Abstract
Accurate knowledge of the anatomy of the bile ducts is critical for successfully hepato-biliary surgery. We describe the anatomical variations of the confluence of the bile ducts, their branches patterns, frequency and classification. From 1996 to 2011, we have collected data of the bile duct confluence. 2,032 and 1,014 anatomical variations of right and left bile ducts, respectively, were reviewed and classified according to the branching pattern. The frequencies of each type of the right hepatic duct (RHD) were as follows: Type A1—1,247 (61.3 %); Type A2—296 (14.5 %); Type A3—272 (13.3 %); Type A4—124 (6.1 %); Type A5—21 (1 %) and others—72 (3.5 %) and, for the left hepatic duct (LHD) was as follows: Type B1—773 (76.2 %); Type B2—153 (15 %); Type B3—38 (3.7 %); Type B4—9 (0.8 %); Type B5—29 (2.8 %) and others—12 (1.1 %). Atypical branching patterns of both the right and left hepatic ducts were found in 14 and 8 %, respectively. The two most common variations of the RHD were right anterior and posterior hepatic ducts join together to form the RHD and trifurcation where the RHD is absent and right anterior and posterior hepatic ducts join directly to the confluence with the LHD to form the common hepatic duct. The two most common variations in the LHD were segment IV drainage to the left and right hepatic ducts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to Couinaud [5], the hepatic biliary tract is made up of hepatic ducts that follow a modal disposition identical to that of the portal vein. The common hepatic duct (CHD) is formed from the reunion, at the level of the hepatic vein, of the left hepatic duct supplying segments I to IV and the right hepatic duct supplying segments V to VIII.
On the left side, the segmental duct for segment III receives the duct for segment II, and farther along the duct for segment IV. It then becomes the left hepatic duct (LHD) and receives, at its terminal part, the duct of segment I (sometimes partially empty into terminal part of the right hepatic duct).
The LHD drains segments II, III and IV of the left hemi-liver. The so-called normal confluence comprises a duct formed from ducts of segments II and III and one or more ducts from segment IV.
The segment III duct follows the left horn of the Rex recessus and joins the segment II duct above the segment II portal branch. For the LHD, this normal anatomy is reported in 82 %. In 4 % of patients, a right sectoral duct can join the LHD (3 % posterior and 1 % anterior) [3].
The right hepatic duct (RHD) is formed from the reunion of the lateral hepatic duct supplying segments VI and VII and the paramedian hepatic duct supplying segments V and VIII. But this modal disposition is only found in 57 % of cases [5]. There are, therefore, many anatomic variants of the convergence of biliary ducts.
The RHD may join the main hepatic duct below the normal confluence in 25 % of the cases (9 % anterior and 16 % posterior). A complete anterior duct was present in 35 % and a complete posterior duct in 61 % [3].
This study describes the anatomic variations of both right and left bile ducts confluence in terms of branching, drainage patterns, frequency and its classification.
Materials and methods
Patient selection
From 1996 to 2011, we have collected data of both right and left bile ducts confluence anatomy and its variations in the literature. 2,032 and 1,014, respectively, right and left anatomy variations were reviewed. We have used anatomical terminology according to Matusz [10].
Anatomic classification
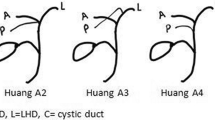
Classification of the RHD anatomy according to Huang et al. [8], Nakamura et al. [11] and Varotti et al. [18] was studied by ERC, IOC, computerized tomography and Doppler ultrasonography, and surgical findings. The biliary tree in the right lobe was classified into six types based on right posterior hepatic duct (RPHD) and right anterior hepatic duct (RAHD) insertion: Type A1—RAHD and RPHD join together to form the right hepatic duct (RHD); Type A2—The RHD is absent and RAHD and RPHD join directly to the confluence with the LHD to form the CHD; Type A3—The RAHD (type 3a) or the RPHD (type 3b) opens directly into the LHD; Type A4—RAHD (type 4a) or the RPHD (type 4b) opens directly into CHD; Type A5—RPHD opens to cystic duct or its periphery aberrantly and others (for instance accessory duct to CHD and to RHD).
The LHD anatomy was classified only, by ERC, according to Huang et al. [8], into six types based on the segment IV insertion: Type B1—segment IV duct opens to left hepatic duct (LHD); Type B2—segment IV opens to CHD separately of the segment II and III duct; Type B3—segment IV opens to RAHP; Type B4—segment IV opens to CHD; Type B5—segment IV opens to segment II duct and others (for instance segments II and III drain individually into the RHD or CHD).
Imaging analysis
The RHD anatomy and their variations were assessed by: endoscopic retrograde cholangiography (ERC)—1,211 (59.5 %); intraoperative cholangiography (IOC)—418 (20.5 %); abdominal ultrasonography with Doppler and/or multi-sliced computed tomography and/or magnetic resonance imaging and/or IOC—124 (6.1 %); IO + operative report—77 (3.7 %). The LHD anatomy and their variations were assessed by: ERC—959 (94.5 %); IOC + 3D reconstruction—55 (5.4 %).
Results
The branches patterns of RHD were classified as one of the six types for both right and left hepatic ducts.
Right bile duct
The frequencies of each type of the 2,032 RHD variations were as follows: Type A1—1,247 (61.3 %); Type A2—296 (14.5 %); Type A3—272 (13.3 %); Type A4—124 (6.1 %); Type A5—21 (1 %) and others—72 (3.5 %), (Figs. 1, 2; Table 1).
Huang et al. [8] classification. Right hepatic duct divided into five types according to sectoral bile drainage and its respective frequencies
Left bile duct
The frequencies of each type of the 1,014 LHD variations were as follows: Type B1—773 (76.2 %); Type B2—153 (15 %); Type B3—38 (3.7 %); Type B4—9 (0.8 %); Type B5—29 (2.8 %) and others—12 (1.1 %), (Fig. 3; Table 2).
Huang et al. [8] classification. Left hepatic duct divided into six types according to segmental bile drainage and its respective frequencies
Discussion
Knowledge of bile duct anatomical variations is crucial for surgical procedures such as liver resection, partial liver transplantation and also for minimizing postoperative complications. Many anatomical studies have been conducted to determine the specific hepatic bile duct anatomical variations [2, 9].
Postmortem anatomic studies of the biliary tract, after injection and corrosion, provide precise and reliable information on the anatomy of the biliary tract and its variants, as was clearly shown by Couinaud [5]. However, this method has its limitations. It is difficult to implement and sometimes fragments of biliary tree molds break, making detailed interpretation of biliary tract delicate.
Several preoperative examinations have been proposed to visualize biliary anatomy including ERC, percutaneous trans-hepatic cholangiography, ultrasonography with Doppler, multisliced computer tomography and magnetic resonance imaging [1, 4, 8, 9, 11, 12, 15, 18]. ERC is an invasive investigation requiring a short general anesthesia. Mortality risks are 1 % and morbidity reaches 7 % [14]. It yields high-quality 2D images of biliary tract. Percutaneous trans-hepatic cholangiography is another invasive technique with a high anatomic and diagnostic value despite the fact that flow of contrast medium is not very well seen because of the spatial structure of the biliary tree [19]. Nuclear magnetic resonance cholangiography and intravenous CT cholangiography are non-invasive procedures requiring injection in the biliary tract. It is highly feasible and has very few contraindications and the only limitation is cost [17]. Yeh et al. [20] who compared of all these techniques except oral contrast agent-enhanced CT cholangiography have shown that intravenous CT cholangiography enabled significantly better visualization than the other methods. Our study has shown that 2,170 (71.2 %) right and left anatomy and their variations were assessed by ERC and 495 (16.2 %) by IOC.
Although numerous biliary tract variations have been reported, we have found that they can be classified into five major categories, type A1 to A5, and type B1 to B5, respectively, for right and left bile ducts (Tables 1, 2).
The normal biliary anatomy has been reported to be present in 52.9–58 % of the population [11]. Anomalous drainage of the RPHD into the LHD is described as the most common atypical anatomy with rates from 11 to 15.6 %. The triple confluence and direct drainage of the RPHD into CHD have frequencies of 14–19 and 5.5 %, respectively (Figs. 1, 2).
In our findings, almost 90 % of the RHD variations were: Type A1—RAHD and RPHD join together to form the RHD; Type A2—the RHD is absent and RAHD and RPHD join directly to the confluence with the LHD to form the CHD and Type A3—the RAHD or the RPHD opens directly into the LHD. Drainage of the RPHD into LHD before its confluence with RAHD was found to occur in 13–19 % of the population [6]. Huang et al. [8] has found a variant form in 5,8 % in which the RPHD drained into the cystic duct. It has been reported that the incidence of this anatomic variation, known as “cystohepatic ducts”, is 1–2 % [3, 16]; in addition, Hamlin [7] reported that in his experience, an anomalous RHD emptying into CHD or cystic duct was the most common biliary anomaly. Reid et al. [13] reported that three of 267 cholangiograms depicted anomalous RHD which emptied into the cystic duct.
Less than 11 % corresponding to type A4, A5 and others such as: RAHD or the RPHD opens directly into CHD and RPHD opens to cystic duct or its periphery aberrantly. In addition, 95 % of the LHD variations were: Type B1—segment IV duct opens to LHD; Type B2—segment IV opens to CHD separately of the segment II and III duct and Type B3—segment IV opens to RAHD.
Less than 5 % corresponding to type B4, B5 and others such as: segment IV opens to CHD and segment IV opens to segment II duct. Anomalous drainage of segment IV into RAHD and in segment II has rates of 4 and 3 %, respectively. The drainage could be much less frequent in the CHD with rates of 1 %. Also segment IV drained independently into RHD and RAHD in 16 and 4 %, respectively [8].
Choi et al. [4] reported that the first branch of the LHD was absent in 1 % of 293 IOC, in whom bile from segment II and III drained independently into RHD and CHD, respectively. Huang et al. [8] reported bile from segment II and segment IV drained independently into CHD in 3 and 1 %, respectively.
Conclusion
Atypical branching patterns of both the right and left hepatic ducts were found in 14 and 8 %, respectively. The two most common variations of the RHD were right anterior and posterior hepatic ducts which join together to form the RHD and trifurcation where the RHD is absent and right anterior and posterior hepatic ducts join directly to the confluence with the LHD to form the common hepatic duct. The two most common variations in the LHD were segment IV drainage to the left and right hepatic ducts.
References
Bageacu S, Abdelaal A, Ficarelli S, ElMeteine M, Boillot O (2011) Anatomy of the right liver lobe: a surgical analysis in 124 consecutive living donors. Clin Transpl 25:E447–E454
Chaib E, Ribeiro MA Jr, Saad WA, Gama-Rodrigues J (2005) The main hepatic anatomic variations for the purpose of split-liver transplantation. Transpl Proc 37(2):1063–1066
Champetier J, Letoublon C, Arvieux C, Gerard P, Labrosse P-A (1989) Les variations de division des voies biliares extra-hépatiques: signification et origine, consequences chirurgicales. J Chir 126:147–154
Choi JW, Kim TK, Kim KW, Kim AY, Kim PN et al (2003) Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol 4:85–90
Couinaud C (1957) Le foie. Etudes Anatomiquesetchirurgicales, Edition Masson
Gazelle GS, Lee MJ, Mueller PR (1994) Cholangiographic segmental anatomy of the liver. RadioGraphics 14:1005–1013
Hamlin JA (1981) Biliary ductal anomalies. In: Berci G, Hamlin JA (eds) Operative biliary radiology, 1st edn. Williams & Wilkins, Baltimore, pp 110–116
Huang TL, Cheng YF, Chen CL, Chen TY, Lee TY (1996) Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transpl Proc 128:1669–1670
Karakas HM, Celik T, Alicioglu B (2008) Bile duct anatomy of the Anatolian Caucasian population: Huang classification revisited. Surg Radiol Anat 30:539–545
Matusz P (2011) Right/left symmetry of the intrahepatic distribution and terminology of the hepatic artery proper and the intrahepatic bile duct system: proposals to revise the Terminologia Anatomica. Surg Radiol Anat 33:71–74
Nakamura T, Tanaka K, Kiuchi T, Kasahara M, Oike F et al (2002) Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation 73:1896–1903
Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K et al (2004) Surgical anatomy of the bile ducts at the hepatic hylum as applied to living donor liver transplantation. Ann Surg 239:82–86
Reid SH, Cho SR, Shaw CI, Turner MA (1986) Anomalous hepatic inserting into the cystic duct. AJR Am J Roentegenol 147:1181–1182
Reinhold C, Bret PM (1996) Current status of MR cholangiopancreatography. AJR 166:1285–1295
Sharma V, Saraswat VA, Baijal SS, Choudhuri G (2008) Anatomic variations in intrahepatic bile ducts in a north Indian population. J Gastroenterol Hepatol 23:e58–e62
Turner MA, Fulcher AS (2001) The cystic duct: normal anatomy and disease processes. RadioGraphics 21:3–22
Van Hoe L, Vanbeckevoort D, Van Steenbergen W (1999) Atlas of cross-sectional and projective MR cholangiography. Springer, Berlin
Varotti G, Gondolesi GE, Goldman J, Wayne M, Florman SS et al (2004) Anatomic variations in right liver living donors. J Am Coll Surg 198:577–582
Zlatos J, Moravec R, Gatial J, Paiko V, Mentel J (1995) Topometry of normal intrahepatic bile ducts. Surg Radiol Anat 17:151–154
Yeh BM, Breiman RS, Taouli B, Qayyum A, Roberts JP et al (2004) Biliary tract depiction in living potential liver donors: comparison of conventional MR, mangafodipir trisodium-enhanced excretory MR, and multidetector row CT cholangiography—initial experience. Radiology 230:645–651
Acknowledgments
We would like to thank Mr. Marcos Retzer for the drawings of this paper. No funding was received.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chaib, E., Kanas, A.F., Galvão, F.H.F. et al. Bile duct confluence: anatomic variations and its classification. Surg Radiol Anat 36, 105–109 (2014). https://doi.org/10.1007/s00276-013-1157-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-013-1157-6