Abstract
The sphenoid sinus, one of the posterior groups of sinuses, has long been regarded as a ‘neglected sinus’ due to the anatomical location, poor understanding and poor accessibility, till the advent of endoscopes and modern imaging techniques. Increasing knowledge and greater understanding of this sinus has permitted an evolution in surgical practices and boundaries. Various literatures of the past report a great variety of rates of pneumatization, rates of optic nerve protrusion and dehiscence, as well as internal carotid artery (ICA) protrusion and dehiscence. One similarity noted among these studies is that the rates vary according to the ethnicity of the patients. Recommendations have also been made along the way with regard to modified surgical techniques. This review aims to describe the pneumatization of sphenoid sinus and the topographical relation of the optic nerve and ICA in different populations.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The sphenoid sinus was once regarded as the difficult sinus to approach due to its deep anatomical location, limited knowledge on it, as well as the complexity of the structures surrounding it. To make things harder, there are some diseases, for example, ascending nasopharyngeal lesions, descending intracranial lesions, mucocele, cholesterol granuloma and neoplasms, that may destroy the walls of the sphenoid sinus, that in turn could distort the delicate anatomy of the sinus and its surrounding structures [16, 33, 56]. The sphenoid sinus is surrounded by neurovascular structures; being the internal carotid artery (ICA), optic nerve (ON), maxillary nerve and vidian nerve.
The advent of functional endoscopic sinus surgery (FESS) and modern imaging techniques have allowed this sinus to be approached more often not only to treat diseases within it, but also as a route to the pituitary gland. In view of the excellent minimally invasive surgical access and advancements in endoscopic techniques, the sphenoid sinus in turn can be used as a path to approach tumors involving the anterior skull base, parasellar region, clivus, petroclival region and the cavernous sinus [25, 32, 44]. Resection of tumors such as chordomas, meningiomas, chondrosarcomas and esthesioneuroblastomas via this approach has shown promising results with lesser rates of complications, morbidity and mortality [25, 32, 44, 70, 76].
The diagnosis of a pathology within a sinus is established based on clinical grounds with the aid of an endoscopic examination. Nasal endoscopy unfortunately is not without its limitations as deeper structures are often not assessable. Imaging of the paranasal sinuses with computed tomography (CT) scan has beyond doubt an established role in reaffirming the diagnosis, as well as in the management of the diseases [ 6, 7, 9]. Hence, CT scan and endoscopy complement each other [68] and make for a full evaluation of the patient and the disease state.
One point worthy to note is that CT scans are conventionally used as the first choice of imaging modality for uncomplicated sphenoid sinus pathology as it is inexpensive and easily available as well as accessible at many centers. However, a magnetic resonance imaging (MRI) scan is a mandatory second choice when dealing with complicated sphenoid sinus lesion, especially in diseases with intracranial extension, as the MRI gives superior information in terms of soft tissue delineation.
Multiple CT scan studies that highlight their findings in terms of the variations of the anatomical structures, emphasize the wide range of the sphenoid sinus anatomical structure variants, and the importance of identifying them in a specific population. These variations have a major significance on the surgical access as well as the potential complications that can arise from them [10, 35]. This review describes the varying rates of sphenoid sinus pneumatization and its significance, optic nerve dehiscence and protrusion as well as ICA dehiscence and protrusion in different populations. We also briefly describe the role of CT imaging in sphenoid sinus disease.
Method
Materials for this review were searched on electronic databases, namely, Pubmed and SCOPUS. MEDLINE records which are produced by the National Library of Medicine (NLM) in EMBASE were scrutinized as well. Some articles were identified from the experience and information provided by the senior authors. Further relevant articles that were pertinent to this review were identified by reviewing the references of articles that had been retrieved. The following keywords were used either individually or in combination; sinus; sphenoid; anatomy; optic nerve; carotid artery; endoscopic sinus surgery; transsphenoidal; variants; paranasal sinus AND CT scan; sphenoid sinus AND pneumatization. Certain information on the anatomical aspects provided in the articles were counter checked and compared with standard textbook information. The search was conducted intermittently over a period of 10 months, between February 2012 and November 2012. The necessary articles that were thought to be relevant which consisted mostly of original research work, were identified from the 102 articles retrieved.
Anatomy of the sphenoid sinus
The sphenoid sinuses are a pair which lie within the body of the sphenoid bone. The structures lying in a close relationship to the sinus are the blood vessels and nerves which travel alongside the sinus on their way to or from the cranial fossa [74]. The right and left sinuses are separated by a septum which is commonly skewed to one side and not necessarily located in the midline. Deviation of the septum towards one side would lead to the inequality of the sizes of the sinus and the larger one usually being referred to as the ‘dominant’ sinus. The average volume of the sinus ranges between 3.0 and 10.0 ml [60]. An average well-formed adult sphenoid sinus measures 20 mm in height, 23 mm in depth and 17 mm in width [74]. A small sinus lies in front of the pituitary fossa [54], and when large, it may extend into the greater wing of the sphenoid and the pterygoid process [64].
Superiorly, the sphenoid sinus is related to the pituitary fossa and the middle cranial fossa, laterally to the cavernous sinus and its contents, posteriorly to the posterior cranial fossa, clivus, brain stem and basilar part of occipital bone, and inferiorly the roof of the nasopharynx [40, 45, 64]. The sinuses are in approximation to the optic nerve superolaterally, ICA posterolaterally [64] and maxillary and vidian nerve inferiorly. The carotico-optic recess is a small depression that separates the carotid artery and the optic nerve.
Pneumatization
At birth, the sphenoid bone contains only erythropoietic marrow [61]. The red erythropoietic marrow is converted to yellow marrow in the presphenoidal plate between the ages of 7 months and 2 years [4]. Marrow conversion then subsequently extends posteriorly into the basisphenoid plate [61].
Pneumatization progresses in an inferior posterolateral direction. The pneumatized basisphenoid plate often extends to the spheno-occipital synchondrosis in the mature sphenoidal sinus, however it does not pass beyond this synchondrosis [61]. Pneumatization may extend into the anterior clinoid process or greater wing of sphenoid. The sphenoid sinus usually attains its mature size by the age of 14 [30]. High-resolution CT may show pneumatization of the sphenoidal sinuses as early as 2 years [61].
Surgical access to the sella, and the state of the surrounding neurovascular structures, are determined and affected by the rate and pattern of pneumatization. A sphenoid sinus that is highly pneumatized may cause anatomical distortion, therefore caution must be exercised during sellar opening to avoid damaging the optic nerve or carotid artery [35, 62, 63].
The extent of surgery is often determined by the extent of sphenoid sinus pneumatization, which occasionally could be very extensive and involving adjacent structures [15, 57, 69]. This was probably one of the reasons as to why Wang J et al. [75] had proposed a reclassification of sphenoid sinus pneumatization when planning for skull base surgery. This paper had proposed that the sellar type of pneumatization could be further classified into six types based on the pneumatization direction. These were sphenoid body, lateral, clival, lesser wing, anterior, and combined [75].
However, the conventional and widely accepted Hammer and Radberg [36] classification is used in most practices till today. It describes sphenoid sinus pneumatization as conchal, presellar and sellar types, based on pneumatization around the sella turcica [18, 29, 35, 36, 50, 71]. In the conchal type, pneumatization is absent, the sphenoid sinus is filled by cancellous bone, and there is no association with the sella turcica. In the presellar type, the sinus cavity remains anterior to a vertical line drawn through the tuberculum sellae. Whereas in the sellar type, sinus pneumatization extends beyond a vertical line drawn through the tuberculum sellae, and this type is related to the floor and anterior wall of the sella turcica. The various patterns of pneumatization are illustrated in Fig. 1a–c, respectively.
a Presellar type of pneumatization, b sellar type of pneumatization, c conchal pneumatization (ST sella turcica) line X vertical line drawn through tuberculum sellae, presellar type: pneumatization remains anterior to line X, sellar type: pneumatization extends beyond line X, conchal type: filled with bone. Figures a–c illustrating the types of pneumatization pattern
We would be remiss in our duty if we do not mention sphenoid sinus agenesis, a very rare entity. Sphenoid sinus agenesis is defined as complete lack of pneumatization of the body of the sphenoid bone [14]. Its incidence has been reported at 0.67 % by Sonbay et al. [66] and even lower at 0.26 % by Cakur et al. [14]. This condition is usually associated with craniofacial syndromes or primary ciliary dyskinesia [58] although occasionally it may be an isolated incident [42, 66].
Madiha et al. [50] in 2007, reported 76 % of presellar type and the rest sellar pneumatization, in 25 Egyptian sinuses consisting of patients and cadavers. Conchal type was not encountered in this study. In contrast, in Tan et al.’s [71] Asian cadaveric study, the sellar type was the commonest at 55 %, and the least commonest was presellar at 17 %. The sellar type was the predominant type with 90 %, followed by presellar type at 9 % and conchal at 1 % in 100 Korean cadaveric heads examined by Cho et al. [18]. There appears to be a difference in the main type of pneumatization with regard to ethnicity, i.e., the sellar type of pneumatization seems to be commoner in Asians. This highlights the importance of studying the patterns of pneumatization in a local population as the type of pneumatization in turn could affect the outcome of surgical access.
The sphenoid sinus ostia and the intersphenoid septum
The sphenoid sinus ostia is located on the anterior wall of the sinus and opens into the spheno-ethmoidal recess. It may be round or oval in shape. Madiha et al. [50] reported 58 % of the 50 ostias in their 25 cadaveric dissections to be oval in shape, and the remainder round. 68 % of the ostia was more than 4 mm in size, whereas the balance were less than 4 mm in size.
The sphenoid sinus ostium can be located and visualized on the medial aspect of the superior turbinate, and this has been considered to be one of the most constant and reliable landmark for endoscopic sinus surgery. Having said that, the vertical, horizontal and oblique distances of the sphenoid ostium from various points serve as good guides to access the ostium during sinus surgery. The vertical distance from the roof of the posterior choanae is a well-described landmark to access the ostia of the sinus. In a study published by Hidir et al. [39], the vertical height of the sphenoid ostium from the roof of the choanae ranged between 5.7 and 21.5 mm with an average of 10.9 mm [39], and Abuzayed et al. [2] reported the vertical height from the posterior choanae to the ostia to be 15 mm in their study on Turkish patients.
The ostia was found to be located at an average of 2.2 cm from the anterior end of the superior turbinate [60]. The superior turbinate has been noted to be a reliable and consistent horizontal landmark for localizing the ostia of the sphenoid sinus, be it the anterior end or the posterior end [12, 60]. The ostia can be localized within 1 cm of the posterior inferior edge of the superior turbinate, and between 1.5 and 3 cm above the superolateral angle of the posterior choana [34].
Most studies report the sphenoid ostia to be located on the middle portion of the anterior wall of the sinus [39, 43]. The anterior nasal spine and the limen nasi have been used as landmarks to measure the distance of the ostia. The anterior nasal spine has been mentioned as a reference point by Davis et al. [21] and Turgut et al. [72]. Gupta et al. [34] reported the distance of the ostia as 55 mm from the limen nasi. It is interesting to note that all these different landmarks described by different authors vary not only between the studies, but also between the respective population.
The intersphenoid septae may occur as a single septum or be present in multiples, for Elwany et al. [28] found 73 % of their sinuses had multiple septae. 80 % of the intersphenoid septae in Sareen et al.’s work [60] was also multiple in nature. This implies that the septum may not exactly be a reliable guide for approaching the midline in endoscopic sinus surgery.
Although the intersphenoid septae separates the right from the left sphenoid sinus, the septum is often deviated to the right or left side, and only occasionally be found in the midline. It has been found that only one in four septums are located in the midline [3, 28]. 16.6 % of the septae were in the midline and 56.3 % were found to be deviated to the left and the remainder inclined towards the right side in the 48 Asian cadaveric heads examined by Tan et al. [71]. In 25 Turkish sinuses examined by Madiha et al. [50], five septaes were deviated to the left, 15 to the right and the remainder five were located in the midline.
The intersphenoid septum may occasionally be deflected to one side attaching to the bony wall covering the optic nerve and/or the ICA, and can be injured when the septum is avulsed during sinus surgery [19]. Hence, it is important to determine the location of the septum and if it is attached to the wall overlying the carotid artery or optic nerve prior to embarking on surgery.
Optic nerve: the anatomy
In clinical context, the optic nerve can be divided into four segments in order, namely the intraocular segment, intraorbital segment, intracanalicular segment and finally the intracranial segment. The shortest segment measuring about 1 mm in length is the intraocular segment, whereas the intraorbital segment is the longest segment, measuring 3 cm in length. The intracanalicular segment, which is enclosed by dura runs along the optic canal.
The intracranial segment, which is the most variable segment of all, based on the position of the optic chiasm, lies medial to the ICA. This segment courses on the superolateral wall of the the sphenoid sinus [11]. The nerve travels medially till the nasal fibers decussate at the optic chiasm, which in turn lies on the tuberculum sellae.
In its course, the optic nerve is the least nourished in its optic canal. It is at this area that it is the most susceptible to injury via direct inflammation of the sinus disease [11]. If the sphenoid sinus is accessed by opening the anterior and posterior ethmoids, it is advocated to stay as medially and inferiorly as possible to avoid optic nerve penetration and injury [67].
Optic nerve: dehiscence and protrusion
The dehiscence and protrusion of the neurovascular structures are closely associated with the extent of sphenoid sinus pneumatization [18]. Occasionally, when the anterior clinoid process is pneumatized, the optic nerve may then traverse the sinus. The nerve may be covered by a thin layer of bone of 0.5 mm or less in thickness, or may even be totally absent, in which case it is noted as being dehiscent.
An optic nerve bony dehiscence of 4 % was reported by Fuji et al. [30]. Except for Heiwaidi et al. [37] who reported optic nerve dehiscence at the rate of 30 %, generally most studies report a low rate of optic nerve dehiscence, ranging from 0.7 to 8 % [41, 54, 73] (Table 1). In most of the studies, optic nerve dehiscence was defined as absence of the bony wall overlying the optic nerve [24], although some studies mention in terms of thickness of the separating bony wall.
Optic nerve injury resulting in blindness is a potential undesirable complication of endoscopic sinus surgery, especially when operating on the sphenoid sinus [55]. Axial view CT scans are essential in the assessment of the posterior ethmoidal cells in relation to the optic nerve [11]. The optic nerve is at greater risk of injury with the presence of Onodi cells [27].
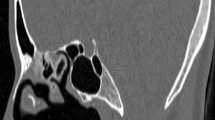
Delano et al. [23] outlined a classification used to describe the association and relationship between the sphenoid sinus, posterior ethmoid sinus and the optic nerve. The optic nerve was categorized as Type 1 when it was found to be lying adjacent to the superior and lateral walls of the sphenoid sinus. They were considered to be Type 2 when the optic nerve was found to make an indentation on the sphenoid sinus. Type 3 classification was given to optic nerves that traversed the sphenoid sinus and in Type 4, the optic nerves were adjacent to the sphenoid and posterior ethmoid sinus and covered by aerated cells [23]. All the Type 3 nerves and 82 % of Type 2 nerves were noted to be exposed without a bony covering [59]. The illustrations in Fig. 2a–d demonstrate the optic nerve variations.
a Type 1 variation: optic nerve lies adjacent to the superior and lateral walls of the sphenoid sinus, b Type 2 variation: optic nerve makes an indentation on the sphenoid sinus, c Type 3 variation: optic nerve traverses the sphenoid sinus and makes a deeper indentation, d Type 4 variation: optic nerve is adjacent to the sphenoid sinus and covered by aerated cells. Figures a–d demonstrating the variations of the optic nerve with respect to its relationship to the sphenoid sinus (optic nerve marked in blue) (color figure online)
Protrusion of the optic nerve in most studies was defined as a bulging of the optic canal into the sphenoid sinus cavity so as to cause exposure of more than half of the circumference of the nerve, with or without defects in the bony margins [24, 65, 73]. The risk of optic nerve injury during surgery was noted to be raised when 50 % or more of the nerve circumference was exposed [24]. Siricki et al. [65] and Unal et al. [73] reported optic nerve protrusion into the sphenoid sinus in Turkish patients at the rate of 31 % each, which is equivalent to one in three patients having optic nerve protrusion (Table 1). Whereas, Tan et al. [71] reported a remarkably high rate of 69 % optic nerve protrusion in the Asian counterparts.
However, a point to ponder here is whether the rates of protrusion could be different in the various population due to their true incidences or due to the difference in definition. The dilemma here is that there is no fixed definition or criteria for the protrusion of optic nerve. Unal et al. [73] in their study defined protrusion as a finding for placement of a neural or vascular structure with more than 50 % of its diameter in sphenoid sinus, whereas Tan et al.[71] had not specified a definition for optic nerve protrusion in their study.
Internal carotid artery: the anatomy
The ICA may be categorized into four segments as per the recommendation of Terminologia Anatomica (1998), which is an official anatomical nomenclature body. The four segments are cervical, petrous, cavernous and cerebral. It essentially segregates the components of the artery as it courses from the point of bifurcation to its terminal branches. The cervical segment begins at the point of bifurcation up to the point of entering the carotid canal, as described earlier.
Once the artery enters the carotid canal, it curves laterally into the foramen lacerum and from this foramen, it curves upwards to enter the posterior part of the cavernous sinus. This segment is termed the petrous segment. Within the cavernous sinus, which makes up the cavernous segment, the artery runs forward and deeply grooves the body of the sphenoid and base of its greater wing. It then curves upwards, pierces the roof of the cavernous sinus medial to the anterior clinoid process and curves immediately backwards to lie on the roof of the cavernous sinus.
Upon exiting the cavernous sinus, the artery makes up the cerebral segment. It subsequently curves upwards lateral to the optic chiasm, and finally reaches the anterior perforated substance where it gives off its terminal branches. Each of the right and left internal carotid arteries ultimately divide into the anterior and middle cerebral arteries to supply the cerebral cortex [64]. Besides the main branches, it also gives off the striate arteries, posterior communicating artery and the anterior choroidal artery.
Another classification, the Bouthillier classification of ICA segments describes a seven-segment classification, i.e., the cervical segment, petrous segment, lacerum segment, cavernous segment, clinoid segment, ophthalmic (supraclinoid) segment and the communicating (terminal) segment [13]. This classification is commonly used by radiologists and neurosurgeons as its segmental course is well appreciated on angiography. Regardless of the classification used to describe the course of the ICA, a minor injury to any part can result in dire consequences as it is the branch of a main artery from the heart.
Internal carotid artery: dehiscence and protrusion
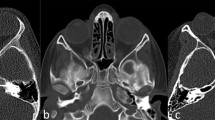
An ICA that is bulging into the sphenoid sinus or dehiscent in its bony wall, is vulnerable and exposed to the high risk of injury during endoscopic surgery. An injured artery would result in profuse bleeding and subsequently obscure the surgical field. In such a situation, it would not only be difficult to operate but it would also be an uphill task to identify and secure the bleeder. Figure 3a–c illustrates the variability of the ICA in relation to the sphenoid sinus.
a Normal bony covering of the internal carotid artery at the lateral wall of sphenoid sinus, b protrusion of the internal carotid artery on the lateral wall of the sphenoid sinus, c dehiscence of bony wall overlying the internal carotid artery. Figures a–c depicting the various relationships of the internal carotid artery to the sphenoid sinus wall
The ICA traverses posterolaterally in relation to the sphenoid sinus wall [11]. The ICA may protrude into the sphenoid sinus, especially so in a well-pneumatized or an over-pneumatized sinus [65]. A dehiscence of the bony covering over the ICA may result in full exposure of the artery within the sinus. It is in this situation that axial CT images are helpful in detecting this dehiscence [11].
Dehiscence of the ICA is defined as the absence of the bony wall separating the ICA from the sphenoid sinus as described by Siricki et al. [65], Sapci et al. [59] and Davoodi et al. [22]. The two main studies that quote a high rate of ICA dehiscence are by Heiwaidi et al. [37] and Siricki et al. [65], which are 30 and 22 %, respectively. Otherwise, generally the rate of carotid artery dehiscence is low at about 5 % [54, 73], and reported to be lower at 1.5 % by Kazkayasi et al. [41].
Internal carotid artery protrusion is defined as presence of more than half of the diameter of the vessel into the sphenoid structure [73]. Two studies on carotid artery protrusion based on CT scans by Meloni [54] on Caucasian patients and Heiwaidi [37] on Libyan patients had reported a rate of 67 and 41 %, respectively, which are indeed high.
The rate was similarly high at 67 % in Asian cadavers as reported by Tan et al. [71], as compared to Siricki’s [65] 26.1 % and Unal’s [73] 30.3 % of CT scan evaluation in Turkish patients. Arslan’s [5] study on Turkish patients based on 200 CT scans on the other hand reported a mere 8 % carotid artery protrusion rate. Generally, the studies done on the Asian patients quote a relatively high rate of ICA protrusion as compared to their Turkish counterparts. These widely variable figures cannot re-emphasize further the importance of determining the respective rates in a local population.
Role of computed tomographic (CT) imaging
The endoscopic transnasal transsphenoidal method of operating on the pituitary gland has become an accepted, minimally invasive excellent approach. Performed in the appropriate and careful manner, undesirable potential complications such as carotid artery injuries, hypothalamic injuries, loss of vision, meningitis and cerebrospinal fluid fistulas [8, 20, 48] can be avoided. Complications of transsphenoidal surgery may lead to mortality with an incidence rate of less than 1 % [20, 46]. These complications can be reduced by better understanding of the anatomy involved, as well as proper pre-operative planning which is where imaging comes into the picture.
The relevant structures may be visualized on CT scan which is ordered prior to endoscopic sinus surgery, especially when addressing the sphenoid sinus. All the paranasal sinuses from the frontal sinus anteriorly to the sphenoid sinus posteriorly are visualized on the CT images. The information gained from a CT scan is invaluable in managing disease recurrence, a recalcitrant disease, in post-surgical monitoring, as well as in cases where there is a diagnostic dilemma. It goes without saying that a pre-operative CT scan is mandatory before embarking on FESS, what more with the advent of high-resolution, multiplanar, multislice scanners [1, 24, 38].
Although MRI may be superior in terms of soft tissue delineation [47], the limited resources and the higher cost seldom make it the first choice of investigation. It is usually reserved for complicated cases. CT scans have proven to be vital, and most often than not, to be sufficient in imaging of the paranasal sinuses. The CT provides excellent contrast as well as sinonasal anatomical details [19, 49, 53].
Computed tomography scans not only demonstrate the anatomical variants of the structure of interest [49], but it also shows the nature and extent of the pathology, the aggressiveness of the disease state, conditions of the surrounding structures and involvement of vital structures[52]. The anatomical variations of the sphenoid sinus have major impact on the surgical access and the possibility of complications [35]. Pre-operative planning with CT scan prior to FESS not only prepares the surgeon for the surgery, but also significantly reduces the risk of potential complications for the patient[51].
Multiple cadaveric studies have been done to assess the anatomy of the sphenoid sinus. At the same time, reports on CT evaluation of the sphenoid sinus and its anatomical variants have been reported. The data gathered from cadaveric dissections concur and are similar to CT scan findings [5, 54]. Hence, it could be extrapolated that information and findings interpreted on the CT images can be expected to be encountered during surgery at their respective sites. The role of the CT scan in terms of a reliable non-invasive assessment tool of the anatomical structures is once again re-emphasized.
The sphenoid sinuses are the most inaccessible paranasal sinuses and are surrounded by significant anatomical structures being the optic nerve, ICA, maxillary nerve, Vidian nerve, orbit and its content, cavernous sinus and the anterior cranial fossa [30, 74]. The optic nerve and ICA may particularly be bulging or dehiscent, hence increasing the risk of injury during surgery. Even minimal damage to surrounding structures during a surgery could lead to an irrevocable outcome such as blindness or massive bleeding [73]. Furthermore, it has been reported that there are significant anatomical variations of the sphenoid sinus by race, as indicated by Heiwaidi [37] in 2008. Thus, with the aid of the CT scan, it is of paramount importance to understand these structures and its variants especially in a local population.
Computed tomography scans and image-guided surgery (IGS) go hand-in-hand. The IGS technology which was developed in Germany, was first introduced by Anon [3, 31] in 1994. IGS is a real-time correlation of the operative field to pre-operative imaging, displaying the precise location of a selected surgical instrument applied within the surrounding structures [31]. However as mentioned in most literatures, IGS is an adjunct to surgery and is not in any way a substitute for competent surgical skills and sound anatomical knowledge [26, 31].
To operate with the IGS, data from the CT images would have to be uploaded prehand into the system and the appropriate landmarks registered on the patient. A standard helical, 2-mm thickness axial slice is usually sufficient [31]. Any one single imaging modality may not be able to give the full picture of the anatomy or disease state. This is where CT–MRI fusion functions as a fantastic way of demonstrating comprehensive data on a certain selected region, not only to give precise guidance during surgery, but it can also be utilized for targeted radiotherapy planning [17, 19].
Conclusion
The overall broader picture from these various studies appear to reveal that the protrusion rates of optic nerve and ICA are higher than the dehiscence rates of these structures. The sellar type of pneumatization seems to be commoner in Asians and rates of optic nerve and ICA protrusion are higher in Asians as compared to their Turkish or Caucasian counterparts.
There are multiple approaches to the sphenoid sinus. Be it the transseptal, transantral, transpterygoid, transethmoidal, transpalatal or the endonasal endoscopic approach, the choice of approach is determined by the skills of the surgeon and the extent of the disease. Knowledge on the anatomical variations in the respective population, together with the aid of imaging, could result in successful surgeries with lesser complications.
Although the medical field has come a long way in terms of imaging and surgical practices, we have yet to see what more the future holds. However for the present, it would perhaps be wise to bear in mind the possible variations of the anatomical structures of the sphenoid sinus by ethnicity, prior to embarking on surgery. Needless to say it always helps to exercise caution and prudence when operating in the sphenoid sinus region.
References
Abdullah BJ, Arasaratnam S, Kumar G et al (2001) The sphenoid sinuses: computed tomographic assessment of septation, relationship to the internal carotid arteries, and sidewall thickness in the Malaysian population. J HK Coll Radiol 4:185–188
Abuzayed B, Tanriover N, Ozlen F et al (2009) Endoscopic endonasal transsphenoidal approach to the sellar region: results of endoscopic dissection on 30 cadavers. Turk Neurosurg 19(3):237–244
Anon JB, Lipman SP, Oppenheim D et al (1994) Computer-assisted endoscopic sinus surgery. Laryngoscope 104:901–905
Aoki S, Dillon WP, Barkovich AJ et al (1989) Marrow conversion before pneumatization of the sphenoid sinus: assessment with MR imaging. Radiology 172:373–375
Arslan H, Aydinlioğlu A, Bozkurt M et al (1999) Anatomic variations of the paranasal sinuses: CT examination for endoscopic sinus surgery. Auris Nasus Larynx 26(1):39–48
Badia L, Lund VJ, Wei W et al (2005) Ethnic variation in sinonasal anatomy on CT-scanning. Rhinology 43(3):210–214
Bailey et al (1993) Approaches to the sphenoid. In: Head and neck surgery-otolaryngology, 1st edn, vol 1. J.B. Lippincott, Philadelphia, pp 402–412
Bailey et al (1993) Intranasal sphenoidectomy. In: Atlas of head and neck surgery-otolaryngology, 1st edn. J.B. Lippincott, Philadelphia, pp 874–877
Bansberg SF, Harner SG, Forbes G (1987) Relationship of the optic nerve to the paranasal sinuses as shown by computed tomography. Otolaryngol Head Neck Surg 96(4):331–335
Batra PS, Citardi MJ, Gallivan RP et al (2004) Software-enabled computed tomography analysis of the carotid artery and sphenoid sinus pneumatization patterns. Am J Rhinol 18:203–208
Bayram M, Sirikci A, Bayazit YA (2001) Important anatomic variations of the sinonasal anatomy in light of endoscopic sinus surgery: a pictorial review. Eur Radiol 11:1991–1997
Bolger WE, Butzin CA, Parsons DS (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities. Laryngoscope 101:56–64
Bouthillier A, van Loveren HR, Keller JT (1996) Segments of the internal carotid artery: a new classification. Neurosurgery 38(3):4254–4332
Cakur B, Sümbüllü MA, Yılmaz AB (2011) A retrospective analysis of sphenoid sinus hypoplasia and agenesis using dental volumetric CT in Turkish individuals. Diagn Interv Radiol 17(3):205–208
Cavallo LM, de Divitiis O, Aydin S (2007) Extended endoscopic endonasal transsphenoidal approach to the suprasellar area; anatomic considerations: part 1. Neurosurgery 61(3 suppl):24–33
Chapman PR, Shah R, Cure JK et al (2011) Petrous apex lesions: pictorial review. AJR Am J Roentgenol 196(3 suppl)
Chi JW, Brady M, Moore NR et al (2011) Fusion of perpendicular anisotropic MRI sequences. IEEE Int Symp Biomed Imaging 1455–1458
Cho JH, Kim JK, Lee JG et al (2010) Sphenoid sinus pneumatization and its relation to bulging of surrounding neurovascular structures. Ann Otol Rhinol Laryngol 119(9):646–650
Chong VFH, Fan YF, Lau D et al (1998) Functional endoscopic sinus surgery (FESS): what radiologists need to know. Clin Radiol 53:650–658
Ciric I, Ragin A, Baumgartner C et al (1997) Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery 40:225–236
Davis WE, Templer J, Parsons DS (1996) Anatomy of the paranasal sinuses. Otolaryngol Clin N Am 29:57–74
Davoodi M, Saki N, Saki G et al (2009) Anatomical variations of neurovascular structures adjacent sphenoid sinus by using CT scan. Pak J Biol Sci 12:522–525
DeLano MC, Fun FY, Zinreich SJ (1996) Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. Am J Neuroradiol 17(4):669–675
Dessi P, Moulin G, Castro F et al (1994) Protrusion of the optic nerve into the ethmoid and sphenoid sinus: prospective study of 150 CT studies. Neuroradiology 36(7):515–516
Divitiis ED, Esposito F, Cappabianca P et al (2008) Endoscopic transnasal resection of anterior cranial fossa meningiomas. Neurosurg Focus 25(6):E8:1–E8:8
Doshi J, Youngs R (2007) Navigational systems in rhinology: should we all be using them? J Laryngol Otol 121:818–821
Driben JS, Bolger WE, Robles HA et al (1998) The reliability of computerized tomographic detection of the Onodi (sphenoethmoid) cell. Am J Rhinol 12:105–111
Elwany S, Yacout YM, Talaat M et al (1983) Surgical anatomy of the sphenoid sinus. J Laryngol Otol 97:227–241
Filho BCA, Neto CDP, Weber R et al (2008) Sphenoid sinus symmetry and differences between sexes. Rhinology 46:195–199
Fuji K, Chambers SM, Rhoton AL Jr (1979) Neurovascular relationships of the sphenoid sinus. A microsurgical study. Neurosurgery 50:31–39
Fried MP, Parikh SR, Sadoughi B (2008) Image-guidance for endoscopic sinus surgery. Laryngoscope 118:75–80
Greenfield JP, Anand VK, Kacker A et al (2010) Endoscopic endonasal transethmoidal transcribriform transfovea ethmoidalis approach to the anterior cranial fossa and skull base. Neurosurgery 66(5):883–892
Gupta AK, Lynrah ZA, Kalsotra G (2009) Invasive sino-aspergillosis in immunocompetent individuals: atypical presentations. AIJCR 2(3):27–31
Gupta T, Aggarwal A, Sahni D (2013) Anatomical landmarks for locating the sphenoid ostium during endoscopic endonasal approach: a cadaveric study. Surg Radiol Anat 35(2):137–142
Hamid O, Fiky LE, Hassan O et al (2008) Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base 18(1):9–15
Hammer G, Radberg C (1961) The sphenoidal sinus. An anatomical and roentgenological study with reference to transsphenoid hypophysectomy. Acta Radiol 56:401–422
Hewaidi G, Omami G (2008) Anatomic variation of sphenoid sinus and related structures in Libyan population: CT scan study. Libyan J Med 3(3):128–133
Hernández GM, Lorduy TC, García MJV et al (2011) Revision of surgical treatment of rhinosinusitis. Acta Otorrinolar 62(1):56–64
Hidir Y, Battal B, Durmaz A et al (2011) Optimum height from the roof of the choana for seeking the sphenoid ostium. J Craniofac Surg 22(3):1077–1079
Kayalioglu G, Govsa F, Erturk M et al (1999) The cavernous sinus: topographic morphometry of its contents. Surg Radiol Anat 21(4):255–260
Kazkayasi M, Karadeniz Y, Osman KA (2005) Anatomic variations of the sphenoid sinus on computed tomography. Rhinology 43:109–114
Keskin G, Ustündag E, Ciftçi E (2002) Agenesis of sphenoid sinuses. Surg Radiol Anat 24(5):324–326
Kim HU, Kim SS, Kang SS (2001) Surgical anatomy of the natural ostium of the sphenoid sinus. Laryngoscope 111:1599–1602
Kingdom TT, Delgaudio JM (2003) Endoscopic approach to lesions of the sphenoid sinus, orbital apex and clivus. Am J Otolaryngol 24(5):317–322
Lang J (1989) Clinical anatomy of the nose, nasal cavity and paranasal sinuses. Thieme Medical Publishers, New York
Lanza DC, Kennedy DW (1993) In: Ballery Byron J (ed) Endoscopic sinus surgery in head and neck surgery-otolaryngology. J.B. Lippincott, Philadelphia, pp 389–398
Lanzieri CF, Shah M, Krauss D et al (1991) Use of gadolinium-enhanced MR imaging for differentiating mucocoeles from neoplasms in the paranasal sinuses. Radiology 178:425–428
Laws ER Jr (1999) Vascular complications of transsphenoidal surgery. Pituitary 2:163–170
Lehmann P, Bouaziz R, Page C et al (2009) Sinonasal cavities: CT imaging features of anatomical variants and surgical risk. J Radiol 90(1 Pt 1):21–29
Madiha AES, Raouf AA (2007) Endoscopic anatomy of the sphenoidal air sinus. Bull Alex Fac Med 43:1021–1026
Mafee MF, Chow JM, Meyers R (1993) Functional endoscopic sinus surgery: anatomy, CT screening, indications and complications. AJR 160:735–744
Martin TJ, Smith TL, Smith MM et al (2002) Evaluation and surgical management of isolated sphenoid sinus disease. Arch Otolaryngol Head Neck Surg 128:1413–1419
Melhem ER, Oliverio PJ, Benson ML et al (1996) Optimal CT evaluation for functional endoscopic sinus surgery. Am J Neuroradiol 17:181–188
Meloni F, Mini R, Rovasio S et al (1992) Anatomic variations of surgical importance in ethmoid labyrinth and sphenoid sinus. A study of radiological anatomy. Surg Radiol Anat 14(1):65–70
Metson R, Richard E, Gliklich RE (1996) Endoscopic treatment of sphenoid sinusitis. Otolaryngol Head Neck Surg 114:736–744
Momeni AK, Roberts CC, Chew FS (2007) Imaging of chronic and exotic sinonasal disease: review. AJR Am J Roentgenol 189(6 suppl)
Ng YH, Sethi DS (2011) Isolated sphenoid sinus disease: differential diagnosis and management. Curr Opin Otolaryngol Head Neck Surg 19:16–20
Pifferi M, Bush A, Caramella D et al (2011) Agenesis of paranasal sinuses and nasal nitric oxide in primary ciliary dyskinesia. EJR 37(3):566–571
Sapçi T, Derin E, Almaç S et al (2004) The relationship between the sphenoid and the posterior ethmoid sinuses and the optic nerves in Turkish patients. Rhinology 42(1):30–34
Sareen D, Agarwal AK, Kaul JM et al (2005) Study of sphenoid sinus anatomy in relation to endoscopic surgery. Int J Morphol 23(3):261–266
Scuderi AJ, Harnsberger HR, Boyer RS (1993) Pneumatization of the paranasal sinuses: normal features of importance to the accurate interpretation of CT scans and MR images. AJR Am J Roentgenol 160(5):1101–1104
Sethi DS, Stanley RE, Pillay PK (1995) Endoscopic anatomy of the sphenoid sinus and sella turcica. J Laryngol Otol 109(10):951–955
Sethi DS (1999) Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg 120:730–736
Sinnathamby CS (2006) Last’s anatomy, regional and applied, 11th edn. Churchill Livingstone Elsevier, UK
Sirikci A, Bayazit YA, Bayram M et al (2000) Variations of sphenoid and related structures. Eur Radiol 10(5):844–848
Sonbay D, Saka C, Akin I et al (2010) Prevalence of sphenoid sinus agenesis in adults: a CT scan study. B-ENT 6(3):167–169
Stammberger H (1991) Functional endoscopic sinus surgery: the Messerklinger technique. BC Decker, Philadelphia
Stammberger H, Hawke M (1993) Essentials of functional endoscopic sinus surgery. Mosby-Year Book Inc, St Louis
Steven D (1990) Endoscopic sinus surgery: posterior approach. Oper Tech Otolaryngol Head Neck Surg 1:104–107
Synderman CH, Pant H, Carrau RL et al (2009) What are the limits of endoscopic sinus surgery?: the expanded endonasal approach to the skull base. Keio J Med 58(3):152–160
Tan HK, Ong YK (2007) Sphenoid sinus: an anatomic and endoscopic study in Asian cadavers. Clin Anat 20(7):745–750
Turgut S, Gumusalan Y, Arifoglu Y et al (1996) Endoscopic anatomic distances on the lateral nasal wall. J Otolaryngol 25:371–374
Unal B, Bademci G, Bilgili YK et al (2006) Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28(2):195–201
Van Alyea OE (1941) Sphenoid sinus. Anatomic study, with consideration of the clinical significance of the structural characteristics of sphenoid sinus. Arch Otolaryngol 34:225–253
Wang J, Bidari S, Inoue K et al (2010) Extensions of the sphenoid sinus: a new classification. Neurosurgery 66:797–816
Wigand ME, Iro H, Bozzato A (2009) Transcranial combined neurorhinosurgical approach to the paranasal sinuses for anterior skull base malignancies. Skull Base 19(2):151–158
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anusha, B., Baharudin, A., Philip, R. et al. Anatomical variations of the sphenoid sinus and its adjacent structures: a review of existing literature. Surg Radiol Anat 36, 419–427 (2014). https://doi.org/10.1007/s00276-013-1214-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-013-1214-1