Abstract
The geometric mismatch analysis of the retrograde nail was performed in 108 Asian cadaveric adult femora. The insertion was done virtually based on a three-dimensional geometric model derived from computed tomographic images. The investigation was performed at eight levels located at 120, 140, 160, 180, 200, 220 and 240 mm above the condylar surface. The evaluation of each level included: (1) the diameter of the intramedullary canal, (2) the percentage of area filled by the nail in the unreamed intramedullary canal, (3) the minimal reamer diameter that required enlargement of the canal to accommodate retrograde nail insertion, (4) the minimal inner cortical reaming thickness that needed to be removed, (5) the percentage of the cortical bone area that needed to be removed prior to nail insertion and (6) the deviation of the nail center from the center of the intramedullary canal. The result showed significant mismatch of the nail to most of the study specimens (94 femora, 87%), which the intramedullary canal needed extensive reaming to accommodate the nail insertion. This may lead to a high possibility of clinical complications. Redesign for proper shape and size of retrograde nail should be considered for the use in Asian population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Closed intramedullary nailing using retrograde nail inserted from the intercondylar notch into the intramedullary canal is now widely accepted as a treatment method for distal femoral shaft fractures and supracondylar fractures [7, 8, 12–17, 19, 20]. Many authors have reported complications of using intramedullary nail, which may occur from the mismatch of the nail to the femur [2, 5, 7, 10, 11]. These include secondary fractures due to bursting of intramedullary nail to cortical bones, poor anatomical alignment and bone weakening due to excessive cortical reaming. Since most available intramedullary nails are designed based on Caucasian anatomy, when those devices are used in Asian population, surgical complications may occur [11].
In previous study of Leung et al. [9], the mismatch analysis of trochanteric gamma nail to the Chinese femur was conducted based on two-dimensional radiographic technique. A similar two-dimensional technique was also found in the study of Egol et al. [4] who conducted the mismatch study of gamma nail to the femur from the collection of museums in the United States. Since computed tomography (CT) technology presents the powerful ability in constructing the three-dimensional medical model, Mahaisavariya et al. [11] and Chevalley et al. [3] used this advantage by integrating the abilities of computer-aided design/computer-aided manufacturing (CAD/CAM) to access the mismatch of various intramedullary nails to the femur in three dimensions. Both literatures present the important information about using the advanced technology to improve the design of intramedullary nails for the proximal femur. Because there is no previous study focused on the mismatch of retrograde nail to femoral canal in Asian population, the authors therefore conducted this study to raise awareness of clinical application of such retrograde nailing method in Asian cadaveric femora.
Methods
The study was conducted three-dimensionally using CT images combined with reverse engineering and CAD/CAM techniques. By this way of study, the critical parameters of geometric mismatch could be accessed. All three-dimensional models of femur and retrograde nail presented in this study were constructed using reverse engineering techniques via CAD software package (Mimics and Magics, Materialise N.V., Belgium).
Data acquisition
Specimens of 108 Thai adult cadaveric femora from Department of Anatomy, Faculty of Medicine, Siriraj Hospital, Mahidol University, Thailand as representatives of Asian anatomy, were used in this study. Each specimen was scanned using CT scanner. In the proximal and the distal region, the geometric data were recorded at 3-mm slice thickness and the interpolation was done at 1-mm slice thickness. For the femoral shaft region, the geometric data were recorded at 10-mm slice thickness and the interpolation was done at 5-mm slice thickness. The CT images obtained from the CT scanner using the aforementioned technique were then used to construct a three-dimensional model of femur. Different threshold values were used to extract the geometry of different regions of the femur. The high threshold value was applied to the cortical region, whereas the low threshold value was applied to intramedullary canal. The geometric data of each femur were then exported as Stereolithography (STL) file format.
Retrograde nail employed in this study had a 10-mm diameter and 260-mm length (Zimmer Inc, USA). Three-dimensional laser scanner was used to capture the geometry of the retrograde nail. Reverse engineering technique was then used to construct a three-dimensional model of the retrograde nail. The geometric data were also exported as STL file format.
Virtual insertion
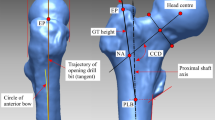
The three-dimensional retrograde nail model was virtually inserted to the femur model by means of various functions of CAD software. The details of virtual insertion can be summarized as follows:
-
1.
Dividing femoral region. As illustrated in Fig. 1a, each femur was divided into three regions. The boundary for dividing femur is 35 and 65% of femoral length [18]. The region above 35% boundary line is the proximal femur. The region in between 35 and 65% boundary line is the femoral shaft. The rest below 65% boundary line is the distal femur.
-
2.
Calculating femoral shaft axis. As illustrated in Fig. 1b, the femoral shaft axis was obtained from the intramedullary canal at femoral shaft region of each femur. This was done by approximating the cross-sectional of intramedullary canal as a two-dimensional circle. Centers of each circle were then fit using linear regression algorithm to obtain femoral shaft axis.
-
3.
Calculating retrograde nail axis. As illustrated in Fig. 1c, the retrograde nail axis was obtained based on the outer surface of retrograde nail in straight portion. This was also done by approximating the surface of retrograde nail as a two-dimensional circle. Centers of each circle were then fit using linear regression algorithm to obtain retrograde nail axis.
-
4.
Aligning retrograde nail axis to femoral shaft axis. As illustrated in Fig. 1d, the retrograde nail axis was aligned to the femoral shaft axis using “Best-fit alignment” functions in CAD software. It is a function used to align objects by referencing each of the object’s axes. After the two axes were superimposed to each other, the retrograde nail was allowed to rotate and translate only along the femoral shaft axis. The retrograde nail was rotated until the distal screw of retrograde nail was parallel to the anteroposterior direction. The translation along the femoral axis was done repeatedly until the distal end of the retrograde nail was located just below the cortical condylar surface.
Geometric mismatch evaluation
The important parameters of geometric mismatch were evaluated as shown in Fig. 2. These included the diameter of the intramedullary canal, the percentage of area filled by the nail in the unreamed intramedullary canal, the minimal reamer diameter that required enlargement of the canal to accommodate retrograde nail insertion, the minimal inner cortical reaming thickness that needed to be removed, the percentage of the cortical bone area that needed to be removed prior to nail insertion and the deviation of the nail center from the center of the intramedullary canal [11]. From Fig. 3, eight levels located at 120, 140, 160, 180, 200, 220 and 240 mm above the condylar surface were investigated. The details of assessment can be summarized as follows:
-
1.
Fitting circle. At each consideration level, the two-dimensional circular approximation algorithm was used to approximate the diameter of intramedullary canal and retrograde nail. The assessment of unreamed diameter of intramedullary canal could be measured at this step.
-
2.
Calculating geometric mismatch parameters. The other geometric mismatch parameters were calculated using the following equations [11].
-
2.1
The percentage of area filled by the nail in the unreamed intramedullary canal
$$ \% {\text{area filled in the canal }} = \% \left( {{\text{area}}_{\rm filled\;by\;nail} /{\text{area}}_{\text{canal}} } \right). $$ -
2.2
The minimal reamer diameter that required enlargement of the canal to accommodate retrograde nail insertion.
$$ {\text{minimal reaming diameter}} = 2 \times \left( {{\text{radius}}_{\text{canal}} + {\text{distance}}_{\rm{out\;of\;centricity}} } \right). $$ -
2.3
The minimal inner cortical reaming thickness that needed to be removed
$$ {\text{minimal inner cortical reaming thickness = }}{{\left( {{\text{minimal reaming diameter}} - {\text{canal diameter}}} \right)} \mathord{\left/ {\vphantom {{\left( {{\text{minimal reaming diameter-canal diameter}}} \right)} 2}} \right. \kern-\nulldelimiterspace} 2}. $$ -
2.4
The percentage of the cortical bone area that needed to be removed prior to nail insertion
$$ \% {\text{bone removal}} = \% {{\left( {{\text{area}}_{\rm{minimal\;reaming}} - {\text {area}}_{\text{canal}} } \right)} \mathord{\left/ {\vphantom {{\left( {{\text{area}}_{\rm{minimal\;reaming}} - {\text {area}}_{\text{canal}} } \right)} {{\text{area }}_{\text{canal}} }}} \right. \kern-\nulldelimiterspace} {{\text{area}}_{\text{canal}} }}. $$ -
2.5
The deviation of the nail center from the center of the intramedullary canal
$$ {\text{The deviation of the nail center from center of the canal}} = {\text{position}}_{\rm{canal\;center}} - {\text{ position}}_{\rm{nail\;center}}.$$
-
2.1
Results
According to this study, the result could be classified into two groups according to the characteristic of geometric mismatch. For Group A, the specimens presented significant mismatch, where some portion of the retrograde nail protruded from the outer cortical boundary, as illustrated in Fig. 4. For Group B, the specimens had no critical mismatch, where the retrograde nail could contain within the outer cortical boundary of femur. From the virtual insertion, it reveals that 94 femora (87%) were in Group A and only 14 femora were in Group B. Since the critical aspect occurred in Group A, the average values of geometric mismatch parameters of 94 Asian’s cadaveric femora at each level were then evaluated, as shown in Table 1.
Discussion
The progress of various engineering technologies such as CT scanner and reverse engineering enables the construction of three-dimensional medical models. This allows examining the complex geometric structure, which may be difficult to carry out based on conventional two-dimensional radiographic technique. Moreover, it makes possible to access the internal geometry of bone, especially intramedullary canal without destruction of specimens. Based on CT technologies, there are two reports, which have evaluated the mismatch of the nail to the proximal femur [3, 11]. To our knowledge, the geometric mismatch analysis of the retrograde nail to the femur has never been reported.
This study presented the assessment of geometric mismatch parameters of the retrograde nail and the femur based on three-dimensional models. From the analysis, it showed the critical aspect of using the retrograde nail in the Asian femur. Most of the specimens exhibited significant mismatch, which the radius of curvature of the retrograde nail could not compensate to the radius of curvature of the intramedullary canal.
Although this study was focused on the retrograde nail system, the appropriate virtual position of the nail should be considered first at the mid-shaft of femur instead of the distal femur. This is because the dimension of the bone in mid-shaft region is small and there is limited space for nail accommodation. It is also a fact that the nail should be placed with a sufficiently long distance within this femoral shaft region for the stability of nail fixation. After the mismatch at the shaft region was analyzed, the mismatch analysis of the distal part can be verified. The significant mismatch can be identified from the appearance of penetration of the nail out of the boundary of the anterior cortex of the femur in the sagittal plane.
Normally, the shaft portion of retrograde nail is quite straight, whereas the author’s previous study showed significant degrees of curvature in the Asian femur [1]. It has been found that the Asian femur presents a greater degree of curvature than the curvature of the Caucasian population. Therefore, in order to avoid penetration of the nail or impingement of the nail to the anterior cortex based on Caucasian design, the appropriate length of the retrograde nail has to be considered. The recommendation is that the nail length should be sufficient to cover the supracondylar fracture. As a result, the nail accommodation can be done without constrain of mid-shaft anatomy as well as the unnecessary reaming beyond fracture site can be avoided. However, it should be noted that the use of retrograde nail for mid-shaft fracture may require over-reaming to accommodate the straight nail portion in curve femur. The risk due to excessive over-reaming, which subsequently reduces bone strength [6] should be considered.
Even though, the femoral anatomy at fracture site can be adjusted to compensate the nail accommodation, the femoral curvature may not be the same as the original femoral curvature. Therefore, to achieve the proper femoral curvature and to minimize any complications from using the existing retrograde nail, redesign is recommended. In order to achieve the proper nail design, the parameters such morphometric data of the intramedullary canal, femoral radius of curvature and geometric mismatch data should be taken into account. For Asian population, the proper diameter of the retrograde nail is about 10 mm. However, the major modification for the current retrograde nail seems to be its radius of curvature, which should be reduced to approximately 900 mm [1]. In addition, the new design should be further investigated biomechanical performance evaluation.
Various advanced technologies relating to virtual prototyping such as medical image processing, reverse engineering and CAD/CAM enabled us to examine the parameter of geometric mismatch virtually in three dimensions. Before the availability of these technologies, the geometric mismatch evaluation based on two-dimensional technique or manual measurement may present inaccurate data due to the lack of ability in assessment in some view of the configurations and human error in measurement. The geometric mismatch assessment by means of three-dimensional technique as presented in this study can be further applied to evaluate the mismatch of various fracture fixations. By this way of investigation, it would be beneficial for a surgeon to acknowledge the possible risk in using existing design of intramedullary fracture fixation in a specific group of population. In addition, the redesign of devices according to the parameters of geometric mismatch would be useful to reduce any possible implant-related complications.
Conclusion
In conclusion, the study presented an advanced technique of using CT data in assessing the internal geometry of femur without destroying. With the aid of useful engineering technologies such as medical image processing, reverse engineering and CAD/CAM, it greatly empowers us to construct three-dimensional CAD models of femur and implant. Furthermore, the striking feature of using these advanced technologies is the examination of geometry in the three-dimensional configurations, where the conventional two-dimensional radiographic technique cannot access. By this technique, several significant points of the geometric mismatch of retrograde nail in the Asian femur were obtained. It is obviously seen from the results that the existing design of retrograde nail has shown a significant mismatch to the Asian femur. The redesign of the retrograde nail for the Asian population is highly recommended.
References
Chantarapanich N, Sitthiseripratip K, Mahaisavariya B, Wongcumchang M, Siribodhi P (2008) 3D geometrical assessment of femoral curvature: A reverse engineering technique. J Med Assoc Thai 91(9):1377–1381
Cheung G, Zalzal P, Bhandari M, Spelt JK, Papini M (2004) Finite element analysis of a femoral retrograde intramedullary nail subject to gait loading. Med Eng Phys 26(2):93–108
Chevalley F, Rubin P (2001) Fit-and-fill analysis of different intramedullary nails for the proximal femur. Eur J Trauma 27(4):178–183
Egol KA, Chang EY, Cvitkovic J, Kummer FJ, Koval KJ (2004) Mismatch of current intramedullary nails with the anterior bow of the femur. J Orthop Trauma 18(7):410–415
Harma A, Germen B, Karakas HM, Elmali N, Inan M (2005) The comparison of femoral curves and curves of contemporary intramedullary nails. Surg Radiol Anat 27(6):502–506
Hipp JA, McBroom RJ, Cheal EJ, Hayes WC (1989) Structural consequences of endosteal metastatic lesions in long bones. J Orthop Res 7(6):828–837
Khare A, Mehra MM (2002) Retrograde femoral interlocking nail in complex fractures. J Orthop Surg 10(1):17–21
Kumar A, Jasani V, Butt MS (2000) Management of distal femoral fractures in elderly patients using retrograde titanium supracondylar nails. Injury 31(3):169–173
Leung KS, Procter P, Robioneck B, Behrens K (1996) Geometric mismatch of the gamma nail to the Chinese femur. Clin Orthop Relat Res (323):42–48
Mahaisavariya B, Laupattarakasem W (1992) Cracking of the femoral shaft by the Gamma nail. Injury 23(7):493–495
Mahaisavariya B, Sitthiseripratip K, Oris P, Chaichanasiri E, Suwanprateeb J (2004) Fit-and-fill analysis of trochanteric gamma nail for the Thai proximal femur: A virtual simulation study. J Med Assoc Thai 87(11):1315–1320
Menth-Chiari WA, Wozasek GE, Vécsei V (1996) Retrograde nailing of supracondylar femoral fractures in patients with total hip arthroplasty: a preliminary report. J Trauma 41(6):1059–1063
O’Mara T, Barei DP, Taitsman LA, Vallier H, Chapman JR (2005) Pertrochanteric femur fracture at the proximal end of a retrograde intramedullary nail––a case report. Injury Extra 36(7):271–276
Ostrum RF, Maurer JP (2009) Distal third femur fractures treated with retrograde femoral nailing and blocking screws. J Orthop Trauma 23(9):681–684
Parrόn R, Tomé F, Pajares S, Herrera JA, Madruga JM, Hermida Á, Barriga A (2008) Treatment of periprosthetic knee fractures in the distal femur by means of retrograde intramedullary nailing. Rev Ortop Traumatol 51(6):314–318
Ponzer S, Tidermark J, Törnkvist H (1998) Retrograde Nailing of Femoral Fractures Distal to a Moore Prosthesis. J Orthop Trauma 12(8):588–591
Singh SK, El-Gendy KA, Chikkamuniyappa C, Houshian S (2006) The retrograde nail for distal femoral fractures in the elderly: High failure rate of the condyle screw and nut. Injury 37(10):1004–1010
Stephenson P, Seedhom BB (2001) Modelling femoral curvature in the sagittal plane: A cadaveric study. Proc Inst Mech Eng H 215(2):221–228
Tan KG, Sathappan SS (2010) Operative fixation of a subtrochanteric fracture in a patient with previous spontaneous hip fusion. Singapore Med J 51(6):e107–e110
Zuurmond RG, Pilot P, Verburg AD, Van Os JJ, Verdonschot N (2008) Retrograde bridging nail in periprosthetic femoral fracture treatment which allows direct weight bearing. Proc Inst Mech Eng H 222(5):629–635
Acknowledgments
The authors would like to acknowledge the Department of Anatomy, Faculty of Medicine, Siriraj Hospital, Mahidol University, Thailand for their kind support of the cadaveric bone specimens and the National Metal and Materials Technology Center (MTEC), Thailand for their kind support of providing the use of their facilities. In addition, the authors are grateful to Thailand Advanced Institute of Science and Technology (THAIST)’s pilot project, National Science and Technology Development Agency (NSTDA) for the scholarship support.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chantarapanich, N., Mahaisavariya, B., Siribodhi, P. et al. Geometric mismatch analysis of retrograde nail in the Asian femur. Surg Radiol Anat 33, 755–761 (2011). https://doi.org/10.1007/s00276-011-0813-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-011-0813-y