Abstract
Although there have been some reports that measured the size of mastoid pneumatization, only a few studies have reported the age-related variations in the mastoid air cell system using three-dimensional (3D) reconstruction techniques of computed tomography (CT) images. We performed a retrospective, cross-sectional study. A 3D reconstruction based on CT images was performed on 199 ears of 102 patients (age range 6–84 years) without otologic disease by a surface-rendering algorithm. The results showed that mastoid pneumatization continued to grow until the third decade. Thereafter, it declined slowly, and then rapidly after the seventh decade. No statistically significant difference was found between male and female or between right and left sides. There was a significant difference between the larger and smaller sides of individuals. The volume measurement technique based on the 3D reconstruction technique reported here is widely available, highly accurate and easy to perform.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Most land-living mammals have an aeration system in which the middle ear cleft is widened into a tympanic bulla. In addition, some species have an aeration system in which the middle ear cleft extends into the temporal bone as a complex system composed of numerous air cell tracts [9].This mastoid air cell system is highly developed in humans.
The temporal bone has a pyramidal shape, in which the air cell system extends variably to all regions within. The size of mastoid pneumatization varies considerably between individuals, and its development changes with age. There have been many reports on the measurement of mastoid pneumatization [1, 4, 6, 7, 8, 10, 11, 13, 14, 16]. However, although all air cells are interconnected, it is very difficult to access their volume directly. It is for this reason that radiological methods are most widely employed.
Many three-dimensional (3D) computer-based image reconstruction and analysis techniques have been developed as computer technology has advanced. These new methods make it possible to measure the volume of mastoid pneumatization. There have been a few reports that have described the volume of mastoid pneumatization as well as its value in use [7, 8, 16]. However, there is no report showing how mastoid pneumatization changes with age.
In this study, we focused on the application of 3D computer-based volume measurement and strove to arrive at as accurate volume as possible after measuring a large number of temporal bones, so that we would be confident that a correct normal distribution over age would be achieved.
Materials and methods
Among the paranasal sinus (PNS) computed tomography (CT) scans taken in our department of otolaryngology-head and neck surgery in the last 3 years, those that showed negative findings about the sinonasal tract were chosen. The medical records of these patients were reviewed for the following exclusion criteria: a past history of middle ear surgery, a history of otitis media, a perforated tympanic membrane, or a sclerotic or atrophic tympanic membrane. Any patients not excluded on the above criteria but who showed findings compatible with chronic otitis media and/or mastoiditis on CT, such as a soft tissue mass found in the middle ear cleft or the mastoid with or without bone erosion of ossicles or surrounding temporal bones, opacification of multiple mastoid air cells, or demineralization of trabeculae with coalescence, were also excluded. The PNS CT scans of 199 ears from 102 healthy subjects aged between 6 and 84 years were selected. Fifty patients were male and 52 were female.
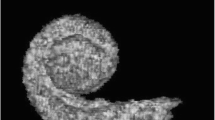
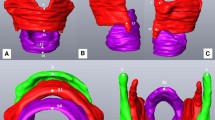
The acquisition parameters applied to the most commonly used protocols are follows. The PNS CT scans were taken with a 2.5 mm slice thickness, 140 kV, 120 mAs, and continuous non-overlapping sections. After the imaging data had been stored in a DICOM (Digital Imaging and Communication in Medicine) file, they were imported to a personal computer running Vworks 4.0 software (Cybermed, Seoul, Korea). When reconstructed using a surface-rendering algorithm, the selection of the window thresholds is critical for making an accurate volume measurement. Setting the upper threshold too high includes the soft tissues in the mastoid, resulting in an overestimation of the volume of mastoid pneumatization. In contrast, too low an upper threshold excludes some of the air cells, resulting in an underestimation of the volume of mastoid pneumatization. In this study, a lower threshold of –1,024 Hounsfield units (HU) and an arbitrary upper threshold of –200 HU were used to represent the air cells only. The volume of mastoid pneumatization was automatically calculated by 3D reconstruction of the mastoid air cell system (Fig. 1).
In order to compare the means between the two sexes, statistical analysis was done with ANCOVA (analysis of covariance). In order to compare the right and left mastoids and to evaluate the difference between the two sides, a paired t-test was done. All statistical analyses were performed using SPSS software (SPSS, Chicago, IL), and a p value <0.05 was considered significant.
Results
In Korean adults (19–44 years old), the mean volume of the mastoid pneumatization was 7,095.2 mm3. The distribution of the volumes according to age group is shown in Table 1. The results show that the volume of mastoid pneumatization increases rapidly from birth until early in the second decade. Thereafter, the growth in size continues at a slow rate, reaching a maximum in the third decade. After the third decade, there is a tendency for a slow reduction in volume, and the volume rapidly decreases from late in the seventh decade (Fig. 2).
This study did not show any statistically significant difference between male and female (p=0.318). Interestingly, the growth of female mastoid pneumatization was more rapid than that in males. In addition, a tendency for the decrease in the volume of female mastoid pneumatization to begin earlier than that in males was shown in this study (Fig. 3).
There were 100 patients who had normal CT findings of both temporal bones. There was no significant difference between the right and left sides (p=0.125). However, there was a statistically significant difference between the larger and smaller sides in individuals (p<0.05).
Discussion
Although interest in the temporal bone and the ear can be traced back to Hippocrates, scientific and systematic studies of the mastoid air cell system were first reported by Diamant [5], who showed that the average size of a normal adolescent’s mastoid is 12.07 cm2 and that the development of the mastoid air cell system is completed by the age of 15 years in males and 10 years in females.
The mastoid air cell system has been well documented as an air reservoir for the middle ear and its volume is believed to govern the capacity of that reservoir. Although little is known regarding the physiologic functions of the mastoid air cell system, it has been suggested that it serves to protect the sensitive inner ear structures from external temperature changes. In addition, it plays an important role as a pressure regulator by virtue of the large surface area with respect to gas exchange [2, 12]. Therefore, it is reasonable that the degree of mastoid pneumatization plays an important role in its function. The status of the middle ear cavity is dependent on the function of the mastoid air cell system and the degree of the mastoid pneumatization is closely correlated with its function, and so it is essential to determine the pneumatization of the mastoid air cell system to understand the physiology or explain the pathophysiology of the middle ear/mastoid disease.
There is a considerable variation in the size of mastoid pneumatization between individuals, and the development of mastoid pneumatization changes with age. When planning this study, it was a dilemma how interindividual variation could be controlled. To control for this, pairwise comparisons are needed over time to detect changes in the size with age. This, of course, would take an entire career of all subjects to measure, and would seem to be impossible in practice. Because this study was designed as a cross-sectional study, there may be some errors resulting from interindividual variation. Two hypotheses for the variations between individuals have been proposed [2]. The first is that the degree of mastoid pneumatization is genetically determined. The second is that the size of mastoid pneumatization is determined by the degree of pathologic involvement of the middle ear during childhood. In general, the latter appears to be accepted [15]. It was the latter hypothesis that legitimizes this study. As the degree of pathologic involvement of the middle ear during childhood affects the development of mastoid pneumatization, so the degree of pathologic involvement during life may influence the size of mastoid pneumatization with age.
There have been many reports regarding the measurement of the size of mastoid pneumatization. Of the reports in which the size of mastoid pneumatization has been measured quantitatively, several methods such as a water-weight method [13], a pressurized transducer method [1] and an acoustic method [10] have been utilized. However, with the development of radiological tools, many methods that are capable of measuring the volume of the mastoid pneumatization have been developed [4, 6, 7, 8, 11, 14, 16]. The temporal bone has a pyramidal shape and an air cell system that extends variably to all regions within it. The mastoid air cells surround the centrally located structures of the inner ear, and have a wide and irregular shape. Although all air cells are interconnected, it is very difficult to assess the size of mastoid pneumatization directly. This is the reason why radiological methods are most widely employed. However, earlier radiological methods could measure only the 2D size (such as the area) of mastoid pneumatization. Later methods have attempted to measure the volume (3D size) of mastoid pneumatization using 2D images, but these methods have a limitation in that it is not clear how close the estimated value is to the actual volume [4, 14].
A 3D computer-based image reconstruction and analysis technique has been developed that, with advances in computer technology, can be performed using a personal computer. This new method makes it possible to reconstruct a 3D model of the middle and inner ears, as well as to measure the area or volume of various structures in the ear. Because volume measurement in three dimensions is theoretically more accurate and has become easier to perform with the advances in computer hardware and software, it is possible to reconstruct the CT images in three dimensions and to measure the length, area, volume and angle, even on a personal computer.
Both volume- and surface-rendering algorithms have been used for many medical purposes, such as the production of educational tools, surgical planning and guidance tasks. Each algorithm has its advantages and disadvantages, some of which are well known. For medical purposes, a volume-rendering algorithm is preferred because of its ability to contain the data of the internal architecture, to give a texture to the density changes in the data, to allow easy and natural exploration of volumetric data, and to exclude the need for classifying or segmenting the data. One of the main sources of error in volume rendering is “partial voluming”. This occurs when the voxels ostensibly represent multiple tissues of different kinds. The disadvantages of a surface-rendering algorithm are: it discards the interior of the object and maintains the object’s shell; it does not facilitate real-world operations such as cutting, slicing or dissection; and it does not enable artificial viewing modes, such as semi-transparency.
The method of data acquisition should use the highest resolution for the most accurate survey of the mastoid air cell system. However, one acquisition parameter, the height of the scan field, of those applied to the most commonly used protocols for temporal bone CT is problematic. When temporal CT is undertaken, the slice thickness is 1 mm and the height of the scan field is 25–30 mm. This height of the scan field is too small to contain all the mastoid air cells, and some air cells of the sinodural angle and digastric ridge are lost, particularly the well-pneumatized temporal bone. This is one of the reasons why this study used PNS CT instead of temporal CT. Also, there may be another difference in the volume calculations which might result from the use of different protocols for image acquisition. When PNS CT is used for volume measurements instead of temporal CT, one disadvantage is an error resulting from the slice thickness. Therefore, we think that there is a need for further studies to reduce the slice thickness of PNS CT or to extend the height of the scan field of temporal CT. Another reason why this study used PNS CT instead of temporal CT is that the indication for CT scanning may also influence the results. Most patients who underwent temporal CT at our hospital had many otologic problems, such as chronic otitis media, atelectatic otitis media, cholesteatoma and temporal bone fracture. These conditions are known to reduce the volume of mastoid pneumatization. Thus, scans must be done to exclude those with these conditions. We think that patients undergoing PNS CT are more representative of the general population than those undergoing temporal CT. In addition, in contrast to head or brain CT, there was no doubt that patients undergoing PNS CT would be examined by an otolaryngologist at least once. Therefore, even in a retrospective study, it is possible to exclude those who had a past history of middle ear surgery, a history of otitis media or a perforated tympanic membrane.
There have been many reports that have measured the volume, not the size, of the adult mastoid pneumatization (Table 2). However, these reports did not mention the age of the study group. To our knowledge, there has been only one report in the literature that evaluated the size variation of mastoid pneumatization with age [3]. In this study Chatterjee et al. [3] evaluated the 2D size, not the volume, of mastoid pneumatization using a radiographic planimetric method.
In this study, the mean volume of the adult mastoid pneumatization was 7,095.2 mm3. This result is similar to previous reports (Table 2). It could also be seen that the growth in the volume of mastoid pneumatization was rapid up to the early second decade and then slowed down until the third decade. It was found that there was a tendency for a slow reduction in the volume until the seventh decade. Thereafter, the volume of mastoid pneumatization was reduced rapidly. These findings are similar to a previous report [3]. Since this study was a cross-sectional study, not longitudinal, the tendency for a reduction in the degree of the mastoid pneumatization with age might not be due entirely to aging. Considering that the generation currently in their seventh to ninth decade were born around the time of World War II and the Korean war (1950–1953), we think that this tendency may be due to poor nutrition, poor health condition, and poor medical services without appropriate antibiotics and hospital treatment.
The volume of mastoid pneumatization did not differ significantly between the sexes (p=0.318). There was no significant difference between the right and left sides (p=0.125). However, when a larger volume was compared with a smaller one, there was a significant difference between the two sides (p<0.05).
It is well known that a poorly pneumatized mastoid is linked with chronic middle ear disease, but we also know that normal ventilation can be possible in ears with small mastoid pneumatization. What, then, is the size of healthy mastoid pneumatization? Is there any variation in the size of healthy mastoid pneumatization with age? The importance of the method used in this study is its high accuracy and ease of use. We hope that our study will contribute to the gathering of further physiologic data on the aeration mechanism of the middle ear and help in establishing a general theory for it.
Conclusion
In this study based on the volume measurement of mastoid pneumatization using 3D reconstruction of CT images, the mean volume of mastoid pneumatization was 7,095.2 mm3 in Korean adults. In evaluating the volume of mastoid pneumatization, high-resolution CT is the best method. In addition, 3D image reconstruction and measurement by the volume-rendering technique must be used to measure temporal bone/mastoid pneumatization for the best results. From this study, we conclude that it is useful to measure the volume of mastoid pneumatization using a 3D reconstruction of PNS CT images. We also hope that this study will provide baseline data for further studies on mastoid pneumatization.
References
Andreasson L, Mortensson W (1975) Comparison between the area and the volume of the air filled ear space. Acta Radio 16:347–352
Austin DF (1977) On the function of the mastoid. Otolaryngol Clin North Am 10:541–547
Chatterjee D, Ghosh TB, Ghosh BB (1990) Size variation of mastoid air cell system in Indian people at different age groups: a radiographic planimetric study. J Laryngol Otol 104:603–605
Colhoun EN, O’Neill G, Francis KR, Hayward C (1988) A comparison between area and volume measurements of the mastoid air spaces in normal temporal bones. Clin Otolaryngol 13:59–63
Diamant M (1940) Otitis and pneumatization of mastoid bone. Acta Otolaryngol 41:10
Isono M, Murata K, Azuma H, Ishikawa M, Ito A (1999) Computerized assessment of the mastoid air cell system. Auris Nasus Larynx 26:139–145
Koc A, Ekinci G, Bilgili AM, Akpinar IN, Yakut H, Han T (2003) Evaluation of the mastoid air cell system by high resolution computed tomography: three-dimensional multiplanar volume rendering technique. J Laryngol Otol 117:595–598
Luntz M, Malatskey S, Tan M, Bar-Meir E, Ruimi D (2001) Volume of mastoid pneumatization: three-dimensional reconstruction with ultrahigh-resolution computed tomography. Ann Otol Rhinol Laryngol 110:486–490
Magnuson B (2003) Functions of the mastoid cell system: auto-regulation of temperature and gas pressure. J Laryngol Otol 117:99–103
Molvaer OI, Vallersnes FM, Kringlebotn M (1978) The size of the middle ear and the mastoid air cell system measured by an acoustic method. Acta Otolaryngol 85:24–32
Park MS, Yoo SH, Lee DH (2000) Measurement of surface area in human mastoid air cell system. J Laryngol Otol 114:93–96
Sade J (1992) The correlation of middle ear aeration with mastoid pneumatization. The mastoid as a pressure buffer. Eur Arch Otorhinolaryngol 249:301–304
Silbiger H (1950) Über das Ausmass der Mastoid Pneumatisation beim Menschen. Acta Anat 11:215–223
Todd NW, Pitts RB, Braun IF, Heindel H (1987) Mastoid size determined with lateral radiographs and computerized tomography. Acta Otolaryngol 103:226–231
Tos M, Stangerup SE (1985) The causes of asymmetry of the mastoid air cell system. Acta Otolaryngol 99:564–570
Vrabec JT, Champion SW, Gomez JD, Johnson RF Jr, Chaljub G (2002) 3D CT imaging method for measuring temporal bone aeration. Acta Otolaryngol 122:831–835
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, DH., Jun, BC., Kim, DG. et al. Volume variation of mastoid pneumatization in different age groups: a study by three-dimensional reconstruction based on computed tomography images. Surg Radiol Anat 27, 37–42 (2005). https://doi.org/10.1007/s00276-004-0274-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-004-0274-7