Abstract
Background
A large patent median artery can be involved in several clinical disorders like carpal tunnel syndrome, anterior interosseous nerve syndrome and pronator syndrome.
Methods
The frequency and variability in the expression of the median artery and the expression of the other forearm arteries were recorded during two dissection courses. The topography of the arteries with their ramifications was documented on diagrams and photographs. The outer diameters of forearm arteries were measured.
Results
A large median artery was found in 4 of 54 arms (7.4%). The median arteries took their origin from the ulnar artery or the common interosseous artery. In one case, the median artery pierced the median nerve in its course under the pronator teres. The outer diameters of the median arteries varied between 1.5 and 2.0 mm proximally and 1.5 and 2.0 mm distally. The diameters of the radial arteries varied between 3.0 and 5.5 mm proximally and 3.0 and 4.0 mm distally and were not reduced in any of the four cases with a large median artery.
Conclusions
Surgeons should be aware of other variations in the forearm when a persistent median artery is identified, for example high median nerve bifurcations. Furthermore, it should be kept in mind that additional structures leading to nerve compression may be present in the carpal tunnel.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The superficial palmar arch and its supplying arteries are highly variable [28, 32, 50]. Classical textbooks note the fact that the median artery (arteria comitans nervi mediani) can be involved in the construction of the superficial palmar arch by replacing the superficial palmar branch of the radial artery. In these cases, a median artery, which is more strongly developed than normal accompanies the median nerve on its way through the carpal tunnel and connects itself with the superficial palmar arch [25, 28]. In some cases, the median artery continues into a digital artery [12] and not seldomly into the second common palmar artery [28]. The diameter of the radial artery can be diminished if the median artery is well developed [28]. The median artery can branch off from the brachial artery, the ulnar artery or the anterior interosseous artery [20, 25]. According to Meckel [36], it is very rare that a branch taking off from the interosseous artery is involved in the construction of the superficial palmar arch. However, the frequencies of the median artery observed in cadavers varied from 1.1 to 17% [1, 15, 17, 51]. Olave et al. [39] dissected 102 hands of 51 adult cadavers of both sexes aged between 23 and 77 years and injected latex into 42 hands. The authors found the median artery in 23 of 102 cases (23%) with their diameters ranging from 0.7 to 2.7 mm.
A large patent median artery can have a special topographical relation to the canalis carpi, the median nerve and the anterior interosseous nerve. Therefore, the median artery can be involved in several clinical disorders like carpal tunnel syndrome [37], anterior interosseous nerve syndrome [41] and pronator syndrome [22].
Here, we report on the frequency and the variable expression of the median artery, taking into account the expression of the other forearm arteries. Furthermore, we report a case where the median nerve was perforated by the median artery underneath the pronator teres and discuss clinical disorders evoked by a large patent median artery.
Materials and methods
In the winter terms of 2004–2005 and 2005–2006, the upper extremities of the gross anatomy courses of the Rostock Anatomical Institute were inspected for variations of the arteries, especially, for the presence of a strongly developed median artery and a possible involvement in the construction of the superficial palmar arch. Generally, the pronator teres was dissected to visualize the route of the ulnar artery with its branches. The topography of the arteries with their ramifications and their relation to the surrounding muscles was documented in diagrams and photographs. The outer diameters of the median artery and of the other arteries of the lower arm including their ramifications were measured with the use of a calliper. The diameters were measured 1–2 cm distal to the respective origins of the vessels. Concerning the superficial and deep palmar arches, the greatest outer diameters were measured.
Results
Altogether, the median nerve was accompanied by a strongly expressed median artery on its route passing the carpal tunnel in 4 of 54 arms (7.4%). The diameters of the forearm arteries are summarized in Table 1.
Right arm of a 70-year-old man with median artery perforating the median nerve and participating in the construction of the superficial palmar arch
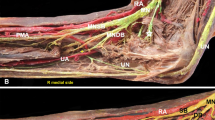
The median artery branched off from the ulnar artery just after the common interosseous artery left this vessel (Fig. 1a, b). At a distance of 6 cm from the point where the radial artery separated from the brachial artery, the median artery covered by the pronator teres perforated the median nerve in the radial to ulnar direction (Fig. 1b). In this region, the median artery and median nerve crossed over an additional head of flexor pollicis longus (Fig. 1a). Thereafter, the vessel accompanied the median nerve, which was located under the second finger part of the flexor digitorum superficialis (Fig. 1a). A topographical relation of the median artery to the anterior interosseous nerve was not observed. Approximately, 7 cm proximal from the wrist joint, both median artery and median nerve located between flexor digitorum superficialis and flexor carpi radialis became more superficial and passed the carpal tunnel. The median artery provided the superficial palmar arch together with the ulnar artery. The median artery joined the superficial palmar arch at the level of the second intercarpal space. The superficial palmar branch of the radial artery was absent. However, after piercing the first metacarpal space, the radial artery nourished the deep palmar arch. A deep palmar branch of the ulnar artery for the deep palmar arch was missing. Three palmar metacarpal arteries left the deep palmar arch, while the superficial palmar arch gave off four common palmar digital arteries (Fig. 1a).
Diagram and photograph of arm 1 from a 70-year-old man with a median artery perforating the median nerve. (a) The median artery takes its origin from the ulnar artery (1) and perforates the median nerve underneath the pronator teres (2). The median artery nourishes the superficial palmar arch (3). (b) Pronator teres had been resected to show the origin of the median artery from the ulnar artery. AIA anterior interosseous artery, BA brachial artery, CPDAA common palmar digital arteries, MA median artery, MN median nerve, PIA posterior interosseous artery, PPDAA proper palmar digital arteries, PT-PP pronator teres (proximal part), PT-DP pronator teres (distal part), RA radial artery, RUA recurrent ulnar artery, SPA superficial palmar arch, UA ulnar artery
Left arm of an 80-year-old woman with median artery not involved in the formation of the superficial palmar arch
The median artery originated from the common interosseous artery (Fig. 2a, b) and accompanied the median nerve through the carpal tunnel. Afterwards, two common palmar digital arteries for the nutrition of the thumb and the second finger arose from the median artery (Fig. 2a). The ulnar artery also gave off two common palmar digital arteries for the nutrition of the third, fourth and fifth finger (Fig. 2a). A superficial palmar arch was not formed (Fig. 2a). By contrast, the deep palmar arch, which was nourished by the radial artery after this vessel had passed the first metacarpal space was well developed. Three palmar metacarpal arteries took off from the deep palmar arch. The superficial palmar branch of the radial artery as well as the deep palmar branch of the ulnar artery were absent.
Diagram and photograph of arm 2 from a 80-year-old woman with a median artery not participating in the construction of the superficial palmar arch. (a) The median artery takes its origin from the common interosseous artery (1) and is gives off two radially located common digital palmar arteries (2). A superficial palmar arch is missing. (b) Near their origin, the median artery and the anterior interosseous artery run parallel. AIA anterior interosseous artery, BA brachial artery, CIA common interosseous artery, CPDAA common palmar digital arteries, MA median artery, MN median nerve, PIA posterior interosseous artery, PPDAA proper palmar digital arteries, PT-PP pronator teres (proximal part), PT-DP pronator teres (distal part), RA radial artery, RRA recurrent radial artery, SPA superficial palmar arch, UA ulnar artery
Left arm of a 75-year-old man with median artery involved in the construction of the superficial palmar arch
The median artery took off from the common interosseous artery (Fig. 3a, b). The median artery accompanied the median nerve, passed the carpal tunnel and entered into the formation of the superficial palmar arch at the level of the third intermetacarpal space. A topographical relation of the median artery to the anterior interosseous nerve was not observed. Median artery and ulnar artery together constructed the superficial palmar arch, which gave off four common palmar digital arteries (Fig. 3a). The superficial palmar branch of the radial artery was missing. The radial artery and the deep palmar branch of ulnar artery built the deep palmar arch. However, palmar metacarpal arteries deriving from the deep palmar arch were not detected.
Diagram and photograph of arm 3 from a 75-year-old man with a median artery involved in the construction of the superficial palmar arch. (a) The median artery derives from the common interosseous artery (1) and is connected with the superficial palmar arch (2). (b) The median artery, and the anterior and posterior interosseous arteries derive immediately from a short common interosseous artery. AIA anterior interosseous artery, BA brachial artery, CIA common interosseous artery, CPDAA common palmar digital arteries, MA median artery, MN median nerve, PIA posterior interosseous artery, PPDAA proper palmar digital arteries, PT-PP pronator teres (proximal part), PT-DP pronator teres (distal part), RA radial artery, RRA recurrent radial artery, SPA superficial palmar arch, UA ulnar artery
Right arm of a 78-year-old woman with median artery involved in the construction of the superficial palmar arch (not shown)
The median artery took off from the ulnar artery, just beneath the origin of the common interosseous artery. The common interosseous artery divided itself into the anterior interosseous artery, the posterior interosseous artery and the recurrent interosseous artery. The median artery followed the median nerve and gave off a branch for the second muscle belly of the flexor digitorum superficialis in the middle of the lower arm. The median artery and anterior interosseous nerve had no topographical relation to each other. After passing through the carpal tunnel together with the median nerve, the median artery connected itself with the superficial palmar branch of the ulnar artery forming the superficial palmar arch. The superficial palmar branch of the radial artery was missing. The medial part (median artery) of the superficial palmar arch formed the common palmar digital artery for the second and third finger, while the lateral part (ulnar artery) gave off two common palmar digital arteries for the third, fourth and fifth finger. The deep palmar arch was formed equally by the deep branches of the radial and ulnar arteries. Four palmar metacarpal arteries were derived from it.
Discussion
Quain [42] was the first author to describe the median artery as early as 1844. A small artery (arteria plicae cubiti superficialis) deriving from the brachial artery in the cubital fossa was named arteria mediana antebrachii superficialis, if it joined the course of the median nerve. In the four cases reported here, the median artery were derived twice from the ulnar artery and twice from the common interosseous artery. The median artery normally is a branch of the common interosseous artery [1, 28] or the anterior interosseous artery [25]. In some cases, the median artery took off from the ulnar artery or the brachial artery [25]. According to Adachi [1], the median artery originated from the ulnar artery in one-third of all cases. Gozdziewski [14] observed a superficially located median artery descending from the arteria brachialis, superior to the cubital fossa. An extraordinary case concerning the origin of the median artery was reported by Pabst and Lippert [40]: The axillary artery divided itself into arteriae brachialis superficialis and profunda. Below the cubital fossa, the arteria brachialis profunda again split itself into a typical common interosseous artery and a median artery. In a rare case, the median artery arose from the radial artery, proximal to the radial artery passing around the brachialis [54].
In 1813, Gantzer [21] described accessory heads of the flexor pollicis longus. In arm 1 described here, the median artery together with the median nerve crossed over an additional head of flexor digitorum pollicis (Gantzer-muscle).
The diameter of the median artery varied between 1.5 and 2.0 mm (Table 1). Libersa et al. [31] measured the external diameter of the median artery at the distal rim of the flexor retinaculum. The authors obtained values between 0.8 and 2.5 mm. Luschka [33] described a median artery of diameter 2.33 mm, supplying the second and third finger. In two patients suffering from carpal tunnel syndrome, the diameter of the median artery was found to measure 3.00 mm [11]. Overall, the diameters of the median arteries described here were medium sized.
The interosseous artery and the median artery as a branch of the common interosseous artery are seen first in the development of the human forelimb [48]. Afterwards, the ulnar artery arises from the brachial artery and the arteria brachialis superficialis develops in the axillary region. Later on, the median artery undergoes degeneration. Finally, an anastomotic branch between the brachial artery and the arteria brachialis superficialis becomes sufficiently enlarged to form the radial artery as a major artery of the forearm with the distal position of the latter. The proximal portion of the arteria brachialis superficialis atrophies correspondingly.
The median artery may persist in adults in two different patterns, i.e., a palmar and an antebrachial pattern [45]. The palmar pattern was studied in 120 cadavers and had an incidence of 20%. It was more frequent in females than in males. The antebrachial pattern was studied in 79 cadavers. With an incidence of 76%, it was also more common in females. In our sample, both sexes were represented equally. Kopuz et al. [26] found a median artery in neonates in 20% of the cases, while it was found in 17% in a combined study of neonates and adults. The authors suggested that the median artery perhaps atrophies at a later age, possibly during the perinatal and early infancy period. In 112 human embryos, a palmar pattern of the median arteries was observed in 18.7% [44].
An extremely rare doubling of the median artery was reported by Maruyama [34] in a Japanese individual. The first median artery was derived from the arteria antebrachialis (corresponding to the common interosseous artery) and the second one took off from the arteria antebrachialis volaris superficialis (corresponding to the ulnar artery). Both vessels run with the median nerve. In context with the above reported embryonic development of the median artery, Adachi [1] mentioned the case of a 39-year-old man. He possessed a strongly developed median artery, while the radial artery had degenerated, with a diameter of 2 mm only. Lanz and Wachsmuth [28] mentioned that a larger-than-normal median artery can be accompanied by an atrophied radial artery. The statement of Coleman and Anson [6] saying that the supplying part of the radial artery to the superficial palmar arch can be replaced by the median artery points in the same direction. By contrast, in the four cases of a strongly developed median artery reported here, the radial artery was expressed quite normally with proximal diameters between 3 and 5.5 mm and distal ones between 3 and 4 mm (Table 1).
The incidence of a median artery may be influenced by racial differences. In a sample of 60 neonates and infants from black communities, a median artery was found in 50% [13]. In samples of black and European South Africans, the median artery had a high incidence of 27.1 and 27.4%, respectively [18, 19]. In our sample, the frequency of the median artery reached 7.4% only.
A lot of clinical disorders can result from the expression of a strongly developed median artery and its variable relation to the median nerve. First of all, the median artery can cause carpal tunnel syndrome [56]. There have been sporadic surgical case reports of the hand in which a large patent median artery caused a carpal tunnel syndrome [4, 8, 10, 29, 30, 35, 43]. Furthermore, the carpal tunnel syndrome can rarely be caused by a thrombosed median artery [3, 5, 9, 23, 24, 38, 46, 53]. Also an aneurysm of a persistent median artery [52, 55] or a calcified median artery [7] can be followed by carpal tunnel syndrome. Balakrishnan et al. [2] reported a case with thrombosis of the median artery caused by a blunt trauma. Kele et al. [23] mentioned a rare case of a patient with carpal tunnel syndrome and thrombosed median artery. Here, pain in the third and fourth finger was recorded as an atypical complaint. In all the cases where a carpal tunnel syndrome was caused by thrombosis of a persistent median artery, symptoms arose suddenly and excision was needed [9]. However, the median artery can only be excised when a sufficient anastomotic blood supply is ensured [10]. Therefore, in the cases reported here, we have described the expression and the external diameters of other forearm arteries (Table 1).
Secondly, an anterior interosseous nerve syndrome can be caused by a median artery passing through this nerve, near its origin from the median nerve just below the elbow [41]. This syndrome is mainly characterized by paralysis of the flexor pollicis longus. In the cases described here, the median artery was not in the neighborhood of the anterior interosseous nerve.
Finally, the median artery can perforate or split the median nerve. Here, we have shown a median artery, which was perforating the median nerve in the upper third of the forearm, namely the part covered by the pronator teres (Fig. 1b). A pronator syndrome may be caused by a persistent median artery that passes through the proximal median nerve [22]. The authors reported about a “double crush” compression of the median nerve caused by persistent median artery producing first a carpal tunnel syndrome and then a pronator syndrome. In 2 of 134 forearms of Indians, the median artery splits the median nerve into two roots and the artery passes through the nerve [49]. Also Sanudo et al. [47] reported about a case where the median nerve split into unequal trunks to enclose the most proximal part of the median artery. Krol et al. [27] described a case where the median nerve, associated with a persistent median artery, was split 45 mm before the carpal tunnel.
Altogether, we can agree with the advice given by Gutowski et al. [16] that surgeons should be aware of additional structures, specifically more than one median nerve, when a persistent median artery is detected. A high bifurcation of the median nerve can be associated with a median artery [16].
References
Adachi B (1928) Das Arteriensystem der Japaner. Band I: A. pulmonalis, Aorta - Arcus volaris profundus. Maruzen, Kyoto, pp 308– 315
Balakrishnan C, Smith MF, Puri P (1999) Acute carpal tunnel syndrome from thrombosed persistent median artery. J Emerg Med 17:437–439
Barfred T, Hojlund AP, Berheussen K (1985) Median artery in carpal tunnel syndrome. J Hand Surg (Am) 10:864–867
Boles DM, Tobias PV, Spiro F (1982) Carpal tunnel syndrome due to compression by an anomalous median artery. Surg Neurol 17:99–100
Burnham PJ (1963) Acute carpal tunnel syndrome. Median artery thrombosis as cause. Arch Surg 87:645–646
Coleman SS, Anson BJ (1961) Arterial patterns in the hand based upon a study of 650 specimens. Surg Gynecol Obstet 113:409–424
Dickinson JC, Kleinert JM (1991) Acute carpal-tunnel syndrome caused by a calcified median artery. A case report. J Bone Joint Surg Am 73:610–611
Feldkamp MM, Gentili F, Hudson AR, Guha A (1995) A persistent median artery causing carpal tunnel syndrome in a patient with chronic renal failure: case report. Neurosurgery 37:140–143
Fumiere E, Dugardeyn C, Roquet ME, et al (2002) US demonstration of a thrombosed persistent median artery in carpal tunnel syndrome. JBR-BTR 85:1–3
Galassi E, Benfenati A, Tognetti F, Pozzati E (1980) Persistence of the median artery: possible cause of the carpal tunnel syndrome. Riv Neurol 50:159–166
Gassner EM, Schocke M, Peer S, et al (2002) Persistent median artery in the carpal tunnel. Color Doppler ultrasonographic findings. J Ultrasound Med 21:455–461
Gegenbaur C (1892) Lehrbuch der Anatomie des Menschen. 2. Bd. Engelmann, Leipzig, pp 259–265
George BJ, Henneberg M (1996) High frequency of the median artery of the forearm in South African newborns and infants. S Afr Med J 86:175–176
Gozdziewski S (1978) Variation of the axial arteries of the upper extremity in man. Folia morphol (Warszawa) 37:91–97
Gray DJ (1945) Some variations appearing in the dissection room. Stanford Med Bull 3:120
Gutowski KA, Olivier WA, Mehrara BJ, et al (2000) Arteriovenous malformation of a persistent median artery with a bifurcated nerve. Plast Reconstr Surg 106:1336–1339
Henle J (1868) Handbuch der systematischen Anatomie des Menschen. 3. Bd., 1. Abtlg.: Gefässlehre. Vieweg und Sohn, Braunschweig, pp 270–278
Henneberg M, George BJ (1992a) High incidence of the median artery of the forearm in a sample of recent Southern African cadavers. J Anat 180:185–188
Henneberg M, George BJ (1992b) A further study of the high incidence of the median artery of the forearm in Southern Africa. J Anat 181:151–154
Hofmann CEE (1878) Lehrbuch der Anatomie des Menschen. 2. Bd: Gefässsystem, Nervensystem und Sinnesorgane. Besold, Erlangen, p 139
Jones M, Abrahams PH, Sanudo JR, Campillo M (1997) Incidence and morphology of accessory heads of flexor pollicis longus and flexor digitorum profundus (Gantzer`s muscles). J Anat 191:451–455
Jones NF, Ming NL (1988) Persistent median artery as a cause of pronator syndrome. J Hand Surg (Am) 13:728–732
Kele H, Verheggen R, Reimers CD (2002) Carpal tunnel syndrome caused by thrombosis of the median artery: the importance of high-resolution ultrasonography for diagnosis. Case report. J Neurosurg 97:471–473
Khashaba A (2002) Carpal tunnel syndrome from thrombosed persistent median artery. J Emerg 22:55–57
Kopsch F (1914) Rauber-Kopsch: Rauber’s Lehrbuch der Anatomie des Menschen. Abteilung 3: Muskeln, Gefäße. Thieme, Leipzig, p 327
Kopuz C, Baris S, Gulman B (1997) A further morphological study of the persistent median artery in neonatal cadavers. Surg Radiol Anat 19:403–406
Krol A, Palczak A, Jedrzejewski KS (2005) Split median nerve. A report of two cases. Folia Morphol (Warszawa) 64:341–344
Lanz T von, Wachsmuth W (1959) Praktische Anatomie. Erster Band, dritter Teil: Arm. Springer, Berlin, pp 189, 200, 216
Lavey EB, Pearl RM (1981) Patent median artery as a cause of carpal tunnel syndrome. Ann Plast Surg 7:236–238
Levy M, Pauker M (1978) Carpal tunnel syndrome due to thrombosed persisting median artery. A case report. Hand 10:65–68
Libersa C, Francke JP, Mauppin JM, et al (1982) The arterial supply to the palm of the hand (arteriae palmae manus). Anat Clin 4:33–45
Lippert H, Pabst R (1985) Arterial variations in man. Bergmann, München, pp 71–77
Luschka H von (1865) Die Anatomie des Menschen. Dritter Band, erste Abtheilung: Die Glieder. Laupp’sche Buchhandlung, Tübingen, p 220
Maruyama K (1944) Seltene Varietät der Arterien der oberen Extremität bei einem Japaner (A. brachialis superficialis lateralis inferior, A. antebrachialis superficialis mediano-ulnaris, Arcus volaris superficialis vom Typus medianoulnaris). Folia Anat Jpn 22:551–567
Mauersberger W, Meese W (1975) Carpal tunnel syndrome caused by the persistence of the median artery. Neurochirurgia (Stuttgart) 18:15–19
Meckel JF (1816) Handbuch der menschlichen Anatomie. Zweiter Band: Besondere Anatomie. Gefäß- und Nervenlehre. Buchhandlung des Hallischen Waisenhauses, Halle
Michelsen H, Posner MA (2002) Medical history of carpal tunnel syndrome. Hand Clin 18:257–268
Nather A, Chacha PB, Lim P (1980) Acute carpal tunnel syndrome secondary to thrombosis of a persistent median artery (with high division of the median nerve). A case report. Ann Acad Med Singapore 9:118–121
Olave E, Prates JC, Gabrielli C, Pardi P (1997) Median artery and superficial palmar branch of the radial artery in the carpal tunnel. Scand J Plast Reconstr Hand Surg 31:13–16
Pabst R, Lippert H (1968) Beiderseitiges Vorkommen von A. brachialis superficialis, A. ulnaris superficialis und A. mediana. Anat Anz 123:223–226
Proudman TW, Menz PW (1992) An anomaly of the median artery associated with the anterior interosseous nerve syndrome. J Hand Surg (Br) 17:507–509
Quain R (1844) Anatomy of the arteries of the human body. Taylor & Walton, London, pp 235–271
Rayan GM (1986) Persistent median artery and compression neuropathy. Orthop Rev 15:241–244
Rodríguez-Niedenführ M, Burton GJ, Deu J, Sanudo JR (2001) Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat 199:407–417
Rodríguez-Niedenführ M, Sanudo JR, Vázquez T, Nearn L, Logan B, Parkin I (1999) Median artery revisited. J Anat 195:57–63
Rose RE (1995) Acute carpal tunnel syndrome secondary to thrombosis of a persistent median artery. West Indian Med J 44:32–33
Sanudo JR, Chikwe J, Evans SE (1994) Anomalous pattern of median nerve associated with persistent median artery. J Anat 185:447–451
Singer E (1933) Embryological pattern persisting in the arteries of the arm. Anat Rec 55:403–409
Srivastava SK, Pande BS (1990) Anomalous pattern of median artery in the forearm of Indians. Acta Anatomica 138:193–194
Steinke H, Esche M, Schmidt W (2004) Mehrfachvarietäten der Handarterien. Ann Anat 186:375–377
Tandler J (1897) Zur Anatomie der Arterien der Hand. Anat Hefte 7:263–282
Toranto IR (1989) Aneurysm of the median artery causing recurrent carpal tunnel syndrome and anatomic review. Plast Reconstr Surg 84:510–512
Wilhelm K, Feldmeier C (1975) Seltene Genese eines Karpaltunnelsyndroms. Münch Med Wschr 117:161–162
Wood SJ, Abrahams PH, Sanudo JR, Ferreira BJ (1997) Bilateral superficial radial artery at the wrist associated with a radial origin of a unilateral median artery. J Anat 189:691–693
Wright C, MacFarlane I (1994) Aneurysm of the median artery causing carpal tunnel syndrome. Aust N Z J Surg 64:66–67
Zeiss J, Guilliam-Haidet L (1993) MR demonstration of a persistent median artery in carpal tunnel syndrome. J Comput Assist Tomogr 17:482–484
Acknowledgments
We would like to thank Mrs. S. Widmer for the final preparation of the arterial variations in the forearms and Mr. G. Ritschel for the excellent drawings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Claassen, H., Schmitt, O. & Wree, A. Large patent median arteries and their relation to the superficial palmar arch with respect to history, size consideration and clinic consequences. Surg Radiol Anat 30, 57–63 (2008). https://doi.org/10.1007/s00276-007-0290-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-007-0290-5