.1148/rg.201514029
Resnick MI, Pounds DM, Boyce WH (1981) Surgical anatomy of the human kidney and its applications. Urology 17:367
Silverman SG, Leyendecker JR, Amis ES Jr (2009) What is the current role of urography and MR urography in the evaluation of the urinary tract. Radiology 250(2):309–323. doi:10.1148/radiol.250208534
Van Der Molen AJ, Cowan NC, Muller-Lisse UG, Nolte-Ernsting CA, Takahashi S, Cohan RH, CT Urography Working Group of the European Society of Urogenital Radiology (ESUR) (2008) CT urography: definition, indications and techniques. A guideline for clinical practice. Eur Radiol 18:4–17. doi:10.1007/s00300-007-0792-x
Wood D, Greenwell T (2008) Surgical anatomy of the kidney and ureters. Surgery 26(4):133–135
Acknowledgments
The authors are grateful to Jay Starkey, M.D. for the revision of the English text, and Daisuke Unai, R.T. for the assistance of creating the CT images. This work is supprted by JSPS KAKENHI Grant Number 15K08129.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Kamo, M., Nozaki, T., Yoshida, K. et al. Kinking of the upper ureter in CT urography: anatomic and clinical significance. Surg Radiol Anat 38, 1115–1121 (2016). https://doi.org/10.1007/s00276-016-1689-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-016-1689-7