Abstract
The aim of this study was to present anatomic macroscopic aspects and the relationship between the duodenum and the posterior abdominal wall. The authors describe anatomic types of peritoneal duodenal fossae and stress some points of surgical importance. Twenty-four cadavers, fixed in formalin, were dissected. Ten peritoneal fossae were given prominence and the authors show the anatomical structures topographically, from a superficial plane to a deep viscerae level. There is usually a complete fusion of the duodenal loop with the posterior parietal peritoneum except the duodenojejunal flexure. The study reveals three right retroduodenal fossae, three left retroduodenal fossae, two inferior duodenal fossae, one left paraduodenal fossa and one superior duodenal fossa. These peritoneal recesses mostly result from an incomplete adhesion of the Treitz’s fascia. This work provides some explanation of paraduodenal hernias that represent a rare case of intestinal obstruction. Two cases of these internal hernias are illustrated and their pathophysiology and embryologic basis are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The duodenum loop belongs to the peritoneal cavity. It extends from the first to the fourth lumbar vertebra and lies on the ventral face of the column “like a bag on a miller’s back”. However, if the duodenum does not adhere to the posterior parietal peritoneum, it adheres to the peritoneal fossae sometimes. We also studied the relationship between the duodenum and the posterior abdominal wall and highlighted its clinical and surgical implications.
Materials and methods
The peritoneal cavities of 24 cadavers were dissected. The cadavers had previously been embalmed in a formalin solution (a mixture of 10% formalin and ethanol). The anterior abdominal wall was incised with a vertical opening resembling a laparatomy. The greater omentum was suspended and the small intestine loops isolated. The liver was removed. A macroscopic analysis of the duodenal area was then performed. An anterior or anterolateral position was chosen.
Results
The dissection revealed three right retroduodenal fossae, three left retroduodenal fossae, two inferior duodenal fossae, one left paraduodenal fossa and one superior duodenal fossa. These fossae extend as far as the second and the third lumbar vertebra. Their height is about 7 cm and their depth in a sagittal plane is about 1–2 cm.
The duodenojejunal flexure appears movable and a semilunar avascular inferior duodenal fold delimits the entrance to these fossae: left paraduodenal fossa under the bridge formed by vessels; left retroduodenal fossae behind the fourth (ascending) portion of the duodenum, inferior duodenal fossa under that fold in the vicinity of the ascending branch of the left colic artery; and superior duodenal fossa under the Treitz’s vascular arch (Fig. 1).
Anterior view of the duodenojejunal flexure. JL jejunal loop, DJF duodenojejunal flexure, D4 fourth (ascending) portion of the duodenum, IDF inferior duodenal fold, TVA Treitz’s vascular arch, M mesentery, paraduodenal fossa (→), left retroduodenal fossa (←), inferior duodenal fossa (↓), superior duodenal fossa (↑)
If the second (descending) part of the duodenum does not lean against the posterior parietal peritoneum, we can discover a right retroduodenal fossa between the head of pancreas ventrally and the inferior vena cava dorsally and the psoas major muscle overlayed with parietal peritoneum. Above and below the recess, the superior genu and the inferior genu are bent across by two right folds, which are very thin on a frontal plane. These avascular folds are involved in the duodenal loop anchorage (Fig. 2).
The abdominal aorta and the inferior vena cava can be visible through the transparent parietal peritoneum. In that dissection, we can view a right inferior fold more widespread and thickened with a sagittal orientation (Fig. 3).
Right anterolateral view. D2 second (descending) portion of the duodenum, AA abdominal aorta, RPS right paracolic gutter, AC ascending colon, EA epiploic appendices, IG inferior genu, RIF right inferior fold, D3 third portion of the duodenum, D1 first portion of the duodenum, D2 second (descending) portion of the duodenum, SG superior genu, right retroduodenal fossa (✧)
The right inferior fossa continues below the third (horizontal) portion of the duodenum. The hepatoduodenal ligament arises at the flexure between the duodenal bulb and the descending part and reaches the gallbladder. It can clearly participate in the existence of an inferior recess because of its traction. This ligament can extend towards the visceral peritoneum causing a new gutter under the inferior genu (Fig. 4).
Sometimes the left retroduodenal fossa consists of a bridge formed caudally by the inferior duodenal fold and cranially by the superior duodenal fold. That recess is enhanced by a lumbar overlordosis (Fig. 5).
Discussion
Peritoneal fossae are usually caused by a non-adhesion between the posterior parietal peritoneum and the abdominal posterior wall between the 5th and the 11th week of gestation. These various recesses have been reported to occur in 68 and 48% cases of inferior and superior duodenal fossae, respectively, and coexist in 30%, with a 1% incidence of paraduodenal and retroduodenal fossae [19].
The retroduodenal fossae are related to partial failure of coalescence of the mesoduodenum to the posterior parietal peritoneum. Viscerae can also be dissimulated between either the posterior face of the fourth duodenum and the descending colon with Toldt’s fascia on the left side or the posterior face of the second duodenum and the ascending colon with Toldt’s fascia on the right side. We can note a thinning of Treitz’s fascia behind the duodenal loop (Fig. 6).
Horizontal section at L2. RTF right Toldt’s fascia, AC ascending colon, SMA superior mesenteric, D2 second (descending) portion of the duodenum, D4 fourth (ascending) portion of the duodenum, SMV superior mesenteric vessels, LSI loops of small intestine, TF Treitz’s fascia, IMA inferior mesenteric artery, LTF left Toldt’s fascia, DC descending colon, PP parietal peritoneum, VP visceral peritoneum, right retroduodenal fossa (✧), left retroduodenal fossa (✦)
The mesenterico-parietal fossa or inferior duodenojejunal is located under the superior mesenteric artery that runs in the superior pole of the mesentery between the duodenum on the ventral side and the posterior parietal peritoneum on the dorsal side. (Fig. 7) [1, 6, 8, 16, 25].
Midsagittal section. AA abdominal aorta, TF Treitz’s fascia, SMA superior mesenteric artery, P pancreas, PP parietal peritoneum, VP visceral peritoneum, LSI loops of small intestine, D1 first portion of the duodenum, D3 third (horizontal) portion of the duodenum, TC transverse colon, M mesentery, TM transverse mesocolon, inferior duodenal fossa (✧)
The paraduodenal fossa of Landzert is located lateral to the fourth segment of the duodenum and posterior to the inferior mesenteric vein and ascending branch of the left colic artery just beneath the posterior parietal peritoneum. These vessels raise serosal folds leading to venous and arterial paraduodenal fossae [11–13]. This fossa of Landzert is a fold seen in 1–2% of autopsies [10, 19, 20]. In addition the left superior duodenal fossa can be divided into two parts; the first horizontal segment interposed in the place below the root of the transverse mesocolon and the superior face of the duodenojejunal flexure; the second vertical part is located between the posterior face of the duodenojejunal flexure and the posterior parietal peritoneum raised by the vessels with a curve with ventral concavity (Fig. 8).
Parasagittal section through the left fossae. LCA left colic artery (ascending branch), SV splenic vein, IMV inferior mesenteric vein, TF Treitz’s fascia, D4 fourth (ascending) portion of the duodenum, TM transverse mesocolon, TC transverse colon, GO greater omentum, GEV gastroepiploic vessels, RM root of mesentery, CP corpus of pancreas, IPV inferior pancreatic vessels, DJF duodenojejunal flexure, PP parietal peritoneum, VP visceral peritoneum, SMD suspensory muscle of duodenum (Treitz’s muscle), LRV left renal vessels, LOV left ovarian vessels, GFN genitofemoral nerve, U ureter, PMM psoas major muscle, TPL3 transverse process of L3, PA pyloric antrum, left inferior fossa (✦), left superior fossa (✧), arterial fossa (✩), venous fossa (★)
These peritoneal fossae can be joined due to a scoliosis of the lumbar column. Thus they give rise to an abnormal “duodeno-aorto-spinal” fossa with unusual left lateroduodenal aortic position leading to a trapezoid space bordered by the fourth portion of the duodenum on the right and the abdominal aorta on the left [3].
The etiology of herniation into duodenal fossae is not well known and remains controversial and debatable. There are two main theories about the etiology of paraduodenal hernia. The first theory suggests that hernia was acquired by the gradual enlargement of an existing fossa. That mechanical theory states that increased intra-abdominal pressure (caused by peristaltismal undulations) forces loops of small intestine into pouches where fusion has not been completed [11, 12, 16, 23]. The second theory is related to anomalous rotation of the midgut between the 5th and 11th week of gestation and is a rare congenital anomaly. The midgut gets trapped in the mesentery of the proximal segment of the hindgut and as this descends to the right lower quadrant, a sac of peritoneum is formed to contain the small bowel to the right of the duodenum. There is, therefore, no possibility for the fusion of the ascending mesocolon to the posterior parietal peritoneum. A small hiatus, however, may admit a few loops of small bowel to the true peritoneal cavity and thereby constitutes a right paraduodenal hernia. On the other side, left paraduodenal hernias result on patients with paraduodenal hernia is progressive abdominal pain with epigastric cramps, bloating after meals. They often reduce spontaneously, leading to diagnostic difficulties [2, 4, 7, 9, 10, 14, 17, 19, 20, 24]. Paraduodenal hernias account for 0.2–0.9% of small bowel obstructions [10]. Males are affected twice as much as females [9, 20]. The average age at the time of occurrence is 38.5 years. The incidence of hernia on the left side is much more common than the right side, with the former accounting for 75% of the hernia cases [10]. To make from rotation of the midgut to the colic branches of the inferior mesenteric artery dorsally instead of ventrally, thereby allowing invagination into the mesocolon [2, 7, 15, 20].
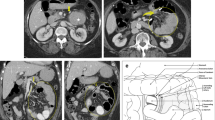
The clinical manifestations at diagnosis, radiological studies (with barium) and CT scan are essential. The upper gastrointestinal series show a characteristic pattern of bunched-up small bowel, as if it were contained in a bag [22, 26]. The CT scan reveals a cluster of dilated loops behind the pancreas, contrasted against the psoas muscles [18, 21]. Once diagnosed, these hernias should be treated. The operation should aim at a reduction of the incarcerated loops and an obliteration of the sac by conventional laparatomy [4, 5, 14] or by laparoscopic repair [24]. Care must be taken to preserve vessels during the surgical correction.
To illustrate this anatomic study, we reported two cases of paraduodenal hernias. The first was a left paraduodenal hernia of a 66-year-old man who complained of abdominal pain and vomiting. The CT scan was consistent with this diagnosis (Fig. 9). The patient underwent a laparotomy. Postoperative course was uneventful. The second patient was a 39-year-old man with the same symptomatology. The diagnosis of a right paraduodenal hernia was confirmed by the Roentgenogram after barium meal (Fig. 10). The treatment was a surgical reduction. Postoperative course went smoothly.
Horizontal CT scan at level L2 showing a left paraduodenal hernia. Note that the abdominal aorta and the inferior vena cava (arrowheads) are displaced on the right side, forming in this case a new space. Then, a small bowel loop gets trapped (curved arrow). SMV superior mesenteric vessels, P pancreas, DL dilated loops
Conclusion
These anatomic data enable a better understanding of the intestinal pathology in this area. These hernias have a paranormal orifice and lack their sac; hence they are named “internal prolapses or procidentia” [9]. These unusual internal hernias must be known and recognized by an uninitiated surgeon, as transmesenteric hernia, paracaecal hernias, transomental hernias, etc., [9, 17]. This diagnosis should be born in mind, particularly in the case of intestinal obstruction, especially in young patients who have not had previous abdominal surgery or external herniae.
References
Ancel P, Cavaillon P (1907) Recherche sur la morphogénèse du péritoine duodénal. Bibliogr Anatomique Tome XVI:73–96
Andrews E (1923) Duodenal hernia, a misnomer. Surg Gynecol Obstet 37:740–750
Barberini F, Carone VS, Caggiati A, Macchiarelli G, Correr S (1999) An usual peritoneal fossa: anatomic report and clinical implications. Surg Radiol Anat 21:287–291
Bartlett MK, Wang C, Williams WH (1968) The surgical management of paraduodenal hernia. Ann Surg 168:249–254
Bringham RA, Fallon WF, Saunders JR, Harmon JW, d’Avis JC (1984) Paraduodenal hernia: diagnosis and surgical management. Surgery 96:498–502
Broesike G (1891) Uber intra-abdominale (retro-peritoneale) Hernien und Bauchfelltaschen, nebst einer Darstellung der Entwicklung peritoneler Formationen. Fischer, Berlin
Callander CL, Rusk GY, Nemir A (1935) Mechanism, symptoms, and treatment of hernia into descending colon (left duodenal hernia); plea for change in nomenclature. Surg Gynecol Obstet 60:1052–1071
Gruber W (1868) Nachträge zu den Bildungshemmungen der Mesenterien und zu der Hernia interna mesogastrica überhaupt; und Abhandlung eines Falles mit einem Mesenterium, etc. Virchow’s Arch Path Anat 44:215–241
Gullino D, Giordano O, Gullino E (1993) Internal hernia of the abdomen. A propos of 14 cases. J Chir 130:179–195
Isabel L, Birrell S, Patkin M (1995) Paraduodenal hernia. Aust N Z J Surg 65:64–66
Jonnesco T (1890) Hernies internes rétro-péritonéales. Masson, Paris, pp 39–59
Jonnesco T (1895) Tube digestif. In: Poirier P (ed) Traité d’anatomie humaine, tome IV. Bataille, Paris
Landzert (without name) (1871) Uber die Hernie retroperitonealis (Treitz)und ihre Beziehungen zur Fossa duodeno-jejunalis. St Petersb Med Ztschr n F 2:306–350 (quoted by Parsons)
Manji R, Warnlock CL (2001) Left paraduodenal hernia: an unusual cause of small bowel obstruction. Can J Surg 44:455–457
Meyers MA (1970) Paraduodenal hernias. Radiologic and arteriographic diagnosis. Radiology 95:29–37
Moynihan BGA (1889) Duodenal folds and fossae. In: On retroperitoneal hernia, Chap 2. Baillière, Tindall Cox, London, pp 19–70
Newsom BD, Kukora JS (1986) Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg 152:279–285
Passas V, Karavias D, Grilias D, Birbas A (1986) Computer tomography of the left paraduodenal hernia. J Comput Assist Tomogr 10:542–543
Pistacchi E (1967) Studio anatomico-clinico sulle cosiddette ernie addominali interne. Minerva Chir 22:511–526
Rastogi A, Laplante S (1997) Right paraduodenal hernia. Can Assoc Radiol J 48:205–207
Rubinstein WA, Auh YH, Zirinsky K, Kneeland JB, Whalen JP, Kazam E (1985) Posterior peritoneal recesses: assessment using CT. Radiology 156:461–468
Taylor J (1930) The X-ray diagnosis of right paraduodenal hernia. Br J Surg 17:639–640
Treitz W (1857) Hernia retroperitonealis. Ein Beitrag zur Geschichte inneren Hernien. FA Credner, Prague
Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, Oguri H (1998) Laparoscopic repair of paraduodenal hernia. Surg Endoc 12:50–52
Waldeyer W (1874) Hernia retroperitonealis, nebst Bemerkungen zur Anatomie des Peritoneums. Arch Path Anat 60:66–92
Williams AJ (1952) Roentgen diagnosis of intra-abdominal hernia. An evaluation of the roentgen findings. Radiology 59:817–825
Acknowledgements
The authors would like to thank Mr. Mitch Donzelot for assistance with the figures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peltier, J., Gars, D.L., Page, C. et al. The duodenal fossae: anatomic study and clinical correlations. Surg Radiol Anat 27, 303–307 (2005). https://doi.org/10.1007/s00276-005-0332-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-005-0332-9