Abstract
Purpose
To retrospectively analyse complications in endovascular aortic repair (EVAR) interventions and evaluate if the CIRSE (Cardiovascular and Interventional Radiological Society of Europe) complication classification system is appropriate as a standardized classification tool for EVAR patients.
Materials and Methods
Demographic, procedural and complication data in 719 consecutive patients undergoing EVAR at one institution from January 2014 to October 2019 were retrospectively reviewed. Data (imaging reports, procedural reports, nurse notes, discharge summary reports) were collected consulting the electronic patient record system (EPR) of the hospital and cleaned and stored in a Microsoft Excel database. All the procedures were analysed in consensus by two interventional radiology consultants and a resident radiologist and if an intra- , peri- or post-procedural complication occurred, a grade (1–6) was assigned using the CIRSE grading complication classification system.
Results
Twenty-five patients were excluded from the analysis because of invalid or incomplete data. The final population was made up of 694 patients (mean age 75,4 y.o., 616 male/78 female, min age 23 y.o., max age 97 y.o.). Complications emerged in 211 patients (30,4% of cases, 22 female/189 male). The number of patients with CIRSE grade I, II, III, IV, V and VI complications was 36 (17%), 17 (8%), 121 (57,3%), 15 (7,1%), 3 (1,4%), 19 (9%). Nineteen (2,6%) patients succumbed after EVAR. Thirty-four complications (16,1%) were related to vascular access.
Conclusion
The CIRSE complication classification system represents a broadly applicable and feasible approach to evaluate the severity of complications in patients following EVAR. However, some deficit may be considered relevant and as starting standing-point for future improvements.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The limited literature exists on standardised reporting systems to evaluate EVAR complications. Moreover, a lack of agreement on the definition of complications and their severity hampers the comparison of different outcomes. As for many other kinds of surgery or intervention, most reports use term such as “minor”, “moderate” and “severe”, but they are subjective, unreliable and often inconsistently used among different authors and centres [1]. Some authors use a simple distinction in minor and major events whilst others employ the Complex Severity Index (CSI) in order to stratify the complications [2, 3]. This lack of uniform reporting throughout different practitioners results in a series of disadvantages to compare results over different time periods within the same institution, within different institutions and even for different treatments. Outcome data for the therapeutic techniques such as for the EVAR are strategically evaluated, and an accurate complication reporting system is necessary [4].
In order to standardize the complication reporting, some classifications have been developed, introduced and validated [5,6,7,8]. In the field of interventional radiology, the CIRSE Standards of Practice committee introduced in 2017 the CIRSE complication classification system. The classification system allows the evaluation of the safety of the procedures, comparison of different approaches and internal quality control to improve management and prevention of complications [9].
To our knowledge, the CIRSE complication classification system has not been reported in the literature in the assessment of EVAR complications. In our opinion, it may represent an appropriate choice in the analysis of the outcome in the EVAR scenario. The main aim of this study is to retrospectively analyse complications in EVAR interventions and evaluate if the CIRSE complication classification system is appropriate as a standardized classification tool for EVAR patients.
Materials and Methods
A retrospective analysis was conducted on all patients who underwent EVAR at our institution between January 2014 and October 2019, providing almost 6 years of consecutive data. All patient data (demographic data, sex, age, imaging reports, procedural reports, nurse notes, discharge summary reports, follow-up notes) were retrospectively extracted and reviewed consulting the electronic patient record system (EPR) of the hospital (Epic eHospital platform, Verona, WI, the USA). Data were cleaned and stored in a Microsoft Excel database. All the EVAR procedures were analysed and reviewed by two interventional radiologists and a resident radiologist and if an intra-, peri- or post-procedural complication occurred, a grade (1–6) was assigned in consensus using the CIRSE complication classification system.
The data of the present study were collected in the course of common clinical practice, and accordingly, the signed informed consent obtained from each patient authorized also for research study purposes. The study protocol conforms to the ethical guidelines of the "World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004.
Complication’s Assessment and Grading
The CIRSE complication classification system takes into account intra-, peri- and post-procedure complications and uses a grading scale 1 to 6 where grade “1” is assigned to a complication that may be solved within the procedure operative session without additional therapy, sequelae or deviation from the normal post-therapeutic course, and “6” is assigned in case of death (Fig. 1). The grading was assigned by a radiologist in training and two trained interventional radiologists. In case of ambiguity of assignment, a consensus between the examiners was requested. Special attention was paid to the analysis of endoleak type II because it represents a common event in EVAR interventions. In our analysis, we decided to consider the endoleak type II a complication only in case it was the cause of aneurysm sac enlargement requiring reinterventions. The presence of hematoma at the access site was carefully evaluated, and it was considered a complication if caused a delay in discharge or reintervention.
CIRSE complication classification system grading [9]
Procedure and Follow-Up Details
Elective and emergency procedures were performed and included in the retrospective analysis. All elective cases were discussed in a multidisciplinary team (MDT) meeting with the interventional vascular radiologists, vascular surgeons, anaesthesiologists and clinicians. The procedures were performed by interventional radiologists with experience ranging from 5 to 20 years. The procedures were performed in a Hybrid EVAR theatre, equipped with a fully motorized C arm (Artis Zeego, Siemens Healthcare GmbH, Erlangen, Germany) or in angio-theatre with a fixed imaging system (Artis Zee, Siemens Healthcare GmbH, Erlangen, Germany). Percutaneous access was performed whenever possible in all patients with suitable iliofemoral anatomy (defined by normal location of the CFA bifurcation at least 2 cm below the inguinal ligament with no evidence of calcification in the anterior arterial wall or the presence of minimal calcification affecting 50% of the posterior arterial wall). The choice of technique for femoral access was at the discretion of the treating physician. Surgical access via femoral cut-down was deemed necessary and performed in case of hostile iliofemoral anatomy. In case of percutaneous access, the “preclosure technique” with Perclose Proglide (Abbott Laboratories, Abbott Park, Illinois, the USA) was used [10].
Post-operatively, patients were monitored with clinical and laboratory examinations. Post-operative surveillance followed an institution's standard EVAR surveillance protocol in line with recommendations by the European Society for Vascular Surgery [11]. We included patients with a minimum follow-up of 3 months and at least 1 imaging follow-up exam. In particular, the availability of data of 1 CT/MR follow-up study was considered an essential inclusion criterion. Due the complexity of the procedure, we decided to consider both early (< 30 days) and late complications. Patients were followed up until the end of the study period, death, emigration, or if controls were ended either by the patient or medical team.
Statistical Analysis
Data were collected and analysed using a combination of Excel (Version 2010, Microsoft, Redmond) and SPSS (Version 23, IBM Corp, Armonk, NY). Descriptive statistics were reported as number (percentage) or mean (standard deviation), as appropriate. Continuous variables were compared using the Chi-square test and Mann– Whitney U test. P values less than 0.05 were considered statistically significant and p values less than 0.01 highly statistically significant.
Results
In the period between January 2014 and October 2019, 719 consecutive EVAR and emergency TEVAR cases were performed in our institution (included Fenestrated -EVAR and Branched-EVAR). Based on the EPR consultation, 25 procedures were excluded from the analysis because of incomplete data (21 patients were excluded because data were corrupted or not complete, this fact is mainly due to fallacious digitalisation of documents, and in order to easy the revision and uniform the criteria of analysis, we decided to include only patients without problem of data recording; four patients excluded because did not fulfil follow-up data inclusion criteria). Descriptive data of the final population are summarized in Table 1.
Uncertainty of grade assignment was rare, just in 13/694 cases (1,87%), the researchers were doubtful about the interpretation of the complication and its grading according to CIRSE complication classification system. In four cases, the revision of the data excluded the event may be considered a complication; in 1 case, the grade was confirmed; in 1 case, the grading was lowered (3 to 1 CIRSE grade); in 7 cases, the grade of the complication was increased. The final grade assignment according to CIRSE classification is reported in Fig. 2.
Overall Mortality Causes
The main cause of death was perioperative bleeding from a ruptured aneurysm (6 cases). In one case, it was a late complication due to endoleak type 2. Two procedures were converted to open repair due to the intraoperative bleeding but without success. kindly post-operative respiratory failure and pneumonia were encountered in four patients as the leading causes of death. From the revision of the perioperative and surgical notes, Nellix (Endologix Inc., Irvine, CA, the USA) device failure (pressurisation of the sac and caudal migration) was the cause of death in 3 cases. Other causes are reported in Table 2.
Emergency and Elective Repair
In the period of analysis, 18 emergent procedures were performed. We encountered 16 complications in this cohort study (16/18, 88,8%), with an overall mortality rate of 38,8% (7/18). Data of complication grade assignment in elective and emergent EVAR procedures are represented in Fig. 3.
Complications Details
CIRSE grade 3, 4 and 5 grade complications occurred in 139/211 patients (66%). The most common CIRSE grade complication encountered was grade 3 and the analysis of the complications made year by year demonstrates this trend (Fig. 4). The group of complications graded as CIRSE 3 is widely heterogeneous. Looking to the causes of complications, we observed serious risky situations just like acute emergent limb ischemia but also recovery-related errors (example—wrong diet in a patient with celiac disease that caused gastro-intestinal discomfort and delayed discharge). Based on the analysis of the complication rate made year by year, we noticed the trend-rate goes from 44.18% in 2018 to the minimum of 17.74% in 2017. The trend of the complication rate year by year shows a not-constant incidence. This fluctuation appears to be time-wise related to some changes in our interventional radiology unit (staff member discontinuity, angio-theatre renovations transition, new protocol flowchart introduction), but it also could be part of a cyclic incidence fluctuation we are not able to demonstrate (Fig. 5). Thanks to the standardized method of evaluation of complications, we were able to stratify complications causes on the bases of CIRSE grade assignation (Table 2).
Access-site-related complications were the commonest complication encountered in the different categories. A total of 34 complications were access-site related (16.1% of complications, 4.9% of procedures). The CIRSE complication grade assigned in these cases ranged from 1 to 4 (Fig. 6).
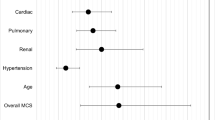
The review of the EPRs about access-site-related complications showed the presence of a seroma as the most common complication encountered (10 cases). The presence of a seroma leads to simple adjunctive surveillance in most of the cases, but in 3 cases, the excessive discomfort and extension caused new treatment/procedure or readmission. Other causes of access-site-related complication are reported in Table 3. Based on the analysis of the complications in the subgroups of patients ≥ 80 y.o. and patients < 80 y.o., the use of the Mann–Whitney U test testified no statistical difference in complications grade assignment (p = 0,85) (Fig. 7).
Discussion
A uniform, simple and reproducible system, like the CIRSE complication classification system, would permit comparison of outcomes between surgical procedures and between different institutions and allow for knowledge transfer for improvement in one’s institution. The implications are wide-ranging as all disciplines would be empowered to work toward the same goal of improving surgical in-patient outcomes [12]. In our analysis, the use of CIRSE classification system filled the gap of the lack of an objective grading system able to detect all kind of complications with a special focus on their outcome and the consequent sequelae in the EVAR scenario.
In our study, the evaluation of complications in EVAR procedures by using the CIRSE complication classification system resulted in an easy appliable method to detect, stratify and categorize intraoperative and post-operative complications. Its wide applicability is testified by the fact that no complications emerged as orphan of grade assignment and by the low rate of uncertainty grade assignment. The complication and the death rates encountered are in line with the results of the literature reports and testify the reliability of the study cohort [13,14,15,16]. As resulted by the rate of CIRSE grade 3 assigned, the need for reintervention and adjunctive therapy represents a common event after EVAR and it has a relevant impact on the outcome and costs of the procedure [17].
The use of the CIRSE classification system allowed to discriminate permanent sequelae following treatment, differentiating mild from severe ones. The use of the CIRSE classification system permitted an immediate detection of the rate of these cases and creation of a useful amount of data to be used by hospital managers, insurance companies and governments, in order to strategically plan their way to assess these events [4].
Our results support the findings of different papers that testify the efficacy and safety of EVAR in the octogenarian subgroup of patients as the evaluation of the mortality rate and grading assignment of complications demonstrated no differences in respect of a younger population [Fig. 7] [18, 19].
Our series highlighted the importance of vascular access care and management. In the literature, injury to access vessels has been reported to occur in up to 5%–17% of cases. These data are in keeping with our results [20,21,22]. In our institution, the policy of “percutaneous-first” (i.e.always percutaneous access if anatomically feasible in patients without hostile iliofemoral anatomy) was adopted during the study period. Several factors may be associated with access-site complications, including operator experience, vessel calcifications, obesity and large sheath size. The percutaneous access in EVAR procedures requires an adequate level of expertise in the evaluation and choice of puncture site and high-level technical skills. These aforementioned factors may be relevant also considering the learning curve and the scenario (University Hospital and training centre) and might have an impact on our results. However, no death or permanent severe sequelae (patients requiring ongoing assistance in daily life) due to access-site complications were detected in our series, but a relevant number of reinterventions or adjunctive therapy were encountered [Table 3, Fig. 6].
Moreover, the CIRSE complication classification system appears to be a useful and exhaustive tool to detect any kind of complications, including those that may happen during the interventions but that do not need any further management after the end of the treatment/procedure (CIRSE grade1). In fact, if it is true that the impact of this kind of complications could be marginal with regards to patient outcome, their impact might not be negligible taking into account analysis of possible comparison of different approaches, analysis of learning curves, procedural time and costs. In our series, they represent a consistent part of the overall complications (17%), and the possibility to detect and analyse their occurrence with the CIRSE complication classification system represents a strong favourable point to its routine use since other classification systems do not take into account them [5,6,7].
As EVAR treatment represents a major procedure, many variables should be considered. In the application of the classification, we were driven to some interpretative efforts, for example, in the grade assignment in case of open conversion. In these cases, we decided to consider the conversion to open repair as a grade 1 because deemed as a complication inherent the percutaneous approach resolved by the alternative surgical approach in the same operative session. Obviously, this fact conditions also the hospital stay, and we believed it would be linear to consider the prolonged hospital stays after the conversion as a grade 2 or 3 only if an open repair- related complication was noted. The recovery time may be strictly related to the initial performance status of the patient and conditions of repair and may impair the definitions of the prolonged stay so that we decided to consider normal a < 48 h of stay if after elective repair. > 48 h but less than 72 h of hospital stay has been considered grade 2 and grade 3 if > 72 h of stay.
In addition, as the complexity of the EVAR requires long follow-up and some complications may arise also years after (endoleak II in primis may be cause of reintervention), we decided could be reasonable to include early and late complication in the same group of analysis. Even if it is true that the definition of temporally associated complication has not to be diluted in time, it is also linear that the cause-effect relationship has not to be considered negligible. About this point, in the CIRSE complication classification system, there is no clear definition regarding the time-course and this may represent a confounding factor in the evaluation of results.
Another important point is represented by the fact that the CIRSE complication classification system does not distinguish between emergent and elective procedure and this may represent an evaluation confounding factor. In our study, we were able to analyse the elective and emergent cohort study, and as expected, in the emergent repair group, the complication rate and the death rate were dramatically higher than in the elective one. This differentiation could be relevant in the evaluation of outcome and its inclusion may represent a suggestion to improve the classification and categorization method in future.
We believe that the CIRSE complication classification system allows an unbiased evaluation of procedure care quality. In our context, the EPR system represented a precious tool because it permitted easy and detailed retrospective evaluation of patient data (imaging reports, procedural reports, laboratory tests, nurse notes, therapy diary, discharge summary reports, follow-up data).
The main limitation of this study is that even using the EPR system, some data may be missing or corrupted. We did not investigate interobserver reliability in the current study rather we attempted to eliminate any doubtful grade assignment by a consensus agreement between the researchers.
However, our dataset represents one of the biggest in the literature regarding EVAR and we believe that will provide a benchmark reference for future studies.
In conclusion, the CIRSE system of classifying complications provides a comprehensive and uniform platform for grading complications within complex contexts such as EVAR with the benefit of evaluating patients and hospital outcomes. The application of this grading system provides the opportunity to learn from and improve the treatment of complications and their management. However, some deficits have been encountered in our tool-applicability experience. In particular, the absence of clear distinction between early and late complication or between the emergency and elective procedure in the CIRSE classification complication system may confound the essence of the obtained results. These aspects may be considered as starting standing-point toward future improvements.
References
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2 (PMID: 19638912).
Gradinscak DJ, Young N, Jones Y, et al. Risks of outpatient angiography and interventional procedures: a prospective study. AJR Am J Roentgenol. 2004;183(2):377–81. https://doi.org/10.2214/ajr.183.2.1830377 (PMID: 15269028).
Noori VJ, Healey CT, Eldrup-Jorgensen J, et al. Comparison of major adverse event rates after elective endovascular aneurysm repair in New England using a novel measure of complication severity. J Vasc Surg. 2019;70(1):74–9. https://doi.org/10.1016/j.jvs.2018.10.055 (Epub 2018 Dec 28 PMID: 30598356).
Martin II RC, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235(6):803–13. https://doi.org/10.1097/00000658-200206000-00007 (PMID: 12035036; PMCID: PMC1422509).
Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250(2):177–86. https://doi.org/10.1097/SLA.0b013e3181afde41 (PMID: 19638919).
Hay JL, Atkinson TM, Reeve BB, et al. NCI PRO-CTCAE Study group. Cognitive interviewing of the US national cancer institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). Qual Life Res. 2014;23(1):257–69. https://doi.org/10.1007/s11136-013-0470-1 (Epub 2013 Jul 20. PMID: 23868457; PMCID: PMC3896507).
Khuri SF, Daley J, Henderson W, et al. The department of veterans affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA surgical quality improvement program. Ann Surg. 1998;228(4):491–507. https://doi.org/10.1097/00000658-199810000-00006 (PMID: 9790339; PMCID: PMC1191523).
Khalilzadeh O, Baerlocher MO, Shyn PB, et al. Proposal of a new adverse event classification by the society of interventional radiology standards of practice committeel. J Vasc Interv Radiol. 2017;28(10):1432-7.e3. https://doi.org/10.1016/j.jvir.2017.06.019 (Epub 2017 Jul 27. Erratum in: J Vasc Interv Radiol. 2018 Jan;29(1):146. PMID: 28757285).
Filippiadis DK, Binkert C, Pellerin O, et al. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017;40(8):1141–6. https://doi.org/10.1007/s00270-017-1703-4 (Epub 2017 Jun 5 PMID: 28584945).
Lee WA, Brown MP, Nelson PR, Huber TS. Total percutaneous access for endovascular aortic aneurysm repair (“preclose” technique). J Vasc Surg. 2007;45(6):1095–101. https://doi.org/10.1016/j.jvs.2007.01.050 (Epub 2007 Mar 29 PMID: 17398056).
Moll F, Powell J, Fraedrich G, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European Society for Vascular Surgery. Eur J Vasc Endovasc Surg. 2011;41(Suppl 1):S1-58. https://doi.org/10.1016/j.ejvs.2010.09.011 (PMID: 21215940).
Seely AJ, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg. 2010;90(3):936–42. https://doi.org/10.1016/j.athoracsur.2010.05.014 (PMID: 20732521).
De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1881–9. https://doi.org/10.1056/NEJMoa0909499 (PMID: 20484396).
Nordon IM, Karthikesalingam A, Hinchliffe RJ, et al. Secondary interventions following endovascular aneurysm repair (EVAR) and the enduring value of graft surveillance. Eur J Vasc Endovasc Surg. 2010;39(5):547–54. https://doi.org/10.1016/j.ejvs.2009.11.002 (Epub 2009 Nov 25 PMID: 19939711).
Baderkhan H, et al. Detection of late complications after endovascular abdominal aortic aneurysm repair and implications for follow up based on retrospective assessment of a two centre cohort. Eur J Vasc Endovasc Surg. 2020;60(2):171–9. https://doi.org/10.1016/j.ejvs.2020.02.021 (Epub 2020 Mar 21 PMID: 32209282).
Chaikof EL, Dalman RL, Eskandari MK, et al. The society for vascular surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67(1):2-77.e2. https://doi.org/10.1016/j.jvs.2017.10.044 (PMID: 29268916).
Stather PW, Sidloff D, Dattani N, et al. Systematic review and meta-analysis of the early and late outcomes of open and endovascular repair of abdominal aortic aneurysm. Br J Surg. 2013;100(7):863–72. https://doi.org/10.1002/bjs.9101 (Epub 2013 Mar 8 PMID: 23475697).
Fonseca R, Rockman C, Pitti A, et al. Intermediate-term EVAR outcomes in octogenarians. J Vasc Surg. 2010;52(3):556–60. https://doi.org/10.1016/j.jvs.2010.03.051.
Rueda-Ochoa OL, van Bakel P, Hoeks SE, et al. Survival After uncomplicated EVAR in octogenarians is similar to the general population of octogenarians without an abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2020;59(5):740–7. https://doi.org/10.1016/j.ejvs.2020.01.026 (Epub 2020 Feb 27 PMID: 32115359).
Murray D, Ghosh J, Khwaja N, et al. Access for endovascular aneurysm repair. J Endovasc Ther. 2006;13(6):754–61. https://doi.org/10.1583/06-1835.1 (PMID: 17154706).
Vatakencherry G, Molloy C, Sheth N, Liao M, Lam CK. Percutaneous access planning, techniques and considerations for endovascular aortic repair (EVAR). Cardiovasc Diagn Ther. 2018;8(Suppl 1):S184-90. https://doi.org/10.21037/cdt.2018.03.06.PMID:29850430;PMCID:PMC5949597.
Dwivedi K, Regi JM, Cleveland TJ, et al. Long-term evaluation of percutaneous groin access for EVAR. Cardiovasc Intervent Radiol. 2019;1:28–33. https://doi.org/10.1007/s00270-018-2072-3 (Epub 2018 Oct 4. PMID: 30288590; PMCID: PMC6267668).
Acknowledgements
These data were submitted as a manuscript and accepted for CIRSE 2020 in September
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Castiglione, D., Easwaran, A., Prashar, A. et al. Assessment of EVAR Complications using CIRSE Complication Classification System in the UK Tertiary Referral Centre: A ∼6-Year Retrospective Analysis (2014–2019). Cardiovasc Intervent Radiol 44, 1174–1183 (2021). https://doi.org/10.1007/s00270-021-02847-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-021-02847-9